Intellectual Functioning in Adolescents With Indicators of Psychosis: Evidence for Decline in Functioning Related to Number of Psychotic Features?
Abstract
Substantial research has demonstrated that adults with schizophrenia display intellectual decline compared to their premorbid levels of functioning. Research of this type, however, is not as common in adolescents with psychotic disorders. Since many first-episode adolescents with psychotic disorders other than schizophrenia may eventually meet criteria for this diagnosis, we examined first admission adolescents with variable psychiatric diagnoses. In this study, current intellectual functioning was compared to estimated premorbid functioning (estimated with word recognition reading), and the difference between these scores was related to the number of indicators of psychosis that was present in each case. Subjects consisted of 513 inpatients, ranging in age from 13 to 17 years, who were admitted to the adolescent service of a private psychiatric hospital. Indicators of psychosis came from clinical diagnoses, self-report measures, and clinical rating scales. Across the entire sample of 513 subjects the greater the number of indicators of psychosis that was present, the greater the estimated premorbid/current intelligence quotient (IQ) discrepancy. Type of IQ test, differences in intellectual premorbid functioning, demographic variables, and type of treatment were all unassociated with risk for IQ discrepancy. Within the limitations of estimation of premorbid intellectual functioning, these data suggest that intellectual decline is present at the time of the first psychiatric admission in psychotic adolescent patients who do not necessarily meet diagnostic criteria for schizophrenia and that this discrepancy is greater in patients with more indicators of psychosis.
The intellectual and cognitive deficits associated with schizophrenia have been well established over the past several decades of research in this area.1–3 First episode patients have clearly been shown to demonstrate substantial severity of overall cognitive impairments,4,5 and the profile of impairments is similar to those seen in patients with an extended history of illness.6 In addition, cognitive impairments seen early in the course of illness in patients with schizophrenia are more severe than those seen in patients with affective disorder, including those who are psychotic at the time of assessment.7 However, conflicting findings have emerged, with regard to the early course of neuropsychological impairments in this disease. While some researchers suggest that the influence of early developmental cognitive impairments completely precedes the onset of schizophrenia with no further intellectual decline, others have demonstrated cognitive and intellectual decline detectable immediately prior to the onset of illness.9,10 The question of general intellectual decline in schizophrenia is receiving more attention as demonstrated by the growing number of investigations addressing this issue. Numerous studies11,12 have found that patients with schizophrenia have evidence of intellectual decline compared to various estimates of premorbid functioning at the time of the first episode. An average discrepancy of approximately 10 points on average from estimated or measured premorbid levels of intellectual functioning in schizophrenics with an established course of illness has been reported.2,13
There has been less attention directed toward the neuropsychological abnormalities associated with other nonaffective psychotic disorders possibly related to schizophrenia (e.g., psychosis not otherwise specified, brief psychotic disorder). One exception is the study of Kremen et al.,14 who reported that intellectual decline between ages 4 and 7 was a risk factor for the development of later psychotic conditions. Furthermore, much of the research on cognitive decline has focused primarily on individuals with an adult onset (see Bedwell et al.11). Given the potential adverse consequences associated with early intellectual decline, particularly in adolescence or earlier, investigation of the cognitive correlates of childhood and adolescent onset psychosis is warranted. The purpose of this study is to examine the issue of potential intellectual decline in a group of first-episode psychotic adolescent inpatients with a diversity of clinical diagnoses.
Assessment of intellectual decline has typically involved comparing an individual’s current cognitive performance with the level of intellectual ability or potential before the onset of psychotic symptoms (i.e., premorbid IQ). Premorbid estimates of intelligence quotient (IQ) are widely used in clinical neuropsychology research and are based on the belief that some neuropsychological tests are relatively unaffected by the onset of brain dysfunction, psychosis, or mild dementia (i.e., hold tests). While there is the potential for error in any estimation of previous functioning, several studies15–19 have demonstrated the utility of reading and word pronunciation tests as an estimation of premorbid intellectual capacity, in healthy individuals, patients with dementia, patients with schizophrenia, and their relatives. Furthermore, some research20 has demonstrated that current oral word-reading ability and original intellectual function (i.e., premorbid full-scale IQ) are highly correlated, adding validity to the use of these estimates. As a result, these skills have commonly been used to provide an estimate of premorbid intellectual functioning.
Research on multiple populations has indicated that there are a variety of psychometric indicators that can be reliably used to identify mild psychotic experiences. For instance, scales of perceptual aberration and magical thinking have been used to identify individuals with subclinical psychotic phenomena (see Lenzenweger21 for a review). Individuals with deviant scores on these instruments have also been shown to have cognitive deficits on some,22 but not all,23 neuropsychological tests. High scorers on these instruments have also been shown to be at somewhat elevated risk for psychosis at follow up,24,25 although high scores on these scales are not specific to vulnerability to schizophrenia. In addition, some studies have also examined the usefulness of certain scales from structured personality and psychopathology inventories such as the Minnesota Multiphasic Personality Inventory (MMPI) for their ability to identify risk for later psychosis.26 It has even been suggested that subsets of MMPI items alone can identify individuals who are vulnerable to the development of schizophrenia.27 Thus, the use of self-report instruments to examine psychotic and subpsychotic phenomena may also be of use in examination of the correlates of psychosis, including intellectual decline.
In the present study, we identified a large sample of adolescent psychiatric admissions that varied in the number and severity of indicators of the presence of psychosis. These indicators came from self-report and observational data and included MMPI subscales, clinical ratings generated by therapists, and diagnoses generated by the treating psychiatrists. Current intellectual functioning was evaluated and a full-scale IQ was obtained, while reading achievement test scores were used to estimate previous intellectual functioning. The discrepancy between these scores was examined with respect to the number of psychotic indicators that were met in each case. The purpose of this study was to begin to answer the following questions:
Does intellectual decline, as indexed by discrepancies between estimated premorbid functioning and current intellectual performance, occur in psychotic disorders other than schizophrenia, particularly in adolescents who do not yet meet full criteria but may at a later time?
Are different levels of severity of symptoms in psychotic adolescents related to the extent of intellectual decline, as indexed by discrepancies between estimated premorbid functioning and current intellectual performance?
METHODS
Subjects
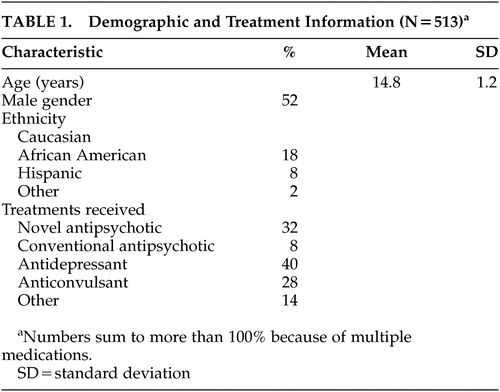
The study sample was comprised of consecutive inpatient referrals to the adolescent psychological assessment service of a private psychiatric hospital in Westchester County, New York during a 30-month period. About two-thirds of all adolescent admissions undergo psychological testing in order to assist with differential diagnosis, assessment of risk, treatment and/or discharge planning. Upon admission to the hospital, patients and their primary caregivers are informed that information from their records, including psychological test data, may be used for archival research under the guidelines of strict confidentiality, consequently, precluding the need for any additional consent form. This study, therefore, was performed on a strictly archival basis, and no direct contact with any patients, other than through their medical records, occurred. The hospital institutional review board approved this study on that basis. Patients with complete assessment data were considered for participation in the study (N=513). Descriptive information on these patients, including the proportions who received antipsychotic medications after treatment was initiated, is presented in Table 1.
Measures
Intelligence.
IQ scores were established for each subject via administration of age-appropriate Wechsler Intelligence Scales. The Wechsler Adult Intelligence Scale, 3rd ed. (WAIS-III) and Wechsler Intelligence Scale for Children, 3rd ed. are individually administered instruments for assessing intellectual abilities. All subjects also received the Wide-Range Achievement Test, 3rd ed. (WRAT-3) from which the reading subtest was used in order to obtain an estimate of premorbid intellectual level. The IQ estimate scores from this measure were used as an index of potential premorbid functional status.
Hopkins Psychiatric Rating Scale.
The Hopkins Psychiatric Rating Scale.28 was completed for all patients by their therapists. This scale contains 17 symptoms items and a global psychopathology measure. The global pathology measure is rated on a 9-point scale, while all of the individual symptom items are rated on a 7-point1–4 scale. There are two items on the Hopkins Psychiatric Rating Scale relevant to psychosis: conceptual disorganization and psychosis. Interrater reliability of the Hopkins Psychiatric Rating Scale was previously determined to have an interrater correlation coefficient (ICC) of 0.91 for the global score (comparing therapist raters to trained clinical raters) and an average ICC of 0.87 for the two psychosis items.29
MMPI-A.
This structured personality inventory examines a variety of aspects of psychopathology in a self-report format and is specifically normed for use with adolescents. Although there are multiple clinical scales, the two scales of interest for this report are the Bizarre Mentation and Schizophrenia scales. The Bizarre Mentation scale is a Content scale that was developed by Ben-Porath and Sherwood30 as a measure of psychotic thought processes. This includes the obvious symptoms of psychosis such as delusions and hallucinations as well as the less obvious such as odd and eccentric thoughts and experiences. Wetzler et al.31 report high positive predictive power for the Bizarre Mentation scale suggesting that it is a useful measure for detection of present psychotic processes. The Schizophrenia scale is an empirically derived measure that comprises one of the Clinical scales of the MMPI-2. Elevations on this scale are purported to reflect bizarre thought processes, peculiar perceptions, and experiences relating to the negative symptoms of schizophrenia.32
Summarizing the Indicators of Psychosis
In order to ascertain the presence of various signs of psychosis, a checklist procedure was employed. The checklist was based on information that was present in the patients’ medical charts and collected in the comprehensive assessments. The following served as indicators for the presence of psychosis: 1) chart discharge diagnosis of a psychotic condition; 2) MMPI-A bizarre thinking scale greater than a t score of 65; 3) MMPI-A schizophrenia scale greater than a t score of 65; 4) therapist rating score greater than or equal to 4 (moderate) on Hopkins Psychiatric Rating Scale for conceptual disorganization; and 5) therapist rating score greater than or equal to 4 (moderate) on Hopkins Psychiatric Rating Scale for psychosis.
RESULTS
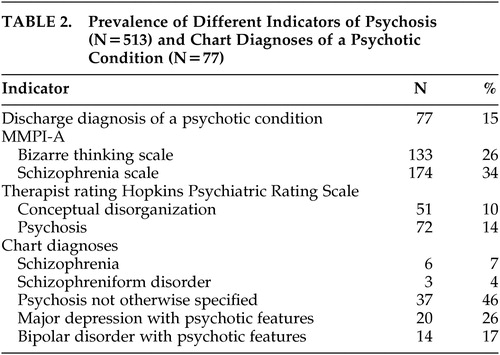
Table 2 lists the frequency of occurrence of the different indicators of psychosis in the sample as a whole on the top and the frequencies of the chart diagnoses of psychotic conditions on the bottom. As can be seen in the table, the MMPI indicators were more frequent than the clinical ratings of psychosis or a psychosis diagnosis.
In the first analyses of the data, difference scores between premorbid IQ as estimated by the WRAT-3 reading subtest and current full-scale IQ were calculated. First, these difference scores were compared across the sample of subjects who had from 0 to 5 of the indicators of psychosis, with the results of this comparison presented in Figure 1. A one-way analysis of variance (ANOVA) found a significant effect of number of indicators for the difference score of estimated premorbid IQ and current measured IQ (F=2.63, df=5, 508, p<0.05). Scheffé follow up tests found that subjects with five indicators of psychosis had a significantly (p<0.05) greater difference score than subjects with four indicators, while those individuals with four indicators had a significantly greater difference score than those with three indicators (p<0.05). There were no significant differences in discrepancy scores between participants who had three or fewer indicators present. In order to ensure that this pattern of differences was not due to differences in premorbid IQ scores, the same analysis was performed with WRAT-3 reading scores and full-scale IQ scores as well. The results of the analysis on the WRAT-3 were nonsignificant (F=1.64, df=5, 508, p>0.10), while the results of the ANOVA on full-scale IQ were statistically significant (F=5.77, df=5, 508, p<0.001). Thus, the pattern of discrepancy between full-scale IQ and WRAT-3-based IQ appears to be related to lower current full-scale IQs in the context of essentially no difference in the reading scores that were used to estimate premorbid functioning.
Following these analyses, the influences of potentially confounding variables were considered. Using a multiple regression analysis, age, gender, years of school completed, ethnicity, and whether or not the subject was receiving antipsychotic medications were examined for their influence on the relationship between number of indicators of psychosis and the IQ difference score described above. When the influence of number of indicators on IQ decline was examined, the overall regression was significant (F=9.86, df=1, 511, p<0.002, with the multiple R2=0.14). When the other demographic variables were entered into the equation, the analysis was still significant (F=8.18, df=6, 506, p<0.001). When the regression was repeated with a forward entry stepwise procedure, number of psychosis indicators entered the equation first, again accounting for 14% of the variance in the difference score, followed by gender which accounted for an additional 3% of the variance, and age, which accounted for 2% of the variance. Thus, although demographic variables are related to the discrepancy between current full-scale IQ and WRAT-3 IQ, they do not replace the number of indicators of psychosis as the best predictor of putative IQ decline. Medication status does not account for any variance in the discrepancy between current and estimated premorbid IQ.
Next, we attempted to identify the differential importance of the five different psychosis indicators for the prediction of discrepancies between current and estimated premorbid IQ. All were entered into a simultaneous regression analysis, predicting the IQ discrepancy, followed by a planned forward entry analysis. The simultaneous entry analysis was statistically significant (F=3.49, df=3, 509, p<0.02), and the forward entry procedure indicated that having a diagnosis of psychosis accounted for 8% of the variance (p<0.01), followed by the presence of a clinical rating of psychosis on the Hopkins Psychiatric Rating Scale (3.5%) (p<0.05), followed by the bizarre thinking score from the MMPI A (2.5%) (p<0.05). Thus, aspects of both the clinical ratings of psychosis and psychometric data added information beyond that obtained from the presence of a psychotic diagnosis.
An additional analysis was performed in order to determine if the specific Wechsler IQ test employed influenced the results in any meaningful way. We used t tests and compared the full-scale IQ, WRAT-3 reading score, and the discrepancy between the two across the type of IQ test administered for the entire sample. No significant differences were found (all t<1.23, df=512, all p>0.10).
Finally, in order to tentatively examine whether affective and nonaffective psychotic diagnoses were associated with any differences in the IQ variables, we compared these same three dependent variables across the groups of chart diagnoses. This analysis collapsed the diagnoses into broad categories of affective psychosis diagnoses (major depression with psychotic features and bipolar disorder with psychotic features) and nonaffective psychosis diagnoses (schizophrenia, schizophreniform, and psychosis not otherwise specified). Again, t tests found no significant differences on any of the variables (all t<1.68, df=78, all p>0.05).
DISCUSSION
These findings demonstrated a statistically significant discrepancy between estimated premorbid levels of cognitive functioning and current IQ that was correlated with the number of indicators of psychosis present in a large sample of adolescent psychiatric inpatients. As the number of indicators of psychosis increased, the greater the estimated premorbid/current IQ discrepancy, providing evidence that more severe psychopathology was associated with putative intellectual decline. Importantly, this discrepancy was not associated with differences in our estimators of premorbid intellectual functioning, because there were no significant differences in reading scores as a function of the number of psychotic indicators. Follow up analyses demonstrated that potential confounding variables such as demographic differences or varying treatments were not the primary factor accounting for the discrepancy between estimated premorbid IQ and current IQ. Indicators of psychosis from the domains of clinical chart diagnoses, clinical ratings of the presence and severity of psychotic symptoms, and self-reports of psychotic symptoms were all independently associated with risk for lower current IQs relative to premorbid estimates.
There are several limitations of the present study that need to be addressed. Not all adolescents who were admitted to the hospital received psychological assessment, which means that the results need to be interpreted in the context of a consecutive sample of assessment referrals and not a consecutive sample of admissions. The chart diagnoses were not confirmed with research procedures. Recent studies have suggested that first-episode patients with psychotic disorders are often diagnosed by experienced clinicians with considerable accuracy, relative to structured research diagnostic procedures.33 In the absence of a structured, research-quality diagnosis, the validity of the specific diagnoses may still be questionable as a predictor. This is why we do not view the lack of differences across the specific psychosis diagnoses in their relationship with intellectual decline with the same level of certainty as the findings regarding the correlation of the number of psychosis indicators and intellectual performance. In previous studies of the adolescent population of this hospital involving structured research diagnoses,34 the prevalence of schizophrenia and schizophreniform diagnoses was essentially the same as this study. Another limitation that should be addressed is the use of the Hopkins Psychiatric Rating Scale. Although the Hopkins Psychiatric Rating Scale is a clinical rating scale for examining various aspects of psychiatric symptomatology, it is not widely used in research studies for rating psychotic symptoms. Consequently, it may produce subtly different scores than the rating scales more commonly used in such research (e.g., Brief Psychiatric Rating Scale or the Positive and Negative Syndrome Scale).
A final limitation to be considered is the use of estimated premorbid functioning. Despite the previous data regarding the validity of this procedure reviewed above, such estimates are clearly a substitute for direct performance measures collected before the onset of psychosis. Further, the crystallized intelligence nature of the reading scores may simply mean that they are less vulnerable to interference from psychosis than the full-scale IQ measures. If this interpretation was true, then the results would not reflect decline in intelligence but rather discrepancy in performance within psychosis.
It could also be argued that since the two clinical ratings and two MMPI indicators were generated from similar sources, they are too highly related to be meaningful as independent predictors. The results of this study argue against that interpretation. Individuals with all indicators of psychosis present had a significantly lower current IQ compared to their reading scores than individuals with three or four indicators, suggesting that the presence of all of these indicators, despite their intrinsic relationships with each other, is associated with differences in intellectual performance and putative intellectual decline.
Lower current IQ as compared to estimated premorbid IQ was not uniquely associated with a clinical diagnosis of schizophrenia. In fact, this was a heterogeneous clinical sample and the diagnosis of schizophrenia was rare compared to other psychotic conditions. Studies of the stability of first episode diagnoses of psychotic patients35 have found that the majority of patients, whose first diagnoses later changed, were initially diagnosed with psychosis not otherwise specified by their treating clinicians and were later rediagnosed with a schizophrenia spectrum diagnosis. Since many of the patients in this study received this diagnosis, they might be expected to meet criteria for schizophrenia later. Given the fact that there are a number of individuals with a current psychotic disorder that has been shown to increase likelihood of a later schizophrenia diagnosis, previous reports of deterioration from premorbid functioning at the time of the first schizophrenic episode may also be applicable to individuals with a diagnosis of another psychotic condition. Our findings suggest that intellectual downturn may occur early in the process of the development of illness, detectable as soon as the substantial indicators of psychosis are present. In a recent study of 107 first episode schizophrenia-related psychosis patients (schizophrenia, schizoaffective, and schizophreniform), Townsend et al.36 reported a 7-point discrepancy between a full-scale IQ measured with the WAIS-III and that obtained from the National Adult Reading Test.37 This discrepancy, about 0.5 standard deviations, was consistent with the level of impairment seen on measures of episodic memory and working memory in that study. As a result, those investigators also found that individuals with an array of schizophrenia-related conditions, including those with affective features, demonstrated intellectual decline.
The magnitude of the discrepancy between estimated premorbid and measured current IQ in this study was quite substantial, approximately 0.67 standard deviations lower in cases with five indicators of psychosis relative to cases with no indicators of psychosis. This study also provides a direct comparison for evaluation of the potential overestimation of premorbid IQ by the WRAT-3, which is important regarding inferences for decline. There was a 4-point discrepancy between WRAT-3 and Wechsler IQ in the subsample with no indicators of psychosis, suggesting that there is some overestimation of Wechsler IQ when using WRAT-3 scores. This overestimation is still 10 points less than the discrepancy seen in the cases with five indicators of psychosis. Thus, inflations of the estimated premorbid IQ are not the likely cause of the discrepancy, although they may contribute to its size. Longitudinal follow up will be required in order to determine if the intellectual decline seen in individuals with heterogeneous psychotic diagnoses resolves, worsens, or remains stable. Furthermore, the instability of clinical diagnoses at the time of the first psychotic episode, even when generated with a formal research procedure, means that many of the current cases with nonschizophrenic diagnoses may later receive diagnoses in the schizophrenia spectrum. Regardless of whether diagnoses would be liable to change later, the current data indicate that there is some evidence that intellectual decline is present at the time of a first psychotic episode and that this decline does not appear specific to receiving a clinical diagnosis of schizophrenia or schizophreniform disorder.
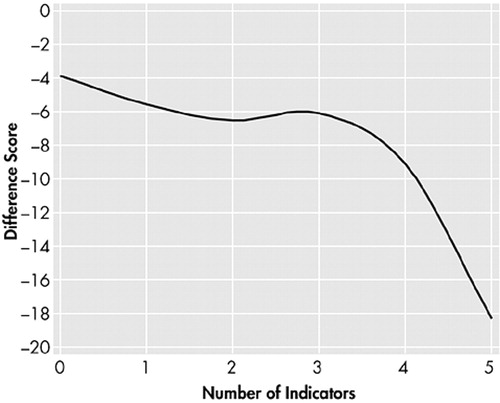
FIGURE 1. Difference Scores Between WRAT and Wechsler IQ Scores as a Function of Number of Psychotic Indicators Present
 |
 |
1 Aylward E, Walker E, Bettes B: Intelligence in schizophrenia: meta-analysis of the research. Schizophr Bull 1984; 10:430–459Crossref, Medline, Google Scholar
2 Weickert TW, Goldberg TE: The course of cognitive impairment in patients with schizophrenia, in Cognition in Schizophrenia: Impairments, Importance and Treatment Strategies. Edited by Sharma T, Harvey P. New York, Oxford University Press, 2000, pp 3–15Google Scholar
3 Weickert TW, Goldberg TE, Gold JM, et al: Cognitive impairments in patients with schizophrenia displaying preserved and compromised intellect. Arch Gen Psychiatry 2000; 57:907–913Crossref, Medline, Google Scholar
4 Bilder RM, Goldman RS, Robinson D, et al: Neuropsychology of first-episode schizophrenia: initial characterization and clinical correlates. Am J Psychiatry 2000; 157:549–559Crossref, Medline, Google Scholar
5 Hoff AL, Riordan H, O’Donnell DW, et al: Neuropsychological functioning of first-episode schizophreniform patients. Am J Psychiatry 1992; 149:898–903Crossref, Medline, Google Scholar
6 Saykin AJ, Shtasel DL, Gur RE, et al: Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry 1994; 51:124–131Crossref, Medline, Google Scholar
7 Mojtabai R, Bromet EJ, Harvey PD, et al: Neuropsychological differences between first-admission schizophrenia and psychotic affective disorders. Am J Psychiatry 2000; 157:1453–1460Crossref, Medline, Google Scholar
8 Russell AJ, Munro JC, Jones PB, et al: Schizophrenia and the myth of intellectual decline. Am J Psychiatry 1997; 154:635–639Crossref, Medline, Google Scholar
9 Davidson M, Reichenberg A, Rabinowitz J, et al: Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am J Psychiatry 1999; 156:1328–1335Medline, Google Scholar
10 Nelson HE, Pantelis C, Carruthers K, et al: Cognitive functioning and symptomatology in chronic schizophrenia. Psychol Med 1990; 20:357–365Crossref, Medline, Google Scholar
11 Bedwell JS, Keller B, Smith AK, et al: Why does postpsychotic IQ decline in childhood-onset schizophrenia? Am J Psychiatry 1999; 156:1996–1997Medline, Google Scholar
12 Bilder RM, Lipschutz-Broch L, Reiter G, et al: Intellectual deficits in first-episode schizophrenia: evidence for progressive deterioration. Schizophr Bull 1992; 18:437–438Crossref, Medline, Google Scholar
13 Amminger GP, Schlogelhofer M, Lehner T, et al: Premorbid performance IQ deficit in schizophrenia. Acta Psychiatr Scand 2000; 102:414–422Crossref, Medline, Google Scholar
14 Kremen WS, Buka SL, Seidman LJ, et al: IQ decline during childhood and adult psychotic symptoms in a community sample: a 19-year longitudinal study. Am J Psychiatry 1998; 155:672–677Crossref, Medline, Google Scholar
15 Gladsjo JA, Heaton RK, Palmer BW, et al: Use of oral reading to estimate premorbid intellectual and neuropsychological functioning. J Int Neuropsychol Soc 1999; 5:247–254Crossref, Medline, Google Scholar
16 Harvey PD, Moriarty PJ, Friedman JI, et al: Differential preservation of cognitive functions in geriatric patients with lifelong chronic schizophrenia: less impairment in reading compared with other skill areas. Biol Psychiatry 2000; 47:962–968Crossref, Medline, Google Scholar
17 Kremen WS, Seidman LJ, Faraone SV, et al: The “3R’s” and neuropsychological function in schizophrenia: an empirical test of the matching fallacy in biological relatives. Psychiatry Res 1995; 56:135–143Crossref, Medline, Google Scholar
18 Russell AJ, Munro J, Jones PB, et al: The National Adult Reading Test as a measure of premorbid IQ in schizophrenia. Br J Clin Psychol 2000; 39:297–305Crossref, Medline, Google Scholar
19 Tracy JI, McGrory AC, Josiassen RC, et al: A comparison of reading and demographic-based estimates of premorbid intelligence in schizophrenia. Schizophr Res 1996; 22:103–109Crossref, Medline, Google Scholar
20 Nelson HE, McKenna P: The use of current reading ability in the assessment of dementia. Br J Soc Clin Psychol 1995; 14:259–267Crossref, Google Scholar
21 Lezenweger MF: Psychometric high-risk paradigms, perceptual aberrations and schizotypy update. Schizophr Bull 1994; 20:121–135Crossref, Medline, Google Scholar
22 Lezenweger MF, Dworkin RH, Wethington E: Examining the underlying structure of schizophrenic phenomenology: evidence for a three-process model. Schizophr Bull 1991; 17:515–524Crossref, Medline, Google Scholar
23 Lezenweger MF, Gold JM: Auditory working memory and verbal recall memory in schizotypy. Schizophr Res 2000; 42:101–110Crossref, Medline, Google Scholar
24 Chapman LJ, Chapman JP, Kwapil TR, et al: Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol 1994; 103:171–183Crossref, Medline, Google Scholar
25 Kwapil TR, Miller MB, Zinser MC, et al: Magical ideation and social anhedonia as predictors of psychosis proneness: a partial replication. J Abnorm Psychol 1997; 106:491–495Crossref, Medline, Google Scholar
26 Merritt RD, Balogh DW: A comparison of the MMPI and the Psychosis Proneness Scales in their classifications of normal controls for use in schizophrenia spectrum research. J Pers Assess 1994; 62:204–212Crossref, Medline, Google Scholar
27 Golden RR, Meehl PE: Detection of the schizoid taxon with MMPI indicators. J Abnorm Psychol 1979; 88:217–233Crossref, Medline, Google Scholar
28 Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1983Google Scholar
29 Pogge DL, Wayland-Smith D, Zaccario M, et al: Diagnostic accuracy of manic episodes in adolescent inpatients: implications for treatment and outcome. Psychiatry Res 2001; 101:47–54Crossref, Medline, Google Scholar
30 Ben-Porath YS, Sherwood NE: The MMPI-2 Content Component Scales: Development, Psychometric Characteristics, and Clinical Application. Minneapolis, University of Minnesota Press, 1993Google Scholar
31 Wetzler S, Khadivi A, Moser RK: The use of the MMPI-2 for the assessment of depressive and psychotic disorders. Assessment 1998; 5:249–261Crossref, Medline, Google Scholar
32 Greene RL: The MMPI-2: an interpretive manual. Boston: Allyn and Bacon, 2000Google Scholar
33 Fennig S, Craig T, Lavelle J, et al: Best-estimate versus structured-interview-based diagnosis in first-admission psychosis. Compr Psychiatry 1994; 35:341–348Crossref, Medline, Google Scholar
34 Harvey PD, Lord J, Stokes J, et al: Neurocognitive and personality assessment of adolescent substance abusers: a multidimensional approach. Assessment 1996; 3:237–249Crossref, Google Scholar
35 Schwartz JE, Fennig S, Tanenberg-Karant M, et al: Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry 2000; 57:593–600Crossref, Medline, Google Scholar
36 Townsend LA, Malla AK, Norman RM: Cognitive functioning in stabilized first-episode psychosis patients. Psychiatry Res 2001; 104:119–131Crossref, Medline, Google Scholar
37 Nelson HE: National Adult Reading Test (NART): Test Manual. Windsor, UK, National Foundation for Educational Research-Nelson, 1982Google Scholar