Neuropsychiatric Presentation of Multiple Sclerosis
Multiple sclerosis (MS) is a degenerative disorder of the central nervous system occurring, in the United States, in approximately 6 to 50 per 100,000 persons.1 It commonly has a relapsing-remitting course.2 Although neuropsychiatric symptoms have been reported in MS since the time of Cruveilhier and Charcot, in the 1800s, this possibility is often overlooked in the differential diagnosis of patients with new-onset psychiatric symptoms.3 Slowed cognition, executive dysfunction, mania, depression, pathological crying, and personality changes have been reported in up to 66% of patients with MS and are, in many cases, the first symptoms for which the patient seeks medical attention.4,5 Recent studies link these symptoms to the anatomical disease and not to the stress of chronic illness.6,7
The classic histopathology of MS is characterized by demyelination and inflammation surrounding venules and extending into the myelin sheath.8 The infiltrating cells include T lymphocytes of predominantly the CD4 phenotype, activated macroglia, and plasma cells. Infiltration of these inflammatory cells and inflammatory cytokines produced in situ are directly associated with demyelination and plaque formation. The histopathologic features of MS lesions are suggestive of a myelin-directed autoimmune process.9
Currently, magnetic resonance imaging (MRI) is the most sensitive tool available to document lesions in patients with a clinical diagnosis of MS and to predict progression to MS in patients who present with optic neuritis. An excellent recent review has summarized the significance of MRI in diagnosis and management of MS.10 In brief, a combination of a T2-weighted MRI (for lesion identification) and a contrast-enhanced T1-weighted MRI (for detection of blood–brain barrier abnormality) is commonly used in clinical practice. The ability to track lesions over time using MRI can be very important in diagnosing MS. New enhancing lesions indicate probable MS.
Most MS lesions appear hyperintense on T2-weighted MRI, an appearance that is nonspecific for MS. Occasional MS lesions are hypointense on T2-weighted MRI, an appearance that has been attributed to the presence of nonheme iron deposition. Presence of multiple lesions, an ovoid shape, and periventricular location are considered characteristic of MS, as is involvement of the corpus callosum. However, attempts to correlate lesion load based on standard T2-weighted MRI with the clinical progression of MS have not been successful. Many patients have multiple lesions on MRI that are asymptomatic.
Newer MRI methods may further improve lesion detection. The fast spin echo (FSE) technique for acquiring T2-weighted MRI provides similar contrast but allows thinner sections that are contiguous. Addition of an inverting pulse (fluid-attenuated inversion recovery; FLAIR) to the T2-weighted MRI provides a heavily T2-weighted image in which the strong signal from cerebrospinal fluid (CSF) has been removed, allowing identification of MS lesions at the interfaces between CSF and brain. The combination of these two techniques (FSE-FLAIR) may be the best for detecting MS lesions, although not all studies agree.
MS lesions appear hypointense on T1-weighted MRI. There is evidence suggesting that lesions seen on T1-weighted MRI (sometimes referred to as “black holes”) correlate more closely to the degree of disability and disease progression than those seen on T2-weighted MRI. Lesions that enhance on T1-weighted MRI following administration of a contrast agent are considered likely to be active, and this appearance correlates with the presence of macrophage infiltration. However, the relationship between blood-brain barrier abnormality and active disease is still considered controversial. The number of lesions that enhance will depend to some extent on the MRI methods used. More lesions will enhance if a higher dose (usually triple the standard dose) of contrast agent is used, if there is a delay (generally 15–60 minutes) between contrast agent administration and MRI, or if magnetization transfer is used in addition to contrast agent in order to decrease the signal from normal tissue.
Magnetic resonance spectroscopy (MRS) is being used to study the chemistry of MS lesions. These lesions have lower levels of N-acetyl aspartate (NAA, a neuronal marker) than normal brain. NAA can also be decreased in areas without clearly identifiable lesions and may indicate presence of microscopic disease. There has been some success correlating changes in NAA with clinical disease classification, and it has been suggested that this may be a measure of axonal loss. Increased choline has been associated with enhancing lesions, whereas decreases may indicate chronic, nonenhancing plaques.
Some of the newer methods of acquiring or analyzing MRI may provide more information about the fundamental processes occurring in the tissue. Magnetization transfer MRI may be sensitive to structural change at the molecular level in MS. Analysis of the T2 decay curve may provide insight into structural changes within the myelin bilayer. An increase in the self-diffusion of water within MS plaques has been found by using diffusion-weighted MRI, but the increase did not correlate with disability. These are exciting research tools that may eventually lead to a clearer understanding of the pathophysiology of MS and to treatment guidelines and protocols.

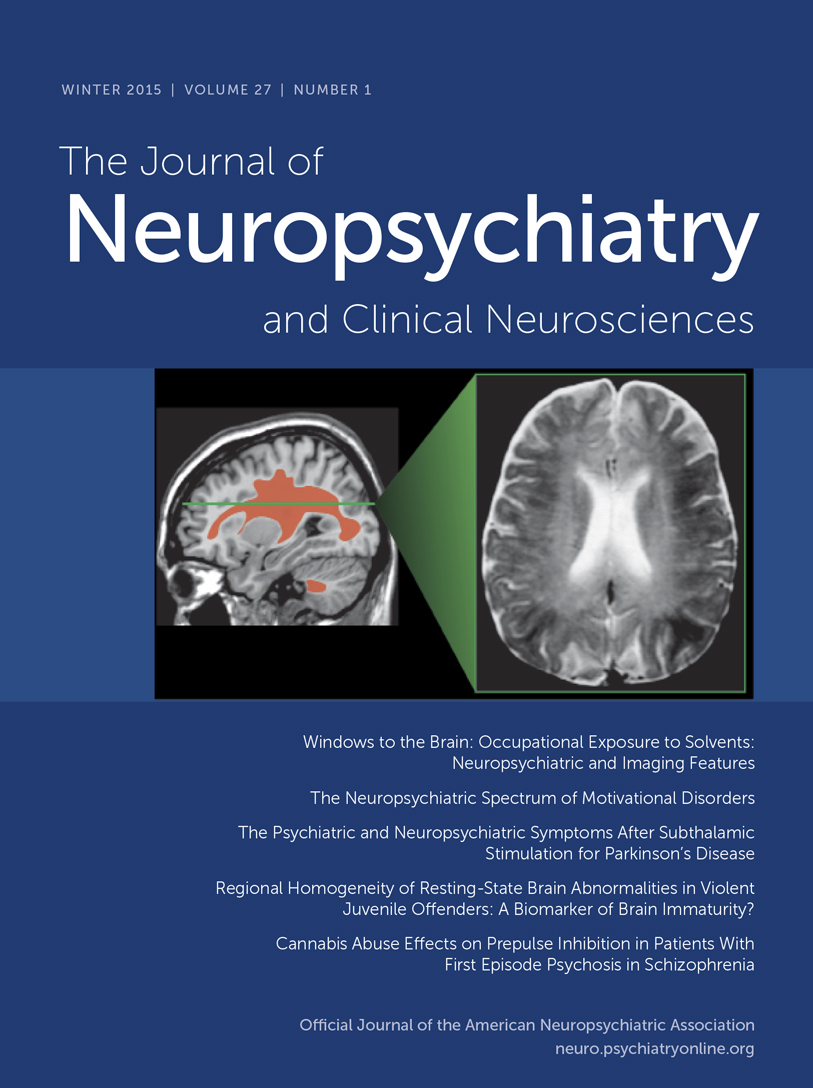
A. (left) T2-weighted axial magnetic resonance image of a 23-year-old woman with multiple sclerosis (MS). Note the characteristic ovoid high signal-intensity demyelinating lesions (arrows indicate the largest periventricular lesions). These are perpendicular to the cerebrospinal fluid (CSF)-filled spaces. Generalized brain atrophy is manifested by symmetric enlargement of the CSF spaces. The patient presented with a history of two past psychiatric hospitalizations (one at age 19 for mania and one at age 22 for depression), intractable insomnia, anxiety, depressed mood, suicidal ideas, bradykinesia, and bradyphrenia. She had none of the usual presenting symptoms of MS (i.e., visual disturbances, weakness, urinary or bowel incontinence, or swallowing and speaking difficulties). However, subsequent testing revealed classic findings of multiple sclerosis, including abnormal visual evoked potentials, positive CSF for oligoclonal bands, and an elevated immunoglobulin G synthesis and index rate. B. (right) Monoclonal antibody labeling of CD4+ T lymphocytes with fluorescent rhodamine staining (orange) of a postmortem MS brain specimen. These lymphocytes infiltrate the white matter of the central nervous system along the periventricular veins.
1 Rodgers J, Bland R: Psychiatric manifestations of multiple sclerosis: a review. Can J Psychiatry 1996; 41:441–445Crossref, Medline, Google Scholar
2 White RF: Emotional and cognitive correlates of multiple sclerosis. J Neuropsychiatry Clin Neurosci 1990; 2:422–428Link, Google Scholar
3 Finger S: A happy state of mind: a history of mild elation, denial of disability, optimism, and laughing in multiple sclerosis. Arch Neurol 1998; 55:241–250Crossref, Medline, Google Scholar
4 Stenager E, Knudsen L, Jensen K: Psychiatric and cognitive aspects of multiple sclerosis. Semin Neurol 1990; 10:254–261Crossref, Medline, Google Scholar
5 Beatty WW: Cognitive and emotional disturbances in multiple sclerosis. Neurol Clin 1993; 11:189–204Crossref, Medline, Google Scholar
6 Pujol J, Bello J, Deus J, et al: Lesions in the left arcuate fasciculus region and depressive symptoms in multiple sclerosis. Neurology 1997; 49:1105–1110Crossref, Medline, Google Scholar
7 Feinstein A: Depression associated with multiple sclerosis: an etiological conundrum. Can J Psychiatry 1995; 40:573–576Crossref, Medline, Google Scholar
8 Ffrench-Constant C: Pathogenesis of multiple sclerosis. Lancet 1994; 343:271–175Crossref, Medline, Google Scholar
9 Zhang J: Multiple sclerosis: perspectives on autoimmune pathology and prospect for therapy, in Current Neurology, edited by Appel S. St. Louis, MO, Mosby-Year Book, 1995, pp 115–155Google Scholar
10 Grossman RI, McGowan JC: Perspectives on multiple sclerosis. AJNR Am J Neuroradiol 1998; 19:1251–1265Medline, Google Scholar