Retropulsion and Back Bruises in Drug-Induced Parkinsonism
To the Editor: Drug-induced parkinsonism is common especially in the psychiatric population where it can be overlooked. 1 , 2 Among other extrapyramidal features, falls due to retropulsion are common and frequently lead to considerable clinical implications, including injuries and high cost of hospitalization. The pathophysiology of falls in parkinsonian disorders is growing and points to a loss of intersegmental flexibility (or axial rigidity) that predisposes patients to fall backward or in lateral directions. 3 In this case, we report multiple bruises noted on the skin examination of a patient admitted with excessive retropulsive falls.
Case Report
A 74-year-old man with history of bipolar depression presented with increasing backward falls that became pronounced following the initiation of a D2-receptor blocker (risperidone). Neurological examination showed multiple extrapyramidal signs including a rest tremor in the right hand, axial rigidity, decreased blink rate, masked facies, and stooped posture with profound postural instability and retropulsion. Backward shoulder pull test was positive for a minimum of five steps with severe tendency to fall. He also exhibited positive glabellar and palmomental reflexes consistent with release of frontal inhibition. Further inspection of the skin revealed severe bilateral bruises in the lower back ( Figure 1 ). A noncontrasted CT scan of the brain showed mild atrophy. The dose of risperidone was reduced, and his axial rigidity has improved.
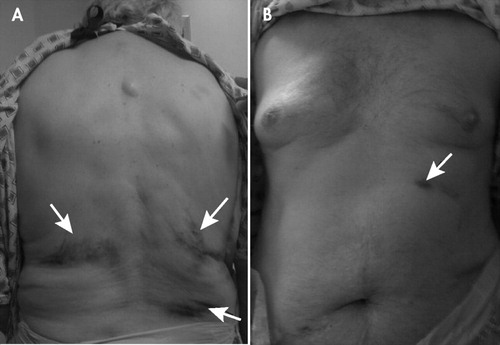
Inspection of the chest and abdomen posteriorly (A) and anteriorly (B) shows multiple bruises in the lower back compared to minimal bruises in the front (arrows), confirming the presence of retropulsion and backward falls.
Discussion
Subtle extrapyramidal signs are often overlooked on neurological examination. The severity of falls in patients with drug-induced parkinsonism is assessed by adequate clinical history of fall frequency and coexisting injuries in addition to the positive shoulder pull test. 4 Coexisting injuries requiring professional health care are reported in 75% of falls, including bone fractures in 30%. 5 Thorough inspection of the skin in these patients may ascertain evidence and point to the severity of backward falls and retropulsion in Parkinson’s disease and other parkinsonian disorders including drug-induced parkinsonism.
1. Alvarez MV, Evidente VG: Understanding drug-induced parkinsonism: separating pearls from oysters. Neurology 2008; 70:e32–34Google Scholar
2. Błaszczyk J, Orawiec R, Duda-Kłodowska D, et al: Assessment of postural instability in patients with Parkinson’s disease. Exp Brain Res 2007; 183:107–114Google Scholar
3. Grimbergen YA, Munneke M, Bloem BR: Falls in Parkinson’s disease. Curr Opin Neurol 2004; 17:405–415Google Scholar
4. Visser M, Marinus J, Bloem BR, et al: Clinical tests for the evaluation of postural instability in patients with Parkinson’s disease. Arch Phys Med Rehabil 2003; 84:1669–1674Google Scholar
5. Wielinski CL, Erickson-Davis C, Wichmann R, et al: Falls and injuries resulting from falls among patients with Parkinson’s disease and other parkinsonian syndromes. Mov Disord 2005; 20:410–415Google Scholar



