Cranial Electrotherapy Stimulation Reduces Aggression in a Violent Retarded Population: A Preliminary Report
Abstract
Nine aggressive, retarded patients refractory to conventional care at a maximum security hospital were given a 3-month course of cranial electrotherapy stimulation. Aggressive episodes declined 59% from baseline; seclusions were down 72%; restraints were down 58%; and use of prescribed-as-needed sedative medications decreased 53%. The most dramatic change was that of a disorganized, schizophrenic patient whose aggressive episodes declined from 62 to 9, seclusions from 53 to 8, restraints from 9 to 1 and PRNs from 25 to 1. No patients discontinued cranial electrotherapy stimulation (CES) because of side effects. This preliminary report indicates that CES appears to be an efficacious, safe, and cost-effective addition to the treatment regimen in this patient population.
A recent annotated bibliography by Kirsch1 details 126 human and 29 experimental animal studies conducted over the past 40 years. The clinical, neurochemical, and electrophysiological studies mentioned below are in the list of references that follows this article.
Medication resistant schizophrenic, and affective psychosis patients have responded to cranial electrotherapy stimulation (CES) and a sham-controlled study on closed-head injury patients showed diminished anger, hostility, and confusion. Neurochemical studies have demonstrated the following CES effects: ↑Plasma and cerebral spinal fluid (CSF) beta-endorphins; ↑activity of the enzyme MAOb; and ↑CSF serotonin.
Using implanted electrodes, Cox and Heath2 noted well-developed alpha rhythms, previously undetected, in a medication resistant, depressive patient. In normal volunteers, Shroeder and Barr,3 were able to record artifact-free electroencephalogram (EEG) characteristics during both 0.5 Hz and 100 Hz CES, noting a significant downward shift in alpha power band distribution.
METHOD
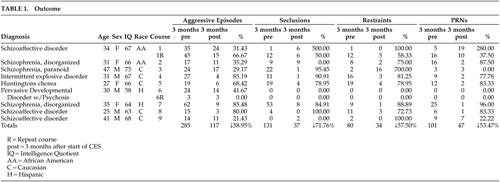
Patients had been hospitalized in the maximum security unit of North Texas State Hospital at Vernon (NTSH-V) from a few months to 14 years (two patients). Eight of the nine patients had been sent from other state hospitals as manifestly dangerous and one had charges pending. Diagnoses, ages, and IQs are listed in Table 1. Comorbid personality disorders (borderline and or antisocial) were evident in five cases, and epilepsy had been diagnosed in four of the nine patients.
During the first 3 months of treatment, no medication changes occurred in six of the patients. One patient had adjustments in clozapine dosage, and another patient’s thiothixene was increased, with aripiprazole being substituted for ziprasidone. One patient was on no medication at all (case 1, below).
The patients received two hourly treatments daily, using the Alpha-Stim 100 device (Electromedical Products International; www.alpha-stim.com). This device produces either a 0.5 Hz or a 100 Hz bipolar asymmetric modified square waveform. The maximum current is 600 μA. Moistened electrodes are clipped to the patients ears, and the current is set slightly below the level at which the patient feels a tingling sensation.
CASE REPORTS
Cited in this article are two cases in which the improvement noted was independent of medication changes.
Subject 1
A 24-year-old, mildly retarded Caucasian female was thought to be experiencing personality changes due to Huntington’s disease, from which her father had died in his mid 40s. The patient had been assaulting others since childhood, with her symptoms worsening at age 13. She was arrested at age 18 for driving a car at a high speed into another vehicle. Highly promiscuous, she had six children, all of whom were in the care of others. The patient was transferred to NTSH-V maximum-security unit after a 6-week period, during which she was assaultive 14 times, with one of these attacks resulting in a staff member suffering a dislocated jaw. Though she was not psychotic, efforts to diminish her violence with medications (e.g., valproic acid, lithium, quetiapine, and olanzapine) were unsuccessful and were discontinued. She never showed remorse after her assaults, and she responded to our inquires with, “I do not know” or “I just wanted to.” But she did admit a thrill at carrying out her attacks. In the 2 months prior to starting CES, she carried out 19 episodes of unprovoked and unpredictable assaults, including two attacks on her physician. In that period, she was restrained and secluded 19 times, and she received 12 haloperidol injections. One hundred Hz CES was initially provided an hour a day, then twice a day for 45 minutes to 1 hour per treatment. She was not taking psychoactive medications during the 2 months of 100 Hz CES treatment. Her aggressive episodes dropped to six, requiring restraint and seclusion four times. And she received only two haloperidol injections during the 2-month period. Her dyskinetic movements disappeared during the period of active treatment. At the end of the 2-month period, she began refusing CES. Shortly thereafter, she reported erotomanic and other delusions as well as auditory hallucinations. After CES was discontinued, she resumed her assaultive behavior at its pretreatment frequency.
Subject 2
The patient is a 38-year-old, unmarried citizen of Mexico undergoing her second hospitalization at NTSH-V. This was not the first time she had been sent from a state hospital as manifestly dangerous. Prior to this admission she had committed 45 acts of aggression, resulting in 14 injuries at the previous state hospital. She also continued biting, hitting, exposing herself, urinating, and defecating in the seclusion room, and she was too disorganized to participate in any programming. She has spent all but 6 months of the past decade in Texas state hospitals.
Born to impoverished parents in Mexico, the patient was the sixth of seven children. When she was 2 years old, her mother died from complications of childbirth. Her alcoholic father was cold and distant with her and her siblings. She attended school only through the third grade. While attending school, she could not get along with other students and learned very little. She cannot read or write in English or Spanish. She has been diagnosed as mildly retarded. The patient is said to have spent her childhood running loose in the streets and she could not keep friends because of her explosive temper. At age 15, she was hospitalized in Mexico and diagnosed as schizophrenic. The family had no money for her medications, which were discontinued after her multiple hospitalizations in Mexico. At age 23, she delivered a child who was taken from her by the Mexican authorities because of her mental condition. Traumatized by this experience, it wasn’t long before she kidnapped the infant of another woman. She spent 6 months in jail, during which time she had no psychiatric treatment. Her family brought her to the U.S. when she was 24 years of age, and she began a decade of hospitalization within 1 year of being in the country. In a prior hospitalization, she had stabilized on clozapine, but unfortunately her seizures increased. Additionally, she had adverse electrocardiogram (EKG) changes (QTc prolongation problems), resulting in discontinuation of the medicine. No other medication has had much effect on her relentlessly assaultive and disorganized behavior. On this admission, she was noted to be babbling incoherently, bizarre, malodorous, and disheveled. Such sentences as she spoke were meaningless compilations of words, which seemed to be in a “bizarre language unknown to anyone.” In the 3 months prior to starting CES, the patient was assaultive 62 times, requiring seclusion on 53 occasions, was restrained 9 times, and received 25 injections of antipsychotic medicine. Shortly before CES was started (at the 0.5 Hz frequency, 1 hour twice daily) the 60 mg/day of haloperidol was discontinued, leaving her on lithium, valproic acid, phenytoin and aripiprazole. In the first 3 months of CES therapy the number of aggressive episodes dropped from 62 to 9, seclusions went down from 53 to 8, restraints declined from 9 to 1, and she required only one sedative injection, down from 25 before CES therapy. Her interactions became much more appropriate with peers, and she no longer urinated and smeared feces in the seclusion room even when she required seclusion. In the second month of CES therapy, there were no seclusions or restraints. In the third month, only three personal restraints and one seclusion were implemented. She began attending classes and therapies and was able to be housed in a dormitory for less aggressive patients. Overall, the patient seemed less demented as CES continued, and she was no longer as disorganized in her thinking.
RESULTS
Table 1 and Figure 1 show the four parameters for 3 months before CES and during the first 3 months of active treatment. In aggregate, aggressive episodes for the nine cases declined 59% over baseline. seclusions were down 72%; restraints were down 58%; and sedative medications required decreased by 53%. Table 2 demonstrates statistical significance for three of the four parameters, the fourth (restraints) being close to significant. No patient discontinued CES because of side effects. Six patients have continued CES, the longest being patient number 6 who has been treated for 3 years. Not captured in the above data are the cognitive improvements in the most disorganized cases,2,3 particularly reflected in interpersonal relatedness. Of the nine cases, four have left the hospital: three to less restrictive facilities and one, having regained competency, was returned to court for judicial processing. Two of the discharged cases have continued CES at other facilities, and both continue to do well.
DISCUSSION
In this group of violent, refractory patients, it is surprising that CES made any difference in their behavior. Though some patients had modest declines in the absolute number of aggressive episodes, diminished severity lead to fewer restraints, seclusions, and sedative medications. In some cases, (e.g., case #3) brief personal hold was enough to allow the patient to regain control without having to be secluded or medicated. In a time when hospitals are under pressure to reduce seclusion and restraint, it appears that CES is useful in diminishing the necessity of these procedures in persistently aggressive patients. In the first 3 months of CES use on the unit for retarded patients (housing 7 of these 9 cases), staff injuries declined 50%; patient injuries dropped by 66%; and the cost of medications was $14,000.00 less, with no change in census. Subject 1 had a better response to the second course of CES, suggesting a cumulative benefit that has also been apparent in the seven patients who continued the treatment after the initial 3-month period.
As with many medications, the effects of CES are empirical. It is possible that CES augments the benefits of antipsychotic and mood stabilizing medications. Further study would be needed to determine which, if any, of the previously reported neurochemical and electrophysiological mechanisms might be responsible for the improvement discussed.
CONCLUSION
These nine retarded, aggressive, medication resistant patients have benefited substantially from CES. Other cases at NTSH-V, quite similar but slightly less severe than the nine cases we studied, have also responded briskly to CES. While controlled studies should be undertaken, CES appears to be an efficacious, safe, and cost-effective addition to the treatment regimen in this patient population.
 |
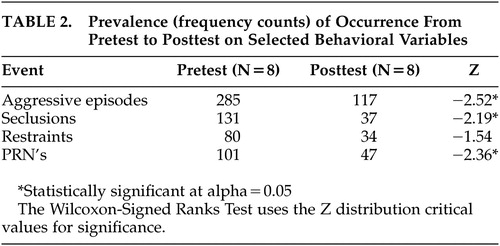 |
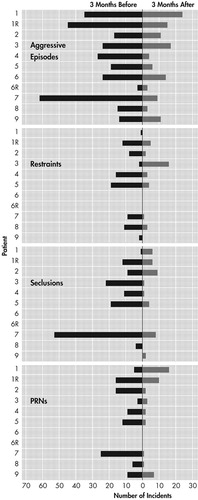
FIGURE 1. Before and After CES
CES=cranial electrotherapy stimulation
1 Kirsch DL: The Science Behind Cranial Electrotherapy Stimulation. Edmonton, Alberta, Medical Scope Publishing, 2002Google Scholar
2 Cox A, Heath RG: Neurotone therapy: a preliminary report of its effect of electrical activity of forebrain structures. Dis Nerv Sys 1975; 36:245–247Medline, Google Scholar
3 Schroeder MJ, Barr RE: Quantitative analysis of electroencephalogram during cranial electrotherapy stimulation. Clinical Neurophysiology 2001; 112:2075–2083Crossref, Medline, Google Scholar