Electrical Injury, Part II: Consequences
This report is the second of a two-part series on the mechanisms and consequences of electrical injury. Part I, addressing mechanisms of cellular injury and neuroimaging, appeared in the Summer 2009 issue of The Journal of Neuropsychiatry and Clinical Neurosciences.
There is no question that electrical injury can cause physical injury to the nervous system. Although thermal injuries were once presumed to be the primary cause of any cellular damage, electroporation is now thought to be the more common mechanism of injury ( Figure 1 ). Larger cells are more vulnerable to electroporation than small cells ( Figure 2 ). This may underlie the susceptibility of large neurons with very long axons. A common symptom of lightning strikes is a temporary paralysis (keraunoparalysis), usually of the lower limbs. 7 , 8 Other immediate symptoms of nerve dysfunction caused by electrical injury include parasthesia, hypertension, causalgia (persistent burning pain, allodynia, hyperpathia), and autonomic nervous system dysfunction. 8 , 9 Case reports of nerve conduction and neuroimaging studies have shown abnormalities in the days immediately following an electrical injury. 10 – 12 In some cases, these abnormalities resolve over time even while clinical symptoms remain. 13 In other cases the objective abnormalities may persist. 14 While electrical injuries clearly can cause measurable acute neurological injury and even death, the long-term sequelae for survivors are more controversial.


Incorrect assumptions associated with electrical injury have interfered with both research and treatment. These include the use of visible burns as a basis for judging injury severity, belief that high voltage exposures are more dangerous than low voltage, belief that psychological factors are the primary cause of poor outcomes, and overemphasis on the importance of secondary gain. 15 , 16 Electrical injury has been compared to mild traumatic brain injury (TBI) in terms of diffuse neuropsychological symptoms that may have a progressive or even delayed onset in the absence of abnormal imaging. 17 , 18 While affective disturbances are present following electrical injury, most research suggests these deficits generally have later onset (rather than precede) neuropsychological impairments. 15 , 19 – 22 Thus, electrical injury can lead to a neuropsychological syndrome with acute, prolonged, and delayed symptoms that can greatly interfere with a person’s functioning.
CLINICAL SEQUELAE OF ELECTRICAL EXPOSURE
Electrical injury sequelae are commonly divided into immediate and transient, immediate and prolonged or permanent, and delayed and progressive. 7 , 23 Acute symptoms such as loss of consciousness, confusion, numbness, tingling, and muscle spasms are indicators that an electrical injury has occurred, but may tell very little about the extent of neurological injury. However, evaluating outcome data on electrical injuries is difficult for a variety of complicating factors (e.g., differences in exposure and time since injury, challenges in determining the extent of relative injuries, variations in assessment procedures). Without careful attention to these parameters, synthesis of the literature and useful clinical prognoses cannot be made. While thousands of individuals experience an electrical injury annually, most do not seek medical attention and are thus unlikely to be included in research. Electrical injury survivors who do not seek immediate medical care may later experience delayed symptoms that prompt them to seek formal or informal help. Only the complicated acute or chronically symptomatic individuals will be referred for more intensive neuropsychological evaluations. As with other significant injuries, the process of recovery and rehabilitation from electrical injury is likely to show an uneven course. Collective clinical experience with electrical and lightning injuries indicates that for the group as a whole the most significant improvement should be in the first year, followed by continued improvement for approximately another 2 years before plateauing. 19 In contrast, the pattern in patients with long-term symptoms following electrical injury is of increasing symptoms for the first six to 18 months, followed by improvement that plateaus between 2 and 5 years. 22 It is important to recognize that functional decline may be due to a variety of mechanisms including delayed neurological insult, increased awareness of deficits identified during efforts to return to normal routines, and/or psychological reactions to the original injury. 7 , 23
Functional Neuroimaging
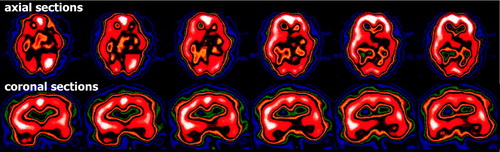
Very little research has examined functional changes the brain may undergo as a result of electrical injury. One case series of high-voltage electrical burn injuries assessed regional cerebral blood flow (single photon emission computed tomography, SPECT) at 3 weeks postinjury. 24 Two of the seven patients (29%) had areas of abnormal perfusion (one had hypoperfusion in the right mesial-temporal region, the other had hyperperfusion in the left caudate nucleus), despite normal CT. None of the patients had evidence of head trauma due to either current exposure or impact. A report of a single clinician’s 15 years of experience with electrical injury patients (5 months to decades after onset) noted that 80% (13/16) of electrical injury subjects in the chronic stage undergoing functional imaging (SPECT, positron emission tomography, PET) had abnormalities in areas that suggest “organic” deficits ( Figure 3 ). 22 This led him and others to conclude that electrical injury affects brain functioning more than brain structure. 5 , 22 A recent functional MRI (fMRI) study reported that patients with electrical injury (chronic stage) had significantly greater activation than healthy control subjects (matched for age and premorbid IQ) in sensorimotor areas (frontal and parietal eye fields, striatum) during a visual-motor task and in the frontal areas (middle frontal gyrus, motor and posterior cingulate cortices) during a spatial working memory task. 25 They had less activation than healthy control subjects in frontal areas (middle frontal gyrus, frontal eye fields, anterior cingulate cortex) during a procedural learning task. Task performance did not differ between the groups. The authors noted that these results suggest compensatory increases in brain activation to support performance in tasks requiring working memory and/or attentional control.
Clinical Symptoms
The data source must be carefully considered in comparing studies. For our discussion, only studies that grouped electrical injury survivors based on the time since their injury are included. Studies reporting the mean, median, and/or range of time since injury are excluded, as they combine survivors in the acute stage who may yet fully recover with those suffering chronic symptoms years after the electrical injury. In general, the symptoms of electrical injury are similar across time, although survivors in the acute stage may have greater confusion or altered mental states.
A major challenge in studying electrical injury is its relatively low frequency of occurrence. One group has developed a web-based survey in an effort to obtain information from a larger group with long-term symptoms (>3 months, N=89) following electrical injury. 26 , 27 Patients in which the likely current path included the neck/head (or was unknown), with possible mechanical TBI, and/or symptom resolution by 6 months were excluded from the analysis. The responses were grouped by two exposure parameters, voltage (110/220, 440–480, >1000) and loss of consciousness (none, <1 minute, >1 minute). Physical symptoms commonly reported by all groups included general weakness, muscle aches and muscle spasms. Neuropsychological symptoms commonly reported by all groups included problems with attention, concentration and short term memory. Of particular interest, the percentage of each group reporting particular symptoms did not appear to be related to either exposure parameter. As noted by the authors, this is a select sample that may differ from the broad or common experience of electrical injury. The results are generally similar, however, to other studies. A survey of electricians found the most common long term symptoms following electrical injury were fatigue, muscle and joint pain, and sensitivity to cold and heat. 28 In comparison to electricians with no history of electrical exposure, those with electrical injuries (N=63) endorsed more symptoms on the Neuropsychological Symptom Checklist. 15 , 21 Highly endorsed physical and neuropsychological symptoms were similar to those reported in the web-based studies. Symptoms often endorsed by patients with electrical injuries in one clinical practice (N=24) included pain and problems with memory and concentration. 22 Two studies found the postacute survivors (>3 month) to have worse self-reported symptoms than the acute survivors (<3 months). 18 , 21 Thus, the profile of electrical injury suggests early signs of neurological dysfunction that in many cases persist or worsen over time.
Two studies have provided longitudinal data on groups of electrical injury survivors. 29 , 30 The earlier study followed 16 patients for at least 5 years postinjury and found “generalized cerebral dysfunction.” 29 The recent study followed a cohort of electrical injury survivors (N=134) from ER admission to 1 year. 30 All subjects were reported to be initially asymptomatic other than the presence of risk factors for late arrhythmias (e.g., transthoracic current path, loss of consciousness, voltage source ≥1000 V, abnormal initial ECG) requiring 24 hours of cardiac monitoring. All levels of electrical exposure were included. Assessments (telephone survey containing both open-ended and specific questions) were obtained at 1–3 months and 1 year following injury. At the first assessment, 26% (30/114) reported the onset of at least one neurological or neuropsychological symptom (e.g., weakness, pain, numbness, tingling sensations, memory loss). At the second assessment, 28% (24/86) reported the presence of neurological and/or neuropsychological symptoms. Of these, 50% were symptomatic at the first assessment and 50% were not. There were no differences in symptom rates at either time point related to type or severity of electrical exposure (e.g., domestic or industrial, greater than or less than 1000 V, presence or absence of burns, presence or absence of loss in consciousness, level of muscle injury as indicated by initial creatine phosphokinase level). As noted by the authors, these results support the presence of both early and delayed-onset neurological and/or neuropsychological symptoms in a substantial minority following electrical injury.
Self-report data are problematic for many reasons, particularly the tendency for patients to underestimate the prevalence of premorbid neuropsychological symptoms such as forgetfulness, irritability, fatigue, and sleep disturbances. 31 Formal neuropsychological testing provides more objective evidence. Common deficits in patients with electrical injuries in one clinical practice (N=26) included processing speed (62%), auditory (62%) and visual (35%) memory, verbal learning (54%) and fluency (46%), concentration (46%), and attention (42%). 22 One study compared neuropsychological performance of patients with high voltage (electrical and lightning) injuries to patients with TBI (matched for gender, age, education, time since injury and injury severity). 17 The overall cognitive performances of the two groups were similar. Verbal memory deficits were found in the electrical injury group at all times examined (<1 month, 1–6 months, and >6 months). Such results clearly demonstrate neuropsychological dysfunction in at least some of the electrical injury survivors.
Psychiatric sequelae following electrical injury have also been documented. Electrical injury survivors report high levels of depression, anxiety, PTSD symptoms, irritability, somatization, mood swings, and personality changes. 5 , 17 , 18 , 20 , 21 , 26 , 27 , 30 , 32 – 34 Significantly, several studies have found that psychological factors such as depression or premorbid psychiatric history do not account for neuropsychological symptoms post electrical injury. 20 – 22 , 35 – 37 However, in one study electrical injury survivors who met criteria for two psychiatric diagnoses reported more neuropsychological symptoms than survivors who met criteria for no or only one psychiatric diagnosis. 38 Psychiatric sequelae of electrical injury may not manifest immediately after the injury. Cross-sectional studies have reported higher incidence of both specific symptoms and formally diagnosed disorders at later times following injury (>3 months) compared to earlier periods (<3 months), as well as persistence of symptoms years after electrical injury. 15 , 18 , 21 , 34 , 38 Longitudinal studies have reported depression and associated psychosocial complaints, with indications of increased symptoms at 1 year compared to a few months after injury. 29 , 30 Such findings suggest the progression or development of chronic psychiatric impairments.
While the origin of the dysfunction associated with electrical injury may be controversial, survivors clearly have difficulty returning to their previous level of functioning. It is often in the process of returning to work following an electrical injury that many survivors first become aware of their deficits. This may be one reason for the “appearance” of symptoms several months postinjury. Studies suggest only 25–50% of electrical injury survivors are able to return to their previous employment while a third could not return to work at all. 32 , 33 Return to work may be impacted by multiple factors including neurological deficits, neuropsychological impairments, and/or psychological reactions. Electrical injury survivors attempting to return to work may also find a psychologically threatening and/or socially unsupportive workplace. An electrical injury may be similar to a single trial of aversive conditioning that is difficult to extinguish. 39 The survivor may feel fearful about returning to what may now be perceived as a dangerous environment, resulting in a cascade of self-defeating thoughts. 40 Coworkers, supervisors, and the survivor may contribute to these thoughts by overtly or covertly blaming the survivor for the electrical injury (e.g., by attributing dangerous, careless, or unprofessional traits to the injured worker). 41 Such beliefs, particularly when reinforced through social interactions, can impede recovery. In addition, electrical injury survivors frequently have a difficult time getting their deficits acknowledged as serious, which may also impede their recovery. 39 Rehabilitation following any significant injury is a difficult and trying process that can result in poor adjustment even when the original injury heals. 42 The inclusion of a vocational evaluation as part of the rehabilitation plan is recommended. 41
CONCLUSION
Ultimately, electrical injury reflects a trauma that includes both neurological and psychological aspects. Each has significant overlap and interaction with the other, resulting in a complex syndrome of inattention, memory lapses, depression, anxiety, muscle weakness, fatigue, extremity numbness or tingling, pain, and sleep disturbances that greatly resembles mild TBI. Historically, the severity of electrical injury often was not recognized and treatment not sought, especially when the acute symptoms were mild. Given the evidence for late-onset deficits, clinicians should consider screening for electrical injury in all initial patient intakes. Future research will need to expand the understanding of mechanisms and consequences of electrical injury. Mounting evidence suggests that sequelae of electrical injury, like mild TBI, are difficult to predict based on acute symptoms or injury characteristics but are likely to occur in a significant minority of victims. Furthermore, the impact of electrical injuries on the developing nervous system of a child is not known. 40 Additional longitudinal studies are sorely needed to determine the progression of electrical injuries over time.

1. Lee RC, Zhang D, Hannig J: Biophysical injury mechanisms in electrical shock trauma. Annu Rev Biomed Eng 2000; 2:477–509Google Scholar
2. Tieleman DP: The molecular basis of electroporation. BMC Biochem 2004; 5:10Google Scholar
3. Teissie J, Golzio M, Rols MP: Mechanisms of cell membrane electropermeabilization: a minireview of our present (lack of?) knowledge. Biochim Biophys Acta 2005; 1724:270–280Google Scholar
4. Lee RC: Cell injury by electric forces. Ann N Y Acad Sci 2005; 1066:85–91Google Scholar
5. Duff K, McCaffrey RJ: Electrical injury and lightning injury: a review of their mechanisms and neuropsychological, psychiatric, and neurological sequelae. Neuropsychol Rev 2001; 11:101–116Google Scholar
6. Rai J, Jeschke MG, Barrow RE, et al: Electrical injuries: a 30-year review. J Trauma 1999; 46:933–936Google Scholar
7. Cherington M: Neurologic manifestations of lightning strikes. Neurology 2003; 60:182–185Google Scholar
8. Jost WH, Schonrock LM, Cherington M: Autonomic nervous system dysfunction in lightning and electrical injuries. NeuroRehabilitation 2005; 20:19–23Google Scholar
9. Danielson JR, Capelli-Schellpfeffer M, Lee RC: Upper extremity electrical injury. Hand Clin 2000; 16:225–234Google Scholar
10. Stockwell B, Bellis G, Morton G, et al: Electrical injury during “hands on” defibrillation: a potential risk of internal cardioverter defibrillators? Resuscitation 2009; 80:832–834Google Scholar
11. Aslan S, Yilmaz S, Karioglu O: Lightning: an unusual cause of cerebellar infarction. Emerg Med J 2004; 21:750–751Google Scholar
12. Kalita J, Jose M, Misra UK: Myelopathy and amnesia following accidental electrical injury. Spinal Cord 2002; 40:253–255Google Scholar
13. Kleiter I, Luerding R, Diendorfer G, et al: A lightning strike to the head causing a visual cortex defect with simple and complex visual hallucinations. J Neurol Neurosurg Psychiatry 2007; 78:423–426Google Scholar
14. Cherington M, Yarnell PR, Lane J, et al: Lightning-induced injury on an airplane. J Trauma 2002; 52:579–581Google Scholar
15. Pliskin NH, Fink J, Malina A, et al: The neuropsychological effects of electrical injury. Ann N Y Acad Sci 1999; 888:140–149Google Scholar
16. Muehlberger T, Vogt PM, Munster AM: The long-term consequences of lightning injuries. Burns 2001; 27:829–833Google Scholar
17. Barrash J, Kealey GP, Janus TJ: Neurobehavioral sequelae of high voltage electric injuries: comparison with traumatic brain injury. Appl Neuropsychol 1996; 3:75–81Google Scholar
18. Wicklund AH, Ammar A, Weitlauf JC, et al: MMPI-2 patterns in electrical injury: a controlled investigation. Clin Neuropsychol 2008; 22:98–111Google Scholar
19. Primeau M, Engelstatter GH, Bares KK: Behavioral consequences of lightning and electrical injury. Semin Neurol 1995; 15:278–285Google Scholar
20. Janus TJ, Barrash J: Neurologic and neurobehavioral effects of electric and lightning injuries. J Burn Care Rehabil 1996; 17:409–415Google Scholar
21. Pliskin NH, Capelli-Schellpfeffer M, Law RT, et al: Neuropsychological symptom presentation after electrical injury. J Trauma 1998; 44:709–715Google Scholar
22. Andrews CJ: Further documentation of remote effects of electrical injuries, with comments on the place of neuropsychological testing and functional scanning. IEEE Trans Biomed Eng 2006; 53:2102–2113Google Scholar
23. Cherington M: Central nervous system complications of lightning and electrical injuries. Semin Neurol 1995; 15:233–240Google Scholar
24. Deveci M, Bozkurt M, Arslan N, et al: Nuclear imaging of the brain in electrical burn patients. Burns 2002; 28:591–594Google Scholar
25. Ramati A, Pliskin NH, Keedy S, et al: Alteration in functional brain systems after electrical injury. J Neurotrauma 2009; Epub ahead of printGoogle Scholar
26. Spies C, Trohman RG: Narrative review: Electrocution and life-threatening electrical injuries. Ann Intern Med 2006; 145:531–537Google Scholar
27. Morse JS, Morse MS: Diffuse electrical injury: comparison of physical and neuropsychological presentation in males and females. J Psychosom Res 2005; 58:51–54Google Scholar
28. Tkachenko TA, Kelley KM, Pliskin NH, et al: Electrical injury through the eyes of professional electricians. Ann N Y Acad Sci 1999; 888:42–59Google Scholar
29. Hooshmand H, Radfar F, Beckner E: The neurophysiological aspect of electrical injuries. Clin Electroencephalogr 1989; 20:111–120Google Scholar
30. Bailey B, Gaudreault P, Thivierge RL: Neurologic and neuropsychological symptoms during the first year after an electric shock: results of a prospective multicenter study. Am J Emerg Med 2008; 26:413–418Google Scholar
31. Iverson GL, Lange RT: Examination of “postconcussion-like” symptoms in a healthy sample. Appl Neuropsychol 2003; 10:137–144Google Scholar
32. Noble J, Gomez M, Fish JS: Quality of life and return to work following electrical burns. Burns 2006; 32:159–164Google Scholar
33. Theman K, Singerman J, Gomez M, et al: Return to work after low voltage electrical injury. J Burn Care Res 2008; 29:959–964Google Scholar
34. Singerman J, Gomez M, Fish JS: Long-term sequelae of low-voltage electrical injury. J Burn Care Res 2008; 29:773–777Google Scholar
35. van Zomeren AH, ten Duis HJ, Minderhoud JM, et al: Lightning stroke and neuropsychological impairment: cases and questions. J Neurol Neurosurg Psychiatry 1998; 64:763–769Google Scholar
36. Kelley KM, Tkachenko TA, Pliskin NH, et al: Life after electrical injury: risk factors for psychiatric sequelae. Ann N Y Acad Sci 1999; 888:356–363Google Scholar
37. Pliskin NH, Ammar AN, Fink JW, et al: Neuropsychological changes following electrical injury. J Int Neuropsychol Soc 2006; 12:17–23Google Scholar
38. Ramati A, Rubin LH, Wicklund A, et al: Psychiatric morbidity following electrical injury and its effect on cognitive functioning. Gen Hosp Psychiatry 2009; 31:360–366Google Scholar
39. Heilbronner RL, Pliskin NH: Psychological issues on the neurorehabilitation of electric injuries. NeuroRehabilitation 1999; 13:127–132Google Scholar
40. Primeau M: Neurorehabilitation of behavioral disorders following lightning and electric trauma. NeuroRehabilitation 2005; 20:25–33Google Scholar
41. Capelli-Schellpfeffer M: Roadblocks to return to work after electrical trauma. NeuroRehabilitation 2005; 20:49–52Google Scholar
42. Heilbronner RL: Rehabilitation of the neuropsychological sequelae associated with electrical trauma. Ann N Y Acad Sci 1994; 720:224–229Google Scholar



