Mental Disorders in Mexican Patients With Multiple Sclerosis
Recently, the administration of a multi-symptom inventory, developed for the use of neurologic disorders with neuropsychiatric manifestations, reported depressive symptoms in 79% of a sample of multiple sclerosis patients, anxiety in 37%, irritability in 35%, and disinhibition/euphoria in 13% of these patients. 5 A study measuring categorical psychiatric diagnosis, rather than isolated symptoms, reported point prevalence for depression in 47% of participants and twice the risk of any non-mood psychiatric disorder in multiple sclerosis patients relative to healthy comparison subjects. 6 The lifetime prevalence for major depression in a clinical setting due to multiple sclerosis has varied in different reports from 25%–50%. 7 , 8 In community-based populations the figure of previously unrecognized depression has been reported up to 41.8%, with 23% of the sample experiencing severe symptoms of depression associated with disability and severity of the illness. 9 , 10 The lifetime prevalence of bipolar disorder has been reported in 13%. 11 , 12 Anxiety disorders were estimated in 35.7% of multiple sclerosis patients in a study that focused on the assessment of the lifetime prevalence of this axis I disorder according to DSM-IV-TR criteria. 13
The aim of our study was to explore the presence of psychiatric comorbidity, according to DSM-IV axis I disorders, in a series of multiple sclerosis outpatients. We established correlations of the psychiatric diagnoses with age, sex, number of relapses, duration of illness and neurological disability rated with the Expanded Disability Status Scale. 14
METHODS
The sample included 37 consecutive patients who fulfilled McDonald criteria for the diagnosis of multiple sclerosis after the evaluation by two neurologists. 15 The patients were attending follow-up visits at the demyelinating diseases clinic of the National Institute of Neurology and Neurosurgery of Mexico. The sociodemographic data registered were age, gender, and level of education, as well as clinical variables such as clinical course, current disease altering therapy and neurological disability rated by the Expanded Disability Status Scale. Duration of illness was estimated from the first neurological syndrome suggestive of multiple sclerosis, when such information was obtained from the clinical history. In the cases where no multiple sclerosis attributable neurological clinical syndromes were elicited, duration of illness was estimated from time of diagnosis in the neurological clinic. We excluded patients with other medical or neurological conditions and patients receiving corticosteroid therapy within 6 months prior to the study.
A comparison group of 37 subjects matched by gender, age, and level of education was recruited. It was composed of 20 family members of patients with a neurological or psychiatric disorder (except multiple sclerosis), who join the family groups in the National Institute of Neurology and Neurosurgery (NINN) monthly, and 17 workers at the National Institute of Public Health of Mexico. Participants with a previous neurological or psychiatric diagnosis or treatment were excluded from the study.
A psychiatrist (ME) administered the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), which diagnoses lifetime and current axis I psychiatric disorders, 16 and the Montgomery-Asberg Depression Rating Scale, used to assess the severity of depression among patients in whom a diagnosis of depressive illness has been made, 17 , 18 to patients and comparison subjects. The proposed cutoff points for the Montgomery-Asberg Depression Rating Scale are scores of 0 to 6 (absence of symptoms), 7 to 19 (mild depression), 20 to 34 (moderate depression), and 35 to 60 (severe depression). 19 The psychiatrist also administered the Hamilton Anxiety Rating Scale (HAM-A), which provides an overall measure of anxiety including global anxiety and psychic (cognitive) and somatic symptoms. 20 Total scores for the HAM-A range from 0 to 56; a score of ≥14 indicates clinically significant anxiety, and nonclinical subjects typically score ≤5 points. 21
We used descriptive statistics in terms of central tendency and dispersion measures in the case of numeric variables and proportions in relation to nominal variables. Inferential statistics, as represented by chi-square tests, Mann-Whitney tests, and t tests, were used to analyze patients and comparison subjects. Spearman and Pearson correlation analyses were performed on the sample of multiple sclerosis patients in order to seek for significant relationships between demographic and clinical numerical data and ordinal clinimetric measures.
The study protocol was revised and approved by the Ethics Committee of NINN, and it conforms to the provisions of the Declaration of Helsinki in 1995 (revised in Edinburgh, Scotland, 2000). All participants signed a letter of informed consent before they underwent any assessment related to the study. Anonymity was preserved in all cases.
RESULTS
The mean age was 36.3 years old (SD=11.5) in the multiple sclerosis group and 39.88 years old (SD=11.5) in the comparison group. There were 24 women (64.8%) in the multiple sclerosis patient group and 22 women (59.4%) in the comparison group. None of the above sociodemographic variables were significantly different between groups. Multiple sclerosis patients’ mean duration of illness was 7 years (SD=6.39), and the mean Expanded Disability Status Scale score was 4.5 (SD=1.95). At the time of the psychiatric assessment, eight patients (21.62%) were receiving interferon therapy, 19 patients (51.35%) azathioprine, two patients (5.4%) cyclophosphamide, and eight patients (21.62%) were not receiving any kind of treatment. Twenty-eight patients (75.6%) presented with a relapsing-remitting clinical course of the disease, seven patients (18.9%) had a secondary progressive course, and two patients (5.4%) were diagnosed as having a primary progressive course of multiple sclerosis.
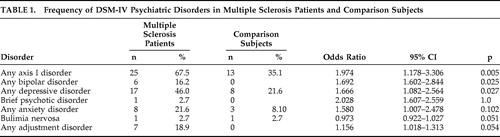
Table 1 shows psychiatric DSM-IV diagnoses obtained administering the SCID-I to patients and controls. Multiple sclerosis patients were more likely to meet the criteria for at least one mental disorder (OR=1.97; 95% CI=1.178–3.306). Six multiple sclerosis patients had diagnosable bipolar disorder (five with bipolar II disorder and one with bipolar I), whereas none of comparison subjects showed such a diagnosis. The greatest burden of morbidity was associated with depressive disorders in general, accounting for 46% of the multiple sclerosis patients and 21.7% of the comparison subjects (OR=1.6, 95% CI=1.082–2.564). Eight multiple sclerosis patients (21.6%) versus two of the comparison subjects (5.9%) had a single episode major depressive disorder. Recurrent major depressive disorder was the most represented depressive disorder in the multiple sclerosis patients, occurring in 12 patients (32.4%) versus three of the comparison subjects (8.8%). Dysthymic disorder was present in one multiple sclerosis patient (2.7%) and in four of the comparison subjects (10.8%). We did not find depression with psychotic or melancholic features. Eight multiple sclerosis patients (28.6%) met the criteria for any anxiety disorder, relative to three of the comparison subjects (8.1%). The most common anxiety disorder in the multiple sclerosis group was generalized anxiety disorder, with one case of obsessive-compulsive disorder. The comparison group presented more varied types of anxiety disorders, with one case of obsessive-compulsive disorder, one case of generalized anxiety disorder, and one case of social phobia. We diagnosed bulimia nervosa one time in each group. There were seven cases (18.9%) of adjustment disorder in the multiple sclerosis group; one patient presented with depressed mood, four with anxiety and depressed mood, and two with disturbance of conduct and emotions. Suicidal intent was explored and denied in both groups.
 |
Levels of depression measured with the Montgomery-Asberg Depression Rating Scale scores were 15.54±9.42 in the multiple sclerosis group and 11.73±7.59 in the comparison group; the difference was not statistically significant, although a trend was observed (p=0.111, t test). The mean severity score of the current depressive disorders in the multiple sclerosis sample was 22.4, corresponding to moderate depression according to the Montgomery-Asberg Depression Rating Scale. Levels of anxiety measured with the HAM-A were significantly higher in patients with multiple sclerosis and depressive disorders than in patients with multiple sclerosis without a depressive disorder (HAM-A=21.2, SD=9.91 versus HAM-A=9.33, SD=8.54, p.001).
In the multiple sclerosis group, we did not find a significant difference concerning correlations between age, number of relapses, duration of illness, Expanded Disability Status Scale scores, and severity measures for anxiety and depression. Also, no significant difference was found regarding depression measures with the Montgomery-Asberg Depression Rating Scale in patients treated with interferon than in the patients not receiving interferon therapy (mean=16.17, SD=5.80, in multiple sclerosis patients receiving interferon versus mean=14.43, SD=8.95, in multiple sclerosis patients not receiving interferon, p=0.773, Mann-Whitney test). Gender and clinical course of multiple sclerosis showed no significant difference between multiple sclerosis patients meeting criteria for DSM-IV psychiatric diagnoses and multiple sclerosis patients not meeting criteria for a mental disorder.
DISCUSSION
The main objective of this study was to explore the prevalence of psychiatric disorders in a sample of multiple sclerosis patients and to analyze the results relative to a healthy comparison group. The study confirms a higher prevalence of any axis I disorder in the multiple sclerosis group relative to the comparison group (67.5% versus 35.1%).
The most common disorders were the ones grouped as any depressive disorder, mostly composed of single episode or recurrent major depressive disorder, whereas dysthymic disorders predominated in the comparison group. The population with multiple sclerosis and a diagnosis of a depressive disorder showed significantly higher scores of anxiety symptoms measured by the HAM-A relative to multiple sclerosis patients and cases from the comparison group experiencing other types of DSM-IV diagnoses. This suggests that the type of depression presenting in multiple sclerosis is frequently accompanied by anxiety and vegetative symptoms. From a diagnosis and detection perspective, a relevant fact is that other studies exploring the longitudinal course of depression in multiple sclerosis have found that mood symptoms of depression are significantly more variable over time than neurovegetative symptoms. 22 From a therapeutic and prognostic perspective, the comorbidity of depression and anxiety has been associated with increased thoughts of self-harm, more somatic complaints, and greater social dysfunction. 23
Depression is highly prevalent in multiple sclerosis, and the core symptoms of depression reduce cognitive capacity and exacerbate disability. 24 , 25 Moreover, it is known that depression in multiple sclerosis is unrecognized and untreated, 26 and it is strongly associated with suicidal intent, a common finding in other studies. 27
Lifetime prevalence of any anxiety disorders in multiple sclerosis patients was 21.6% with a mean severity score of 27.71. In previous studies anxiety and depression have been reported as intermediate factors in the association with disability measures and quality of life. 28 However, in our study no correlations between anxiety disorders and Expanded Disability Status Scale scores were found.
Depressive disorders in our comparison patients were higher relative to the national figures obtained from the Mexican National Comorbidity Survey. 29 This survey assessed psychiatric disorders of the general population using a nationally representative sample. The high prevalence of depression in our sample is probably explained by a higher risk of psychiatric symptoms in caregivers, who comprised more than half of our comparison group. Overall, six participants (75%) with any depressive disorder and all four cases meeting criteria for dysthymic disorder of this group were family members of patients. Depression could be a result of the psychological adjustment and overburden of being a caregiver, 30 and the health system should attend to the psychological wellbeing of this population. Hence, a limitation of our study is that our comparison group cannot be regarded as entirely composed of “healthy” individuals. In spite of this, the multiple sclerosis group had a two-fold frequency of depression, confirming a positive association between multiple sclerosis and depression in Mexican patients.
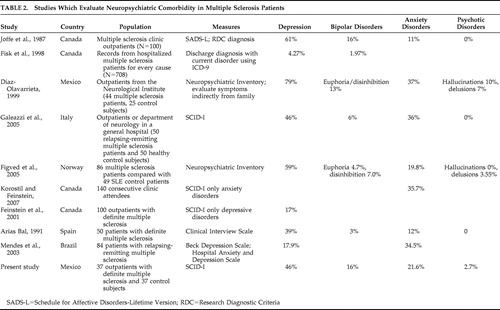
In Table 2 , we summarize the results of previous neuropsychiatric studies of multiple sclerosis. As shown, there are significant variations in the frequency of mental disorders, probably related to the assessment methodology (dimensional versus categorical measures; direct versus indirect approaches). Also shown in Table 2 , only a few studies have been done in Latin American or Hispanic populations. Taking into account the fact that there are regional changes in multiple sclerosis prevalence around the world, there is a significant concern regarding the variability of neuropsychiatric features of multiple sclerosis. It is not known if neuropsychiatric manifestations of multiple sclerosis are universal or influenced by race and culture; regional neuropsychiatric epidemiology is necessary to clarify this issue. In Hispanic or Latin-American patients, only one study in a Spanish population has been reported with use of categorical diagnosis and direct assessment. 31 A recent Brazilian study evaluated depression and anxiety in multiple sclerosis with dimensional measures. 32 A previous Mexican study 5 used indirect assessment and reported higher prevalence of depression, anxiety, and psychotic features, as compared to our findings and other international studies using different assessment methods. This fact points out the possibility of overestimation of mental disorders when using indirect measures. Notwithstanding the fact that multiple sclerosis patients frequently present with cognitive impairment, most of these patients have the capacity to express their own psychopathology, mainly related to anxiety and depression. The SCID-I, our mental disorders assessment method, provides both direct and indirect assessments 16 and hence could offer a more accurate measure of mental disorders. This is supported by the fact that frequencies reported by our study are within the range of international literature, and support homogeneity of mental disorders in this disease across borders, probably related to universal effects of multiple sclerosis in the psychological and neuropathological dimensions.
 |
1. Murray TJ: The history of multiple sclerosis, in Multiple Sclerosis: Diagnosis, Medical Management, and Rehabilitation. Edited by Burke JS, Johnson KP. New York, Demos Medical Publishing, 2000, pp 1–32Google Scholar
2. Feinstein A: The neuropsychiatry of multiple sclerosis. Can J Psychiatry 2004; 49:157–163Google Scholar
3. Zorzon M, de Masi R, Nasuelli D, et al: Depression and anxiety in multiple sclerosis: a clinical and MRI study in 95 subjects. J Neurol 2001; 248:416–421Google Scholar
4. Lopez-Meza E, Corona-Vazquez T, Ruano-Calderon LA, et al: Severe impulsiveness as the primary manifestation of multiple sclerosis in a young female. Psychiatry Clin Neurosci 2005; 59:739–742Google Scholar
5. Diaz-Olavarrieta C, Cummings J, Velazquez J, et al: Neuropsychiatric manifestations of multiple sclerosis. J Neuropsychiatry Clin Neurosci 1999; 11:51–57Google Scholar
6. Galeazzi GM, Ferrari S, Giaroli G, et al: Psychiatric disorders and depression in multiple sclerosis outpatients: impact of disability and interferon beta therapy. Neurol Sci 2005; 26:255–262Google Scholar
7. Minden SL, Schiffer RB: Affective disorders in multiple sclerosis: review and recommendations for clinical research. Arch Neurol 1990; 47:98–104Google Scholar
8. Schiffer RB, Caine ED, Bramford KA, et al: Depressive episodes in patients with multiple sclerosis. Am J Psychiatry 1983; 140:1498–1500Google Scholar
9. McGuigan C, Hutchinson M: Unrecognized symptoms of depression in a community-based population with multiple sclerosis. J Neurol 2006; 253:219–223Google Scholar
10. Chwastik L, Dawn EM, Gibbons LE, et al: Depressive symptoms and severity of illness in multiple sclerosis: epidemiologic study of a large community sample. Am J Psychiatry 2002; 159:1862–1868Google Scholar
11. Joffe RT, Lippert GP, Gray TA, et al: Mood disorder and multiple sclerosis. Arch Neurol 1987; 44:376–378Google Scholar
12. Young CR, Weiss FL, Bowers MB, et al: The differential diagnosis of multiple sclerosis and bipolar disorder. J Clin Psych 1997; 58:123Google Scholar
13. Korostil M, Feinstein A: Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler 2007; 13:67–72Google Scholar
14. Kurtzke JF: Rating neurological impairment in multiple sclerosis: an expanded disability status scale. Neurology 1983; 33:1444–1452Google Scholar
15. Polman CH, Reingold SC, Edan G, et al: Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald criteria.” Ann Neurol 2005; 58:840–846Google Scholar
16. First MB, Spitzer R, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version (SCID-CV), Spanish Version. Washington, DC, American Psychiatric Press, 1999Google Scholar
17. Montgomery SA, Asberg M: A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134:382–389Google Scholar
18. Lobo A, Chamorro L, Luque A, et al: Validation of the Spanish versions of the Montgomery-Asberg Depression and Hamilton Anxiety Rating Scales. Med Clin 2002; 118:493–499Google Scholar
19. Snaith RP, Harrop FM, Newby DA, et al: Grade scores of the Montgomery-Asberg Depression and the Clinical Anxiety Scales. Br J Psychiatry 1986; 148:599–601Google Scholar
20. Hamilton M: The assessment of anxiety states by rating. Br J Med Psychol 1959; 32:50–55Google Scholar
21. Kobak KA, Reynolds WM, Greist JH: Development and validation of a computer administered version of the Hamilton anxiety scale. Psychol Assessment 1993; 5:487–492Google Scholar
22. Arnett PA, Randolph JJ: Longitudinal course of depression symptoms in multiple sclerosis. J Neurol Neurosurg Psychiatry 2006; 77:606–610Google Scholar
23. Feinstein A: Depression: prevalence, symptoms, diagnosis, and clinical correlates, in The Clinical Neuropsychiatry of Multiple Sclerosis, 2nd ed. New York, Cambridge University Press, 2007, pp 28–46Google Scholar
24. Feinstein A: Mood disorders in multiple sclerosis and the effects on cognition. J Neurol Sci 2006; 245:63–66Google Scholar
25. Arnett PA: Longitudinal consistency of the relationship between depression symptoms and cognitive functioning in multiple sclerosis. CNS Spectr 2005; 10:372–382Google Scholar
26. Mohr DC, Hart SL, Fonareva I, et al: Treatment of depression for patients with multiple sclerosis in neurology clinics. Mult Scler 2006; 12:204–208Google Scholar
27. Feinstein A: An examination of suicidal intent in patients with multiple sclerosis. Neurology 2002; 59:674–678Google Scholar
28. Janssens AC, van Doorn PA, de Boer JB, et al: Anxiety and depression influence the relation between disability status and quality of life in multiple sclerosis. Mult Scler 2003; 9:397–403Google Scholar
29. Medina-Mora MA, Borges G, Benjet C, et al: Psychiatric disorders in Mexico: lifetime prevalence in a nationally representative sample. Br J Psychiatry 2007; 190:521–528Google Scholar
30. Sculz R, Sherwood PR: Physical and mental health effects of family caregiving. Am J Nurs 2008; 108:23–28Google Scholar
31. Arias Bal MA, Vázquez-Barquero JL, Peña C, et al: Psychiatric aspects of multiple sclerosis. Acta Psychiatr Scand 1991; 83:292–296Google Scholar
32. Mendes MA, Tilbery CP, Balsimelli S, et al: Depressao na esclerose multipla forma remitente-recorrente. Arq Neuropsiquiatr 2003; 61:591–595Google Scholar
33. Fisk JD, Morehouse S, Brown M, et al: Hospital-based psychiatric service utilization and morbidity in multiple sclerosis. Can J Neurol Sci 1998; 25:230–235Google Scholar
34. Figved N, Klevan FN, Myhr KM, et al: Neuropsychiatric symptoms in patients with multiple sclerosis. Acta Psychiatr Scand 2005; 112:463–468Google Scholar
35. Feinstein A, Feinstein K: Depression associated with multiple sclerosis: looking beyond diagnosis to symptom expression. J Affect Disord 2001; 66:193–198Google Scholar



