Topiramate Effect in Catatonia: A Case Series
While antipsychotic medications provide relief of the positive symptoms of psychosis, hallucinations, and delusions, the negative symptoms tend to respond only to the new atypical antipsychotics. Neither typical nor atypical antipsychotic drugs have been shown to be as consistently useful in the treatment of catatonia. Approaches that are often helpful to patients suffering from catatonic agitation include benzodiazepines, such as lorazepam, and electroconvulsive therapy (ECT). 1 As benzodiazepine therapy for catatonia is not always quickly effective and ECT is not acceptable to all patients or their families, any new treatment approach for catatonia will be an advantage. We report four cases in which patients suffering from schizophrenia or bipolar illness with catatonia obtained fairly rapid relief with topiramate after failing to respond to benzodiazepine and antipsychotic therapy.
CASE REPORTS
Case 1
A 19-year-old Caucasian woman with a 3-year history of chronic psychotic illness with auditory hallucinations and paranoid and referential delusions had been stable with risperidone therapy at a dose of 4 mg daily. The patient was compliant by all accounts. However, she later became agitated, and this agitation was, most likely, the result of Cannabis abuse, which was confirmed by laboratory testing. She was committed to a local hospital where she was treated with risperidone, which had until then given her very good symptom relief. During this episode, the patient deteriorated further and began to demonstrate catatonic mutism, negativism, and occasional posturing. Lorazepam was added in low dose (about 3 mg daily in divided doses). At the family’s request, the patient was transferred to our facility, in part to explore other treatment options, including ECT. After arrival at our facility, the patient and her family decided against a trial of ECT, and a trial of high-dose lorazepam, up to 9 mg daily, was offered. This was well tolerated, but signs of catatonic agitation, including posturing and catalepsy, only worsened. Marked sedation made further dose increases an impractical option. A trial of divalproex was unhelpful and was poorly tolerated due to gastrointestinal side effects. On the basis of an argument that glutamate antagonism might offer further relief of catatonic agitation without excess sedation and because of a recent report on the success of topiramate in treatment of schizophrenia, a trial of topiramate was offered. Topiramate dose was gradually titrated from 25 mg b.i.d. to 100 mg b.i.d. The patient’s catalepsy, posturing, and episodic immobility remitted as the daily dose reached 200 mg per day, and lorazepam was gradually withdrawn. Risperidone therapy was continued with topiramate as the patient was discharged home in the care of her family. At the 3-month follow-up, the patient had experienced no recurrence of catatonic agitation, and at the 1-year follow-up, she had improved enough to return to college.
Case 2
A 19-year-old Caucasian woman with only a 1-year history of psychotic and depressive illness with bizarre delusions had nine prior hospitalizations at area hospitals, during the span of her 1-year history. In addition, the patient had a history of violent suicide attempts, most recently by trying to sever one hand with her father’s circular saw. When the patient was transferred to our unit after surgical reattachment of her injured hand, she was cooperative with postoperative care, but she was mute and immobile for a period and was observed to demonstrate posturing and waxy flexibility by the third morning of her stay at our facility. She was already receiving high dose benzodiazepine therapy with the olanzapine that she had been taking as an outpatient before the crisis that culminated in the severing of her hand. The patient already had failed to improve during adequate trials of risperidone, quetiapine, ziprasidone, most of them in combination with lithium or divalproex. At the time of admission, the patient was compliant with divalproex 1,000 mg daily and olanzapine 15 mg daily, according to both the patient and to her parents, with whom she lived. The working diagnosis to date had been bipolar disorder, mixed with psychotic features, although her flat affect and the bizarre character of her delusions forced us to consider schizophrenia in the differential diagnosis. A trial of clozapine was offered and accepted, and the patient stated it seemed to help her more than the other agents she had taken. Episodic muteness and immobility continued despite this improvement and continued lorazepam therapy. Our experience with the patient prompted another recommendation for a trial of topiramate, in lieu of divalproex. Signs of catatonia disappeared as the daily dose passed 150 mg, and the dose was again titrated to 200 mg daily. The patient continued to improve and was discharged home on topiramate at the same dose and clozapine 300 mg daily. She did well for approximately 3 weeks before being hospitalized for suicidal behavior again.
Case 3
A 61-year-old woman with a history of bipolar disorder (type I) since age 20 had been fairly stable until suffering a myocardial infarction and undergoing coronary artery bypass graft surgery. She then suffered a recurrence of mania with paranoid delusions that developed despite compliance with lithium carbonate and quetiapine therapy, with proven therapeutic levels of lithium of 1meq/liter. She appeared to stabilize with the addition of divalproex sodium but again became psychotic and agitated when her sternotomy wound from bypass surgery was complicated by sternal osteomyelitis. While still receiving intravenous antibiotics, she was transferred to the psychiatry service due to disorganized, agitated behavior, with extreme negativism—so great that she refused to rise from bed or even to feed herself. The development of catalepsy convinced us that her condition was a catatonic agitation. High-dose lorazepam led only to sedation, even when quetiapine was discontinued. A trial of topiramate was well tolerated, and led to gradual resolution of signs of catatonia after the daily dose reached 200 mg. The patient developed stupor with fever after antibiotic therapy was discontinued, and all psychotropic medications were stopped. Medical evaluation revealed a urinary tract infection that was subsequently treated. As the stupor and delirium cleared, the patient again demonstrated agitation, extreme negativism, and catalepsy. Topiramate therapy was resumed and again titrated to 200 mg daily. Signs of catatonic agitation remitted, and the patient was able to return home to care for herself.
Case 4
A 65-year-old woman with chronic schizophrenia and a history of repeated hospitalizations for catatonic states with catalepsy and muteness was admitted to the medical service of the hospital. She was dehydrated and had early sepsis from sacral decubitus ulcers that developed during immobility caused by a new recurrence of catatonia. When medically stable, she was transferred to the psychiatry service. High dose lorazepam therapy, up to 12 mg daily, made no difference in her mute immobility, nor did the addition of divalproex up to 1,500 mg daily (valproate level was 95 mcg/ml). A trial of topiramate was made, and the patient began to speak, feed herself, and ambulate as the dose reached 200 mg daily. The patient continued to receive topiramate therapy and was well for about 1 year, during which time lorazepam was gradually withdrawn. She suffered a recurrence of catatonic agitation with mute immobility, posturing, catalepsy, and gegenhalten. Symptoms improved gradually during the second hospitalization with continuation of topiramate 400 mg daily and a daily dose of lorazepam totaling 12 mg daily.
During the same period of time, two patients were seen with catatonia who responded to lorazepam therapy, and two who were treated with ECT. There were no patients with catatonia who were treated with topiramate first, and no patients who were treated with topiramate who did not experience remission.
DISCUSSION
Catatonia is a long recognized and well-described phenomenon whose pathophysiology remains largely a mystery. 1 It can occur in the setting of other recognized psychiatric illnesses but always is distinguished by characteristic signs and symptoms, and it has been proposed that it should be classified separately from other psychiatric disease. 1
Catatonia is common, and one recent report estimated its prevalence at about 90,000 cases annually. 1 The syndrome has been reported in adolescents younger than our patients described in the present study.
Catatonia can be characterized in three separate domains: motor, affective, and behavioral symptoms. 1 Our patients presented with motor immobility or catalepsy and unusual behavioral alterations of negativism, mutism, and posturing. The final dimension of affective symptoms are best characterized as crippling, uncontrollable anxiety, which was present in all of our cases but difficult to quantify.
The syndrome of catatonia is associated with schizophrenia and bipolar illness, and studies appear to show that it is more often associated with mania than with any other disease state. 4 , 5 , 6 The association with several disease states has led to some nosological confusion, so the term catatonia was not to be found in several recent editions of the Diagnostic and Statistical Manual until DSM–IV. 7 It is now coded as a feature of schizophrenia or mania. When catatonia occurs in association with autism 8 , 9 , 10 or medical problems, nosology remains problematic.
The presence of recognizable syndromes of catatonic agitation make possible the construction of rating scales, at least for research purposes. 11 , 12 , 13 , 14 The application of rating scales clinically is sometimes difficult because of the variable clinical picture, but the research has done much to help refine our understanding and to develop diagnostic criteria.
The most reliable treatment for catatonia remains benzodiazepines. 15 High doses are required, usually for long periods, and they do not always work, but they help more often than any other intervention that has been reported, except perhaps ECT. The facts that benzodiazepines are preferential GABA-A agonists and work so well provide important clues to the neurobiology of catatonic agitation. Other GABA agonist drugs such as the anticonvulsants valproic acid and carbamazepine have also been reported to help patients recover from catatonia. 16 , 17
All of these drugs had been tried and failed to help the patients described in this study, and all of the patients or family members had rejected the offer of ECT. Topiramate was considered next as an anticonvulsant with similar GABA-ergic properties compared to carbamazepine and valproate and with an additional antiglutamatergic property that might be useful. Topiramate had already been reported as useful in a few cases of schizophrenia, some of which included some features of catatonia 18 ( Table 1 ).
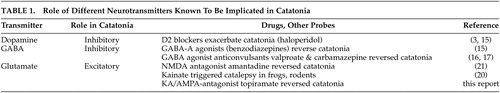 |
The neurochemical hypothesis proposed by Northoff 19 in 2002 focuses on four neurotransmitters: dopamine (DA), gamma-aminobutyric acid (GABA), glutamate, and serotonin (5-HT). Evidence points to a central role for GABA, with down-regulation of GABA-A receptors. In fact the GABA-A receptor agonist/modulator lorazepam successfully treats 60%–80% of all acutely catatonic patients. Northoff 19 suggests that motor and affective symptoms might be more amenable to GABA agonists than are behavioral symptoms, which may be affected by an altered relationship between GABA-ergic and glutamatergic neurotransmission One clue as to how this might happen was demonstrated by catatonic—looking immobility in rats injected with kainic acid. 20 An additional clue is the demonstration that the NMDA antagonist amantadine can successfully treat catatonia. 21 If the kainic acid-treated rat model approximates the human catatonic state, then excessive glutamatergic binding at KA receptors may trigger or help drive catatonic agitation and may help explain our finding that topiramate terminated catatonic agitation in four patients whose catatonia had been refractory to treatment with benzodiazepines, antipsychotic tranquilizers, and the GABA-ergic anticonvulsants valproate and carbamazepine. 22
An additional clue to the role of different glutamate receptors may be the observation that AMPA-kines, drugs that modulate the AMPA receptor complex also enhance NMDA receptor function. It is thus possible that AMPA receptor antagonists may attenuate NMDA receptor function. 23 , 24 There may be an additional synergistic interaction between amantadine and topiramate.
The cases reported above demonstrate a novel approach to the treatment of catatonia. Topiramate was successful in four cases that were refractory to the more usually effective therapies. Two of the patients experienced relapses while still taking the drug, which may suggest that topiramate should not be considered an effective drug for maintenance therapy (or may only reflect what the authors knew, that these were refractory cases). The other two patients have experienced sustained remissions of a year or more.
1. Taylor MA, Fink M: Catatonia in psychiatric classification: a home of its own. Am J Psychiatry 2003; 160:233–1241Google Scholar
2. Taylor MA: Clinical examination. In Catatonia: from Psychopathology to Neurobiology. Caroff S (Ed.), Mann S, Francis A, Fricchione G: American Psychiatric Press, 2004. Washington, DC, London EnglandGoogle Scholar
3. Fink M, Taylor MA: Catatonia: A Clinician’s Guide to Diagnosis and Treatment. Cambridge University Press, Cambridge, UK 2003Google Scholar
4. Losonczy MF, Song IS, Mohs RC, et al: Correlates of lateral ventricular size in chronic schizophrenia, I behavioral and treatment response measures. Am J Psychiatry 1986; 143:976Google Scholar
5. Taylor MA, Abrams R: Catatonia: prevalence and importance in the manic phase of manic-depressive illness. Arch Gen Psychiatry 1977; 34:1223–1225Google Scholar
6. Abrams R, Taylor MA, Stolurow KAC: Catatonia and mania: patterns of cerebral dysfunction. Biol Psychiatry 1979; 14:111–117Google Scholar
7. The American Psychiatric Association: Diagnostic and Statistical Manual IV. Washington, DC, American Psychiatric Press, 1999Google Scholar
8. Dhossche D, Bourman NH: Catatonia in children and adolescents. J Am Acad Child Adolesc Psychiatry 1997; 36:870–871Google Scholar
9. Dhossche D: Brief report: catatonia in autistic disorders. J Autism, Dev Discord 1998; 28:329–331Google Scholar
10. Cohen D, Flament M, Cubos P, et al: Case series: catatonic syndrome in young people. J Am Acad Child Adolsec Psychiatry 1999; 38:1040–1046Google Scholar
11. Lund CE, Mortimer AM, Rogers D, et al: Motor, volitional and behavioral disorders in schizophrenia, I: assessment using the modified rogers scale. Br J Psychiatry 1991; 158:323–327Google Scholar
12. Northoff G, Kock A, Wenke J, et al: Catatonia as a psychomotor syndrome: a rating scale and extrapyramidal motor symptoms. Mov Disord 1999; 14:404–416Google Scholar
13. Peralta V, Cuesta MJ: Motor features in psychotic disorders I: factor structure and clinical correlates. Schizophr Res 2001; 47:107–116Google Scholar
14. Peralta V, Cuesta MJ: Motor features in psychotic disorders, II: development of diagnostic criteria for catatonia. Schizophr Res 2001; 47:117–126Google Scholar
15. Rosebush PL, Mazurek M: Pharmacotherapy, in Catatonia from Psychopathology to Neurobiology. Edited by Caroff SN, Mann SC, Francis A, Fircchione GL. Washington, DC, London American Psychiatric Press, 2004Google Scholar
16. Kruger S, Braunig P: Intravenous valproic acid in the treatment of severe catatonia. J Neuropsychiatry Clin Neurosci 2001; 13:303–304Google Scholar
17. Kritzinger PR, Jordaan GP: Catatonia: an open prospective series with carbamazepine. Int J Neuropsychopharmacol 2001; 4:251–257Google Scholar
18. Millson RC: Topiramate for refractory schizophrenia. Am J Psychiatry 2002; 159:675Google Scholar
19. Northoff G: What catatonia can tell us about “top-down modulation”: a neuropsychiatric hypothesis. Behav Brain Sci 2002; 25:555–577Google Scholar
20. Sperk G, Lassmann H, Baran H, et al: Kainic acid induced seizures: neurochemical and histopathological changes. Neuroscience 1983; 10:1301–1315Google Scholar
21. Northoff G, Eckert J Fritze J: Glutamatergic dysfunction in catatonia? successful treatment of three acute akinetic catatonic patients with the nmda antagonist amantadine. J Neurol Neurosurg Psychiatry 1997; 62:404–406Google Scholar
22. Northoff G: Neuroimaging and neurophysiology, in Catatonia from Psychopathology to Neurobiology. Edited by Caroff SN, Mann SC, Francis A, Fricchione GL. Washington, DC, London, American Psychiatric Press, 2004Google Scholar
23. Goff DC, Coyle JT: The emerging role of glutamate in the pathophysiology and treatment of schizophrenia. Am J Psychiatry 2001; 158:1367–1377Google Scholar
24. Laruelle M, Kegeles LS, Abi-Dargham A: Glutamate, dopamine and schizophrenia: from pathophysiology to treatment. Ann NY Acad Sci 2003; 1003:138–158Google Scholar



