Capgras Syndrome Associated With Fahr's Disease
To the Editor: Capgras syndrome is a specific misidentification syndrome in which the person believes that another person, with whom he or she has close emotional ties as well as ambivalence at the same time, has been replaced by an persecutory imposter. Capgras syndrome has been found in a number of neuropsychiatric conditions like Alzheimer’s disease, parkinsonism, vascular dementia, stroke, multiple sclerosis, and schizophrenia-like-psychosis. 1 Fahr’s disease is a clinical entity with idiopathic bilateral basal ganglia calcification in the absence of any clinical or biochemical abnormality. Up to 50% of idiopathic bilateral basal ganglia calcification present with neuropsychiatric manifestations, which include auditory and visual hallucinations, complex delusions, and schizophrenia-like psychosis. 2 We describe an association between idiopathic bilateral basal ganglia calcification and Capgras syndrome, which has not been reported earlier.
Case Report
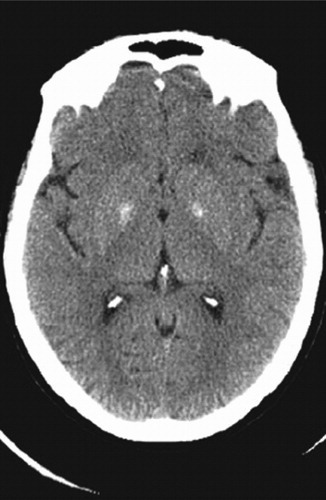
A 30-year-old woman diagnosed with paranoid schizophrenia for 6 years was maintaining well on olanzapine, 15 mg/day, with good compliance. She presented with a 6-month history of misidentifying her husband as an imposter with malice, suggestive of Capgras syndrome. There was no other associated psychopathology. A detailed physical and neurological examination suggested bilateral pedal pitting edema and positive left-sided palmomental reflex, without any evidence of cognitive impairment or move-ment disorder. A contrast-enhanced CT brain scan revealed bilateral basal ganglia calcification, involving the pallidal region ( Figure 1 ). Laboratory tests including hemogram, thyroid function test, and serum calcium were within normal limits. A neurologist, whose opinion was sought in view of the CT findings, suggested the calcification as idiopathic. The patient’s olanzapine was increased to 25 mg/day for the next 3 months; following this the Capgras phenomenon resolved. However, she developed delusions of infidelity during follow-up, which resolved after increasing olanzapine to 30 mg/day.
Discussion
In Capgras syndrome there is a disruption of facial recognition circuitry, resulting in facial misidentification. 3 The structural and functional neuroimaging studies in Capgras syndrome have localized the involvement of the bilateral parietal and posterior frontal regions with more frequent involvement of the nondominant cerebral hemisphere. 4 Till now, no particular circuit involving basal ganglia has been implicated in Capgras syndrome, although hypodensity of lenticular nucleus has been reported. 5 The CT scan of our patient revealed idiopathic bilateral basal ganglia calcification involving the pallidum. We hypothesize that, in our case, basal ganglia calcification could have disrupted one of the cortico-subcortical circuits, which might have some contribution in facial processing systems. Basal ganglia calcification leading to disruption of the thalamo-cortico-striatal circuit has been reported to manifest as schizophrenia-like psychosis. The isolated Capgras phenomenon in our case could be a part of the schizophrenia process resulting from the same mechanism. 6 A dysfunctional input of basal ganglia to the prefrontal cortex as seen in Capgras syndrome in parkinsonism 7 could be a third proposition.
1. Feinberg TE, Roane DM: Delusional misidentification. Psychiatr Clin North Am 2005; 28:665–683Google Scholar
2. Francis AF: Familial basal ganglia calcification and schizophreniform psychosis. Br J Psychiatry 1979; 79:360–362Google Scholar
3. Papageorgiou C, Lykouras L, Ventouras E, et al: Abnormal P300 in a case of delusional misidentification with coinciding capgras and Frégoli symptoms. Prog Neuropsychopharmacol Biol Psychiatry 2002; 26:805–810Google Scholar
4. Eren I, Civi I, Yildiz M: Frontoparietal hypoperfusion in capgras syndrome: a case report and review. Turk Psikiyatri Derg 2005; 16:284–290Google Scholar
5. Paillère-Martinot ML, Dao-Castellana MH, Masure MC, et al: Frontoparietal hypoperfusion in capgras syndrome: a case report and review. Psychopathology 1994; 27:200–210Google Scholar
6. Chabot B, Roulland C, Dollfus S: Schizophrenia and familial idiopathic basal ganglia calcification: a case report. Psychol Med 2001; 31:741–747Google Scholar
7. Roane DM, Rogers JD, Robinson JH, et al: Delusional misidentification in association with parkinsonism. J Neuropsychiatr Clin Neurosci 1998; 10:194–198Google Scholar



