Generalized Peripheral Nerve Hyperexcitability Associated With Lithium
To the Editor: Approximately one out of every 1,000–1,500 people in Western countries are receiving lithium treatment, mainly for a diagnosis of bipolar disorder. 1 The overall incidence of side effects on the CNS ranges from 35% to 50%, with lithium serum levels within the therapeutic range. 2 They often include an acute encephalopathy with cognitive impairment, hallucinations, insomnia, movement disorders, seizures, cerebellar signs, nystagmus, and ocular motor defects. Among the neuromuscular side effects, myopathy, axonal neuropathy, and a myasthenic syndrome were reported. 3 In the majority of cases, drug discontinuation implies complete recovery. Here we describe a patient presenting with an acquired generalized peripheral nerve hyperexcitability associated with lithium treatment.
Case Report
A 73-year-old man with a longstanding history of bipolar II disorder was admitted to our neurology department for acute onset of confusion, dysarthria, gait disturbances, muscle stiffness with cramps, and widespread twitching. He reported a fever 3 days before admission. There was no previous history of neurological or neuromuscular disorders. The patient had been taking lithium carbonate (600 mg daily) and venlafaxine (75 mg/day) in the last 3 years. Neurological examination showed an unsteady gait, dysarthria, resting and postural tremor of the upper and lower limbs, mild bradykinesia and rigidity, and prominent muscle twitching of the tongue and the four limbs. Reflexes were symmetrical. Mini-Mental State Examination (MMSE) and Milan Overall Dementia Assessment (MODA) were 24.3 and 89.8, respectively. Routine blood tests including inflammation indexes, electrolytes, renal and thyroid function, creatine kinase, glucose, vitamin B 12 , folate, and ammonium were normal. Lithium serum level was within the normal range (0.8 meq/liter). Voltage-gated potassium channel antibodies and acetylcholine receptor antibodies were negative. A brain CT scan showed a vascular encephalopathy. An EEG showed a widespread slowing of the background activity with outbursts of generalized theta-delta abnormalities. Motor and sensory nerve conductions were in the normal range. Repetitive stimulation of the motor nerves revealed no myasthenic defect. The needle electromyogram (EMG) disclosed no neuropathic or myopathic features. However, widespread spontaneous motor unit discharges were recorded in the form of doublets, triplets, or multiplets with high intraburst frequencies (50 Hz–160 Hz), occurring at irregular intervals. They were interposed by fasciculation potentials and myokymic discharges ( Figure 1 ). The overall neurophysiological picture met the criteria suggested by Maddison 4 for the diagnosis of the peripheral nerve hyperexcitability “neuromyotonia phenotype.” Since the extensive search for other peripheral nerve hyperexcitability causes was negative, lithium was hypothesized to be responsible for the picture. Indeed, after lithium withdrawal the patient experienced a complete clinical recovery with disappearance of the neurological signs. The treatment with venlafaxine was kept unchanged. Two months later, the EMG and neuromuscular picture remained normal.
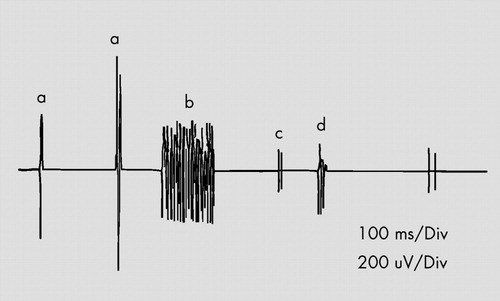
Recording of fasciculations (a), myokymic discharges (b), doublets (c), and multiplets (d) from the right tibialis anterior muscle.
Discussion
Our patient presented several predisposing factors for lithium toxicity: elderly age, fever, and vascular encephalopathy. 5 Side effects in the CNS such as confusional state, dysarthria, extrapyramidal signs, and EEG abnormalities may occur within lithium therapeutic range. 2 The combination of lithium with antidepressant drugs has been associated with the occurrence of severe toxic pictures such as the serotonin syndrome. 6 However, this possibility was ruled out because the patient’s symptoms did not meet the relevant diagnostic criteria. 7 Conversely, to the best of our knowledge, there is no previous report of a peripheral nerve hyperexcitability associated with lithium.
Peripheral nerve hyperexcitability is a rare disorder characterized by generalized hyperexcitability of motor nerves resulting in continuous and spontaneous muscle fiber activity (e.g., fasciculations, myokymias, or multiplets). 8 It is not a single disease but represents a response to peripheral nerve dysfunction due to several sources such as autoimmune diseases (e.g., systemic lupus erythematosus, myasthenia gravis, Hashimoto thyroiditis), anterior horn cell degeneration, genetic disorders (e.g., voltage-gated potassium-channel gene mutation, familial episodic ataxia type I, hereditary neuropathy), intoxications (e.g., herbicides, insecticides, toluene), or drugs (gold, oxaliplatin). 8 , 9 The pathogenesis of drug-induced peripheral nerve hyperexcitability is not completely clear. Evidence from basic science studies suggested that peripheral nerve hyperexcitability during oxaliplatin treatment may be related to a delay in entry of voltage-gated sodium channels into an inactive state, allowing greater sodium currents to enter the cell, 9 resulting in a repetitive firing and hyperexcitability. Considering the fact that lithium may interact with the sodium channel kinetics, 3 it is tempting to speculate that the peripheral nerve hyperexcitability observed in our patient may have a similar pathogenesis.
In our opinion, physicians should be aware of the spectrum of lithium side effects on the neuromuscular system, including peripheral nerve hyperexcitability. Further studies are needed to clarify the epidemiological, clinical, and pathophysiological nature of such phenomena.
1. Vestergaard P, Schou M: Lithium treatment in Aarhus. 1. Prevalence. Pharmacopsychiatry 1989; 22:99–100Google Scholar
2. Shopsin B, Johnson G, Gershon S: Neurotoxicity with lithium: differential drug responsiveness. Int Pharmacopsychiatry 1970; 5:170–182Google Scholar
3. Van Kempen GMJ: Lithium, in Handbook of Clinical Neurology: Intoxications of the Nervous System, vol 20, part I. Edited by de Wolff FA. Amsterdam, Elsevier Sciences, 1994, pp 293–302Google Scholar
4. Maddison P, Mills KR, Newsom-Davis J: Clinical electrophysiological characterization of the acquired neuromyotonia phenotype of autoimmune peripheral nerve hyperexcitability. Muscle Nerve 2006; 33:801–808Google Scholar
5. Markham Brown T, Studemire A: Psychiatric Side Effects of Prescription and Over-the-Counter Medications. Washington, DC, American Psychiatric Press, 1998, pp 83–92Google Scholar
6. Adan-Manes J, Novalbos J, Lopez-Rodriguez R, et al: Lithium and venlafaxine interaction: a case of serotonin syndrome. J Clin Pharm Ther 2006; 31:397–400Google Scholar
7. Boyer EW, Shannon M: The serotonin syndrome. N Engl J Med 2005; 352:1112–1120Google Scholar
8. Maddison P: Neuromyotonia. Clin Neurophysiol 2006; 117:2118–2127Google Scholar
9. Webster RG, Brain KL, Wilson R, et al: Oxaliplatin induces hyperexcitability at motor and autonomic neuromuscular junction through effects on voltage-gated sodium channels. Br J Pharmacol 2005; 146:1027–1039Google Scholar



