Secular Mindfulness-Based Interventions: Efficacy and Neurobiology
Mindfulness-based stress reduction (MBSR) was developed initially for patients with chronic pain conditions.10,11 Since that time, it has shown benefits across a wide range of physical and mental health conditions. Published randomized control trials (RCTs) for mindfulness interventions increased from seven between 2001 and 2003 to more than 200 between 2013 and 2015.12 In addition, 79% of medical schools now offer some variation of mindfulness training.13 The most widely used evidence-based mindfulness interventions stem from Buddhist meditation practices, which focus on breaking maladaptive habits and increasing the experience of positive emotions.14,15 MBSR served as a template for the later development of mindfulness-based cognitive therapy (MBCT) and mindfulness-based relapse prevention (MBRP).14,16,17 These secular mindfulness-based therapeutic interventions all share the goal of facilitating the development of the skills required to maintain a nonjudgmental awareness (e.g., accepting, open) while keeping attention focused on internal and external experiences occurring in the present moment.14,18 That is: observing one’s own thoughts in the present moment with objective curiosity.14,18 It is important to emphasize that mindfulness is not synonymous with relaxation and that relaxation is not the goal of mindfulness interventions. An article from Harvard Business Review in 2015 was titled, “If Mindfulness Makes You Uncomfortable, You’re Doing It Right.”
Development of mindfulness as a skill has been shown to have significant positive effects in both healthy community and clinical samples. Two recent meta analyses of studies assessing the effect of mindfulness interventions on groups of healthy individuals (e.g., undergraduate students, healthcare trainees, healthcare professionals, community members) reported moderate to large positive effects on multiple aspects of functioning (e.g., stress, anxiety, depression, quality of life).19,20 Studies support significant benefit for persons coping with physical conditions, (e.g., cancer, chronic low back pain, fibromyalgia, and migraines), as well as persons suffering from mental health disorders (i.e., depression, substance misuse, sexual trauma, anxiety, general stress, and emotional dysregulation). As is generally true for clinical research, publication and reporting bias for positive trials are problematic, potentially over-stating the effects of mindfulness-based interventions.21,22 Recent advancements have produced a standardized active control condition (i.e., an 8-week health enhancement program). If used consistently across RCTs, this could significantly decrease the surplus of confounding methodological variables.12,23
Recent reviews agree that mindfulness-based interventions are effective in improving many aspects of chronic pain (e.g., pain intensity, pain-related disability, quality of life, mental health issues).12,24 Two recent meta analyses of 25 RCTs of mindfulness interventions in patients with chronic pain conditions (unspecified chronic pain, musculoskeletal pain, fibromyalgia, rheumatoid arthritis) support modest beneficial effects.22,25 One meta-analysis identified RCTs that utilized either acceptance-based or mindfulness-based therapy.25 Multiple outcome measures (pain intensity, pain interference, disability, quality of life, depression, anxiety) were examined. Pooled standardized mean differences indicated that modest improvements (small to moderate effect sizes) were found on most outcome measures at the end of treatment. Pain interference and anxiety were the most improved (moderate effect sizes). Notably, only five studies included comparison to an active control (e.g., cognitive-behavioral therapy [CBT], relaxation training). Mindfulness interventions were superior to relaxation (moderate to large effect size) for most outcome measures, including quality of life, pain interference, disability, and depression. CBT was somewhat better (small effect size) for depression, pain interference, and disability. Thirteen studies included follow-up data (ranging from 2 to 12 months). Effect sizes were greater on all outcomes except pain intensity at follow-up.25 Both meta analyses raised concerns related to the considerable methodological heterogeneity across studies (e.g., sample make up and size, power, treatment length and adherence, comparison conditions, symptom measures).22,25 Some of these methodological issues have been addressed by the most recent RCTs. A large RCT (initial N=282, 6 month follow up N=253) of older adults with chronic lower back pain comparing MBSR to a health education program of the same duration reported modest (small effect sizes) short- and longer-term benefits for pain measures (current, most severe). Improvements on functional measures were not sustained at follow up.26 As noted by the authors, low levels of depressive symptoms at baseline and less-than-optimal treatment attendance limited generalizability of findings. Another large RCT (initial N=342, 52 week follow up N=290) in adults (20 to 70 years of age) with chronic (minimum 3 months) low back pain reported MBSR and CBT were both superior to usual care.27,28 A significantly greater percentage of the MBSR and CBT groups had clinically meaningful improvements (minimum 30%) in the primary outcome measures (disability questionnaire, self-reported pain bothersomeness) at 26 weeks.27 This difference was maintained at 52 weeks for the MSBR group. As noted in a related editorial, although participation in treatment was not optimal (only half of participants attended at least 6 out of the 8 group sessions), the findings support the value of these approaches for improving the lives of patients with chronic pain conditions.29 The analyses comparing specific elements of therapeutic outcomes that have been proposed as mechanisms of change associated with MBSR (increased mindfulness and pain acceptance) or CBT (decreased catastrophizing and increased self-efficacy) found that none of the predictions were fully supported.28 MBSR was significantly more effective in decreasing catastrophizing immediately post treatment and the interventions were similarly effective at 52 weeks. MBSR and CBT had similar benefits for self-efficacy immediately post treatment. Generally, no significant differences were observed between groups in pain acceptance and mindfulness. As noted by the authors, these results suggest that MBSR and CBT may be acting through similar therapeutic mechanisms.28
Although less studied, there is increasing evidence that mindfulness based interventions may be generally beneficial for other health conditions.12,24 Recent systematic reviews indicate preliminary evidence for the treatment of primary insomnia, somatization disorder, irritable bowel syndrome, asthma, tinnitus, as well as potential improvements in select immune system processes.23,30 A pilot study in Veterans with Gulf War Illness (defined as the combination of activity limiting fatigue, musculoskeletal pain in more than one area, and difficulty with concentration/memory) found MBSR plus usual care to be significantly more effective than usual care alone for improving all three symptom domains (medium to large effect size) by the 6 month follow-up.31 Also promising are mindfulness based interventions in adult primary care settings.32 A meta-analysis of six RCTs reported modest beneficial effects on general health, mental health and quality of life.32 Although encouraging, the authors noted the need for better designed studies and long-term follow-up measures. Surprisingly, one RCT found that participants’ self-reported utilization of healthcare services during the study period did not differ between the mindfulness and usual care groups.33 In contrast, studies based on administrative data capturing all healthcare services demonstrated marked decreases in health service usage following mindfulness interventions.34,35
Growing interest in mental health treatment incorporating mindfulness-based interventions has resulted in a surge of research encompassing a wide range of conditions, including mood, anxiety, psychotic, and substance use disorders.12,15,24,36–38 Recent meta analyses of RCTs indicate that mindfulness-based interventions are effective for relapse prevention in patients with recurrent depression.39,40 The meta-analysis (25 studies, follow up 17 to 332 weeks) that examined a range of psychological interventions (CBT, MBCT, interpersonal therapy) found that all were similarly effective in reducing relapse risk as compared with both treatment as usual and to maintenance antidepressant medication.39 Similar results were reported in the meta-analysis that focused on MBCT (nine studies, follow up 60 weeks).40 This study also reported preliminary evidence that MBCT might be more effective in patients with higher levels of residual symptoms prior to treatment. A meta-analysis of RCTs of mindfulness interventions (MBSR, MBCT) in patients meeting diagnostic criteria for current major depressive disorder or an anxiety disorder (e.g., social anxiety disorder, generalized anxiety disorder, posttraumatic stress disorder) demonstrated improvements (large effect size) in severity of primary symptoms for depressive disorder but not for anxiety disorders when compared with inactive control conditions.41 A health economics analysis found that provision of MBCT for Australian patients with recurrent depression receiving specialist mental health care was cost effective, as reductions in other health care costs (e.g., hospital services, ambulatory care) were greater than the cost of providing MBCT.42
Mindfulness interventions may have potential for treatment of anxiety disorders. Reviews indicate that even internet-based mindfulness interventions can be beneficial.43,44 A systematic review of mindfulness intervention studies for social anxiety disorder (SAD) found mindfulness based treatments to be effective, though not superior to CBT.45 A more recent RCT in patients with SAD focused on the effects of group CBT versus group MBSR.46 Results suggest that CBT and MBSR were equally effective in reducing symptoms and maintaining treatment gains at one-year follow up. Contrary to expectations, mediation analyses identified mostly shared psychological mechanisms of change for CBT and MBSR (i.e., decreased cognitive distortions and safety behaviors, increased reappraisal frequency, mindfulness skills, and attention focusing). A systematic review of mindfulness intervention studies for posttraumatic stress disorder (PTSD) found preliminary evidence that mindfulness-based treatments may be effective, although more methodologically rigorous studies are needed.47 A secondary analysis of four MBSR trials in Veterans with PTSD came to similar conclusions.48 Promising results were also reported for a brief (four session) mindfulness intervention for PTSD delivered within primary care.49 Mindfulness interventions may also be a useful alternative psychological treatment for comorbid conditions. A recent pilot study in Veterans with comorbid PTSD and mild traumatic brain injury found MBSR to be beneficial for both conditions (improving attention and decreasing PTSD symptoms).50 Positive aspects of this treatment in comparison to others included absence of adverse effects and high levels of acceptability. Veterans reported that the offering of diverse mindfulness exercises (e.g., body scan, yoga) was particularly helpful, as it presented a higher likelihood that at least one exercise would resonate with each individual.
Potential mechanisms of action have been evaluated in both a meta-analysis and a systematic review.51,52 Mediation analyses testing potential mechanisms of action for mental health outcomes (clinical and nonclinical populations) found moderate to strong evidence for improved cognitive and emotional reactivity, higher mindfulness, and decreased repetitive negative thinking (e.g., rumination, worry).51 Mechanisms of action in patients with recurrent major depression identified by multiple studies included increases in mindfulness-related skills (e.g., meta awareness, self-compassion) and decreases in negative thinking.52 Thus, it appears that mindfulness training is effecting fundamental cognitive processes, such as distress tolerance, cognitive and emotional reactivity, and emotional regulation.51,53
Although multiple reviews and meta analyses have identified a broad range of structural and functional brain differences associated with meditation practices, most studies are not directly relevant to understanding the neural correlates of secular therapeutic mindfulness interventions.54–56 The majority of studies are cross sectional (e.g., comparing long-term meditation practitioners to meditation-naïve individuals). This makes it very difficult to adequately control for the multiple factors differing between groups that have the potential to greatly affect brain structure and function. In addition, some studies combine very different types of meditation practices. Two recent meta analyses that were designed to identify the neural correlates of mindfulness meditation (defined either as open monitoring or as Buddhist inspired meditation) had only a few areas of agreement.57,58 More informative for clinical practice are longitudinal studies that assess change within an individual by obtaining measures both prior to and following a mindfulness intervention. Studies in healthy individuals have potential to provide insight into intervention-related neurobiological changes but may not be directly informative about mechanisms for therapeutic change. These are best addressed by longitudinal studies in specific clinical populations.
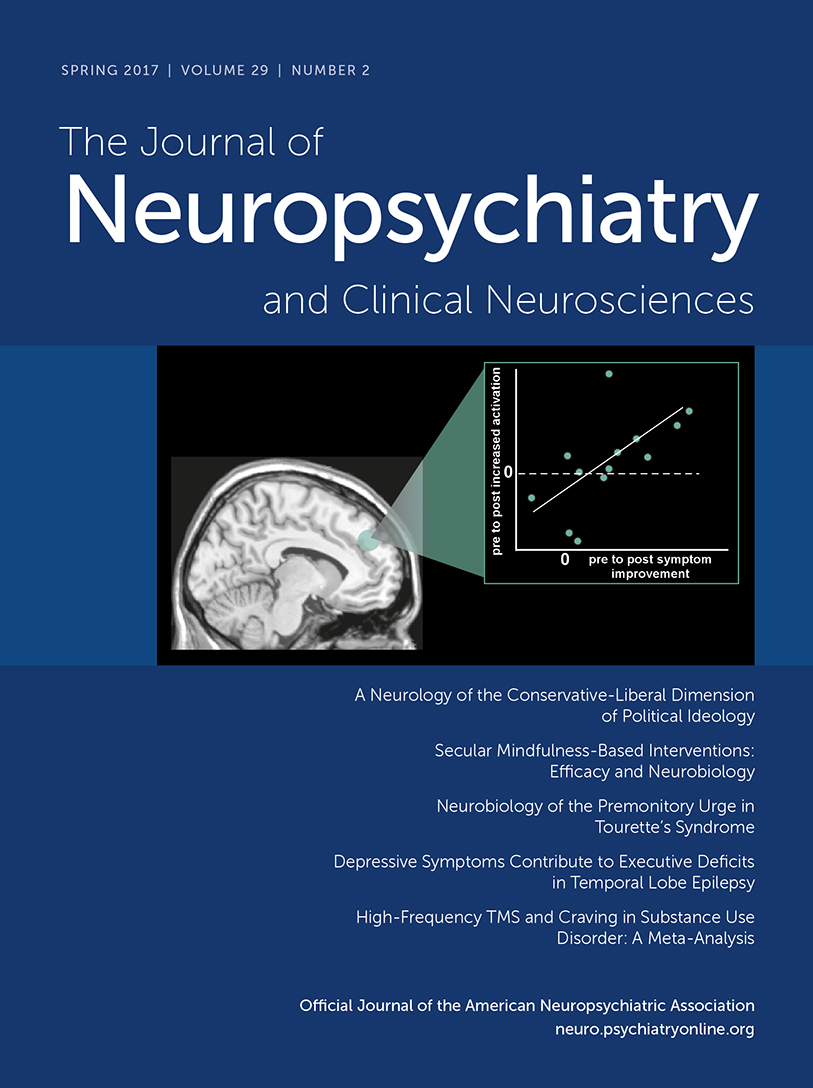
Several small studies have utilized functional magnetic resonance imaging (fMRI) with emotional tasks (e.g., emotional faces, self-referential negative and positive words, self-referential negative and positive beliefs) prior to and following mindfulness interventions in patients with anxiety disorders (SAD, generalized anxiety disorder, PTSD) to identify clinically-relevant training-related changes. Areas of convergence across studies include increased posttreatment activations in dorsomedial prefrontal cortex (PFC), anterior cingulate cortex (ACC) and ventrolateral PFC/anterior insula that correlated with symptom reductions (Figure 1).1–4 As noted by the authors of these studies, the results support treatment-related enhanced recruitment of areas contributing to emotional processing and regulation of emotional responding. Changes in the amygdala have also been reported. A study of patients with generalized anxiety disorder reported posttreatment normalization (decreased activation) of the amygdala response to neutral faces.2 Task-related functional connectivity of the amygdala with several areas (medial PFC/ACC, dorsolateral PFC) switched from negative (anticorrelated) to positive (correlated); these changes correlated with symptom improvement.2 A study in community adults reported that higher past month stress was associated with higher resting state connectivity between the amygdala and subgenual ACC (whole brain analysis).59 Resting state connectivity between these structures was decreased in the highly stressed subgroup (job-seeking unemployed) following an intensive (three day residential) MBSR intervention.59 In contrast, a study of patients with PTSD reported increased amygdala response to angry faces posttreatment that correlated with symptom improvement.3 Both task-related and resting state functional connectivity from the amygdala to the medial PFC (and other areas) increased, but these changes did not correlate with symptom improvement.3,5 However, increased posttreatment resting state functional connectivity between the posterior cingulate cortex (PCC) and dorsolateral PFC correlated with decreases in both the avoidant and hyperarousal symptoms clusters (Figure 2).5 The study in highly stressed community adults (job-seeking unemployed) also reported increased resting state connectivity between PCC and dorsolateral PFC following an intensive MBSR intervention.6 As noted in both studies, these results are consistent with training-related improvement in voluntary control of attention (top-down executive control) contributing to improved emotional regulation. Overall, these findings indicate that standard clinical mindfulness interventions may exert therapeutic effects by altering the state of specific brain regions (as indicated by changes in task-related activations) and brain networks (as indicated by connectivity changes).
FIGURE 1 AND COVER. Several small studies have utilized functional magnetic resonance imaging (fMRI) with emotional tasks (e.g., emotional faces, self-referential negative and positive words, self-referential negative and positive beliefs) prior to and following mindfulness interventions in patients with anxiety disorders (social anxiety disorder, generalized anxiety disorder, posttraumatic stress disorder) to identify clinically-relevant training-related changes. Areas of convergence across studies include increased activations that correlated with symptom reductions in dorsomedial prefrontal cortex (PFC), anterior cingulate cortex (ACC) and ventrolateral PFC/anterior insula (approximate locations overlaid on representative sagittal and axial MRIs, color coded by study).1–4 As noted by the authors of these studies, the results support treatment-related enhanced recruitment of areas contributing to emotional processing and regulation of emotional responding.
FIGURE 2. Studies have utilized both task-activated and resting state fMRI to identify pre-to-post mindfulness intervention functional connectivity changes that correlate with reductions in clinical symptoms. In a study of patients with generalized anxiety disorder, task-related (emotional faces) functional connectivity from the amygdala to medial PFC (orange) and dorsolateral PFC (orange) switched from negative (anticorrelated) to positive; these changes correlated with symptom improvement.2 Studies in patients with posttraumatic stress disorder and in highly stress community adults have reported increases in posttreatment resting state functional connectivity between the posterior cingulate cortex (PCC) and dorsolateral PFC (purple, blue).5,6 As noted in all studies, these results are consistent with training-related improvement in voluntary deployment of attention (top-down executive control) contributing to improved emotional regulation.
Only a few longitudinal studies have utilized voxel based morphometry and exploratory whole brain analyses to identify areas of structural change (gray matter density, gray matter concentration) associated with a standard mindfulness intervention (e.g., 8 weeks of MBSR), mostly in healthy individuals. There are only a few areas of convergence across studies (Figure 3). One study reported increased gray matter concentration in PCC, temporoparietal junction, cerebellar vermis/brainstem and lateral cerebellum following MBSR, whereas there were no areas of significant change in the control group.7 In a subset of participants in which a measure of psychological well-being was obtained prior to and following MSBR, percent change in well-being scores correlated with percent change in gray matter concentration in bilateral clusters in the pons (area of the locus coeruleus).60 A pilot study of a 6-week mindfulness intervention (Mindful Awareness Practices for Daily Living) in older adults with sleep disturbances (Pittsburg Sleep Quality Index >5) reported increased gray matter in precuneus and decreases in prefrontal and parietal areas, hippocampus, and thalamus following the intervention.8 A small RCT of MBSR in patients with Parkinson’s disease reported increased gray matter density in the caudate, thalamus, temporoparietal junction and occipital lobe following MBSR, whereas the two areas of significant increase in the control group were in the cerebellum.9 Although preliminary, these studies support the possibility of rapid initiation of structural brain changes by standard clinical mindfulness interventions.
FIGURE 3. A few longitudinal studies have utilized voxel based morphometry and exploratory whole brain analyses to identify areas of structural change (gray matter density, gray matter concentration) associated with a standard mindfulness intervention, mostly in healthy individuals. A few areas of convergence across studies are illustrated.7–9 One study reported increased gray matter concentration in PCC (brown), temporoparietal junction (brown), cerebellar vermis/brainstem and lateral cerebellum following MBSR.7 A pilot study in older adults with sleep disturbances reported increased gray matter in precuneus (pink) and decreases in prefrontal and parietal areas, hippocampus, and thalamus following the intervention.8 A small clinical trial in patients with Parkinson’s disease reported increased gray matter density in the temporoparietal junction (blue), occipital lobe, caudate, and thalamus lobe following MBSR.9 Although preliminary, these studies support the possibility of rapid initiation of structural brain changes by standard clinical mindfulness interventions.
In conclusion, there is a growing body of evidence supporting the helpful effects of secular mindfulness interventions for improving a wide range of fundamental processes in both physical and mental disorders. There is still much to be learned regarding the underlying neurobiological processes of therapeutic change. Longitudinal fMRI studies in specific patient populations will be particularly useful to elucidate similarities and differences across disorders.
1 : Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: effects on the self-referential brain network in social anxiety disorder. Front Hum Neurosci 2012; 6:295Crossref, Medline, Google Scholar
2 : Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. Neuroimage Clin 2013; 2:448–458Crossref, Medline, Google Scholar
3 : A pilot study of mindfulness-based exposure therapy in OEF/OIF combat veterans with PTSD: Altered medial frontal cortex and amygdala responses in social-emotional processing. Front Psychiatry 2016; 7:154Crossref, Medline, Google Scholar
4 : Neural Function Before and After Mindfulness-Based Cognitive Therapy in Anxious Adolescents at Risk for Developing Bipolar Disorder. J Child Adolesc Psychopharmacol 2016; 26:372–379Crossref, Medline, Google Scholar
5 : Altered default mode network (DMN) resting state functional connectivity following a mindfulness-based exposure therapy for posttraumatic stress disorder (PTSD) in combat veterans of Afghanistan and Iraq. Depress Anxiety 2016; 33:289–299Crossref, Medline, Google Scholar
6 : Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: A randomized controlled trial. Biol Psychiatry 2016; 80:53–61Crossref, Medline, Google Scholar
7 : Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res 2011; 191:36–43Crossref, Medline, Google Scholar
8 : Brain gray matter changes associated with mindfulness meditation in Older adults: An exploratory pilot study using voxel-based morphometry. Neuro 2014; 1:23–26Medline, Google Scholar
9 : Mindfulness based intervention in Parkinson’s disease leads to structural brain changes on MRI: a randomized controlled longitudinal trial. Clin Neurol Neurosurg 2013; 115:2419–2425Crossref, Medline, Google Scholar
10 : An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry 1982; 4:33–47Crossref, Medline, Google Scholar
11 : Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1992; 149:936–943Crossref, Medline, Google Scholar
12 : Mindfulness interventions. Annu Rev Psychol 2016Medline, Google Scholar
13 : Exploring the promise of mindfulness as medicine. JAMA 2015; 314:1327–1329Crossref, Medline, Google Scholar
14 : Mindfulness-based approaches: are they all the same? J Clin Psychol 2011; 67:404–424Crossref, Medline, Google Scholar
15 : Open, aware, and active: contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annu Rev Clin Psychol 2011; 7:141–168Crossref, Medline, Google Scholar
16 : The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clin Psychol Psychother 2002; 9:131–138Crossref, Google Scholar
17 : Mindfulness-based relapse prevention for alcohol and substance use disorders. J Cogn Psychother 2005; 19:211–228Crossref, Google Scholar
18 : The neuroscience of mindfulness meditation. Nat Rev Neurosci 2015; 16:213–225Crossref, Medline, Google Scholar
19 : Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res 2015; 78:519–528Crossref, Medline, Google Scholar
20 : Mindfulness training for health profession students: the effect of mindfulness training on psychological well-being, learning and clinical performance of health professional students: A systematic review of randomized and non-randomized controlled trials. Explore (NY) 2016; 13:26–45Crossref, Medline, Google Scholar
21 : Reporting of positive results in randomized controlled trials of mindfulness-based mental health interventions. PLoS One 2016; 11:e0153220Crossref, Medline, Google Scholar
22 : Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med 2016Google Scholar
23 : Mindfulness meditation and the immune system: a systematic review of randomized controlled trials. Ann N Y Acad Sci 2016; 1373:13–24Crossref, Medline, Google Scholar
24 : The emerging role of mindfulness meditation as effective self-management strategy, part 1: Clinical implications for depression, post-traumatic stress disorder, and anxiety. Mil Med 2016; 181:961–968Crossref, Medline, Google Scholar
25 : Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther 2016; 45:5–31Crossref, Medline, Google Scholar
26 : A mind-body program for older adults with chronic low back pain: A randomized clinical trial. JAMA Intern Med 2016; 176:329–337Crossref, Medline, Google Scholar
27 : Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA 2016; 315:1240–1249Crossref, Medline, Google Scholar
28 : Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain 2016; 157:2434–2444Crossref, Medline, Google Scholar
29 : Is it time to make mind-body approaches available for chronic low back pain? JAMA 2016; 315:1236–1237Crossref, Medline, Google Scholar
30 : Mindfulness-based stress reduction for long-term physical conditions: A systematic review. Aust N Z J Psychiatry 2016; 50:21–32Crossref, Medline, Google Scholar
31 : Mindfulness-based stress reduction in addition to usual care is associated with improvements in pain, fatigue, and cognitive failures among veterans with Gulf War illness. Am J Med 2016; 129:204–214Crossref, Medline, Google Scholar
32 : The efficacy of mindfulness-based interventions in primary care: A meta-analytic review. Ann Fam Med 2015; 13:573–582Crossref, Medline, Google Scholar
33 : Mindfulness-based cognitive therapy for patients with medically unexplained symptoms: a randomized controlled trial. Psychother Psychosom 2013; 82:299–310Crossref, Medline, Google Scholar
34 : Impact of mindfulness-based cognitive therapy on health care utilization: a population-based controlled comparison. J Psychosom Res 2014; 77:85–89Crossref, Medline, Google Scholar
35 : Mindfulness-based stress reduction in an integrated care delivery system: one-year impacts on patient-centered outcomes and health care utilization. Perm J 2014; 18:4–9Crossref, Medline, Google Scholar
36 : Mindfulness meditation practices as adjunctive treatments for psychiatric disorders. Psychiatr Clin North Am 2013; 36:141–152Crossref, Medline, Google Scholar
37 : Mindfulness- and Acceptance-based Interventions for Psychosis: A Systematic Review and Meta-analysis. Glob Adv Health Med 2016; 5:30–43Crossref, Medline, Google Scholar
38 : Mindfulness interventions for psychosis: a systematic review of the literature. J Psychiatr Ment Health Nurs 2017; 24:69–83Crossref, Medline, Google Scholar
39 : Effectiveness of psychological interventions in preventing recurrence of depressive disorder: meta-analysis and meta-regression. J Affect Disord 2015; 174:400–410Crossref, Medline, Google Scholar
40 : Efficacy of Mindfulness-Based Cognitive Therapy in Prevention of Depressive Relapse: An Individual Patient Data Meta-analysis From Randomized Trials. JAMA Psychiatry 2016; 73:565–574Crossref, Medline, Google Scholar
41 : Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: a meta-analysis of randomised controlled trials. PLoS One 2014; 9:e96110Crossref, Medline, Google Scholar
42 : Mindfulness-based cognitive therapy for recurrent major depression: A ‘best buy’ for health care? Aust N Z J Psychiatry 2016; 50:1001–1013Crossref, Medline, Google Scholar
43 : Mindfulness- and acceptance-based interventions for anxiety disorders: a systematic review and meta-analysis. Br J Clin Psychol 2012; 51:239–260Crossref, Medline, Google Scholar
44 : Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clin Psychol Rev 2016; 45:102–114Crossref, Medline, Google Scholar
45 : A systematic review of mindfulness and acceptance-based treatments for social anxiety disorder. J Clin Psychol 2015; 71:283–301Crossref, Medline, Google Scholar
46 : Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. J Consult Clin Psychol 2016; 84:427–437Crossref, Medline, Google Scholar
47 : An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: A systematic review. J Clin Psychol 2015; 71:935–963Crossref, Medline, Google Scholar
48 : Changes in mindfulness and posttraumatic stress disorder symptoms among veterans enrolled in mindfulness-based stress reduction. J Clin Psychol 2017; 73:201–217 Crossref, Medline, Google Scholar
49 : A randomized clinical trial of primary care brief mindfulness training for veterans with PTSD. J Clin Psychol 2016; 72:179–193Crossref, Medline, Google Scholar
50 : Simultaneous treatment of neurocognitive and psychiatric symptoms in veterans with post-traumatic stress disorder and history of mild traumatic brain injury: A pilot study of mindfulness-based stress reduction. Mil Med 2015; 180:956–963Crossref, Medline, Google Scholar
51 : How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev 2015; 37:1–12Crossref, Medline, Google Scholar
52 : Neural mechanisms of mindfulness meditation: bridging clinical and neuroscience investigations. Nat Rev Neurosci 2015; 16:439Crossref, Medline, Google Scholar
53 : Staying well: A follow up of a 5-week mindfulness based stress reduction programme for a range of psychological issues. Community Ment Health J 2015; 51:897–902Crossref, Medline, Google Scholar
54 : Meditation-related activations are modulated by the practices needed to obtain it and by the expertise: an ALE meta-analysis study. Front Hum Neurosci 2013; 6:346Crossref, Medline, Google Scholar
55 : Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev 2014; 43:48–73Crossref, Medline, Google Scholar
56 : The meditative mind: A comprehensive meta-analysis of MRI studies. Biomed Res Int 2015; 2015:419808.Crossref, Medline, Google Scholar
57 : Disentangling the neural mechanisms involved in Hinduism- and Buddhism-related meditations. Brain Cogn 2014; 90:32–40Crossref, Medline, Google Scholar
58 : Functional neuroanatomy of meditation: A review and meta-analysis of 78 functional neuroimaging investigations. Neurosci Biobehav Rev 2016; 65:208–228Crossref, Medline, Google Scholar
59 : Mindfulness meditation training alters stress-related amygdala resting state functional connectivity: a randomized controlled trial. Soc Cogn Affect Neurosci 2015; 10:1758–1768Crossref, Medline, Google Scholar
60 : Change in brainstem gray matter concentration following a mindfulness-based intervention is correlated with improvement in psychological well-being. Front Hum Neurosci 2014; 8:33Crossref, Medline, Google Scholar