Rapid Cycling Associated With Menstrual Periods in an Adolescent: Electrophysiological Underpinnings for Bipolarity
To the Editor: Affective fluctuations during menstruation have drawn considerable interest from researchers for a long time. 1 Data indicates increased frequency of depression associated with menstrual period in adolescence, 2 though there is limited information about the differences in the course or symptoms of bipolar disorder associated with menstrual period in adolescents. The question of the direction of mood shifts in the course of bipolar disorder with specific phases of menstrual cycle has been raised, albeit with limited and inconsistent results. 3 We present a case of an adolescent female with cyclic affective changes akin to rapid cycling bipolar disorder starting in the premenstrual (luteal) period and subsiding with onset of menstruation, and we try to explore the biological underpinnings of inherent propensity for the development of bipolar disorder using quantitative electroencephalography (qEEG).
Case Report
Our patient is a 15-year-old Asian Hindu girl from a middle socioeconomic background with no significant birth, development, personal, medical, or family history. She presented with complaints of excessive talking, tall claims, irritability, headache, increased goal-directed activity, decreased need for sleep, and increased appetite for 5 days which started abruptly 3 days before the onset of menstrual bleeding. Patient attained menarche at the age of 12 years old. Her history revealed 1 year of six similar brief episodes occurring 2–3 days prior to the onset of her menstrual bleeding, which subsided after 2–3 days of bleeding with complete recovery. This time the symptoms persisted even after cessation of menstrual bleeding, which led to our consultation. There was no prior history of menstrual irregularities or endocrinal dysfunction. Physical examination was unremarkable and mental status examination revealed an irritable patient with overproductive speech, euphoric affect, subjective racing of thoughts, and grandiose plans. We made a diagnosis of bipolar disorder, rapid cycling. Routine clinical investigations were unremarkable. A detailed endocrinal workup including thyroid profile, hormone assay, and an ultrasound of thyroid and abdomen revealed no abnormality.
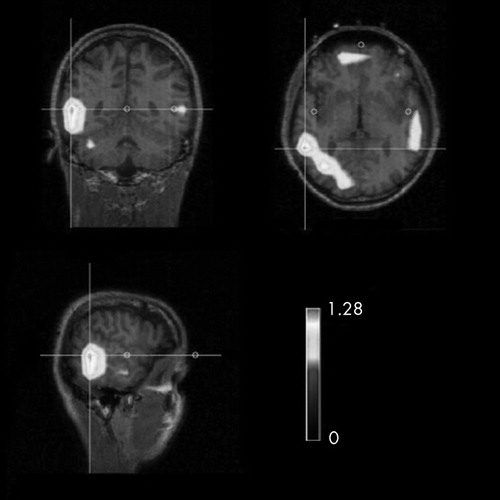
A 32-channel qEEG and advanced source analysis was obtained in this patient during the acute phase of the illness with scalp electrodes using the International 10–20 system. It did not reveal any abnormality on qualitative examination. Spectral mapping was done with fast Fourier transformation, and source localization was done by low-resolution electromagnetic tomography (LORETA). It was conducted over a 20-minute EEG tracing where multiple epochs were taken each of 0.256 second duration with overlapping by −1.000 second followed by averaging of the entire data. We used ASA version 2.5 (ANT, Inc.). There was high spectral power in low frequency (theta band) over the right temporal region which was further corroborated by LORETA and revealed high signal density over the right temporal region for the same frequency band ( Figure 1 ). Clinical severity rating using the Young Mania Rating Scale 4 revealed a score of 23 on the day of qEEG. The patient was prescribed lithium, 600 mg/day, which was gradually increased to 1,050 mg/day after serum lithium estimation. She showed good response, and her Young Mania Rating Scale score at the end of 4 weeks dropped to 8. Lithium was continued, and over the next 4 months she had only one such episode of milder intensity when lithium was optimized to 1,200 mg/day with a lithium level of 0.84 mmol/L.
Discussion
Rapid cycling is reported more frequently in female children or adolescents with bipolar disorder. Prospective studies which followed up the cases for at least 3 months found no significant relationship between mood shift and the menstrual cycle in adults with mood disorder. 5 , 6 Our patient presented with affective changes occurring cyclically in the luteal phase preceding menstruation and subsiding with onset of menstrual flow. Such cyclical instability could reflect episodic exacerbation of an underlying mood disorder, but in this case absence of nonmenstrual mood episodes and family history of affective illness rules out this possibility.
A review 3 presented findings of 24 prospective studies of affective fluctuations during the menstrual cycle. In most cases the authors found that negative moods marked by irritability, restlessness, anxiety, tension, migraine, sleep disturbance, and impaired concentration occurred more often during the premenstrual and menstrual phases than at other times in the cycle. There were only a few cases of positive moods—such as an increased feeling of well-being, elation, pleasantness, and activation—during the follicular and midcycle phases. 3 This case presents with positive mood state, though irritability and headache were present as seen in premenstrual syndrome (PMS). This is an atypical presentation of PMS as opposed to the more common occurrence of elated moods during midcycle; in our case it occurred in premenstrual phase. 7 It has been reported that whereas menstrual problems appear to occur more frequently in younger than in older women, premenstrual symptoms occur more often in older women. This suggests a relation between age and menstrual symptoms. 8 However, our patient is in her middle adolescence, thus making her presentation relatively unique. Premenstrual affective syndrome is a positive predictor for the development of major affective disorders under stressful conditions. 9 In our patient, these brief episodes of affective dysregulation with mania-like presentation could be conceptualized as an atypical presentation of PMS carrying a risk of future bipolarity.
Several interesting associations between EEG findings and the clinical features of mania have been reported. Right-sided abnormalities are associated with affective illness, whereas the left side is more implicated in schizophrenia. 9 Quantitative EEG has been more frequently applied to the study of manic patients and less often in studies of children and adolescents. The qEEG findings appear to implicate dominant temporal lobe dysfunctions in mania, though most of the research is done in adult populations. 11 To the contrary, in our case there was high spectral power over the right temporal region in the theta frequency band which was localized to the right temporal region in LORETA. Similar findings were found in a study comparing bipolar disorder patients with chronic schizophrenia patients, which revealed a significantly higher power of EEG signals on the right side in the former group. 12 Our findings, though not conclusive, can be viewed in light of the available imaging findings which suggest structural abnormalities in the amygdala in bipolar disorder patients, though data on the younger population is sparse. 13 The overlap in symptomatology between PMS and cyclothymia, often considered to be a variant of manic-depressive illness, has given rise to therapeutic trials of lithium carbonate in women with PMS, with mixed results. 14 Lithium treatment has been beneficial in controlling premenstrual affective changes, and this led us to use the same in our case.
Conclusion
As there are quantitative neurobiological indicators in terms of findings in qEEG, we will closely monitor this case in order to look for future bipolarity, further implicating long-term treatment with a mood stabilizer.
1. Steiner M, Born L: Psychiatric aspects of menstrual cycle, in Women’s Mental Health. Edited by Kornstein SG, Clayton AH. New York, Guilford, 2002Google Scholar
2. Mattisson C, Bogren M, Nettelbladh P, et al: First incidence depression in the Lundby study: a comparison of the two time periods 1947–1972 and 1972–1997. J Affect Disord 2005; 87:151–160Google Scholar
3. Akdeniz F, Karadag F: Does the menstrual cycle affect mood disorders? Türk Psikiyatri Dergisi 2006; 17:1–9Google Scholar
4. Young RC, Biggs JT, Ziegler VE, et al: A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 1978; 133:429–435Google Scholar
5. Wehr TA, Sack DA, Rosenthal NE, et al: Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988; 145:179–184Google Scholar
6. Leibenluft E, Ashman SB, Feldman-Naim S, et al: Lack of relationship between menstrual cycle phase and mood in a sample of women with rapid cycling bipolar disorder. Biol Psychiatry 1999; 46:577–580Google Scholar
7. Rasgon N, Bauer M, Glenn T, et al: Menstrual cycle related mood changes in women with bipolar disorder. Bipolar Disord 2003; 5:48–52Google Scholar
8. Ghadirian KM, Kamaraju LS: Premenstrual mood changes in affective disorders. CMAJ 1987; 136:1027–1032Google Scholar
9. Hsaio MC, Liu CY: Unusual manifestations of premenstrual syndrome. Psychiatry Clin Neurosci 2007; 61:120–123Google Scholar
10. Abrams R, Taylor MA: Differential EEG patterns in affective disorder and schizophrenia. Arch Gen Psychiatry 1979; 36:1355–1358Google Scholar
11. Small JG, Milstein V, Malloy FW, et al: Clinical and quantitative EEG studies of mania. J Affect Disord 1999; 53:217–224Google Scholar
12. Oluboka OJ, Stewart SL, Sharma V, et al: Preliminary assessment of intrahemispheric QEEG measures in bipolar mood disorders. Can J Psychiatry 2002; 47:368–374Google Scholar
13. Brambilla P, Harenski K, Nicoletti M, et al: MRI investigation of temporal lobe structures in bipolar patients. J Psychiatr Res 2003; 37:287–295Google Scholar
14. Steiner M, Haskett RF, Carroll BJ: Premenstrual tension syndrome: the development of diagnostic criteria and new rating scales. Acta Psychiatr Scand 1980; 62:177–190Google Scholar



