Impaired Set-Shifting Ability and Therapeutic Response in Obsessive-Compulsive Disorder
Abstract
Set-shifting ability and therapeutic response to serotonin reuptake inhibitors were investigated in 20 patients with obsessive-compulsive disorder. A clear relationship was found between impaired performance on two Wisconsin Card Sorting subtests (categories completed and perseverative errors) and positive treatment response.
In several studies, patients with obsessive-compulsive disorder (OCD) exhibited impaired set-shifting ability (SSA), as elicited by tests of executive functions such as the Wisconsin Card Sorting Test1–3 and the Attentional Set-shifting Task.4 It was suggested that this impairment may underlie the difficulties that patients with OCD have in deflecting from an established course of thought or action.1
In patients with OCD, impaired SSA was found to correlate positively with the severity of obsessive-compulsive symptoms,1 with the presence of psychotic phenomena,2 and with reduced left inferior frontal and caudate nucleus cerebral blood flow.3 Additionally, the performance of patients with OCD on a set-shifting task correlated negatively with the prolactin response to meta-chlorophenylpiperazine (m-CPP),5 suggesting that patients with OCD and impaired SSA may also show altered serotonergic tonus.
The objectives of our study were twofold: 1) to evaluate the performance of patients with OCD on set-shifting tasks; and 2) to correlate this performance with the severity of obsessive-compulsive symptoms and therapeutic response to a serotonin reuptake inhibitor (SRI).
METHODS
Patients were recruited through advertisements in newspapers and referrals from clinicians. The Structured Clinical Interview for DSM-IV (SCID-I)6 was employed for diagnostic assessment. Twenty patients were selected according to the following inclusion criteria: having OCD as the most clinically significant diagnosis; a score of 4 or greater on the Clinical Global Impression (CGI);7 and a drug-free status for the last 2 weeks prior to testing (5 weeks in the case of fluoxetine). The exclusion criteria were central nervous system diseases, systemic diseases, psychosis, severe personality disorders, alcohol or drug abuse, and low levels of intelligence (as shown by performance below the 16th percentile on the Vocabulary subtest of the Wechsler Adult Intelligence Scale–Revised8). The study was approved by the local ethics committee. Informed consent was obtained from the patients at baseline, after the objectives and procedures of the study were fully explained.
The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS)9 and the Clinical Global Impression were employed to measure the severity of symptoms. The following tests were used to assess executive functions: Wisconsin Card Sorting Test (WCST);10 Trail Making Test, parts A and B (TMT A and B);11 and Controlled Oral Word Association Test (COWAT).12 SSA was specifically assessed with the WCST and the TMT B/A time ratio.
In the WCST subtests, patients were considered impaired if their performance was below the 16th percentile, according to normative data corrected for age and education.10 In the case of TMT, patients were considered impaired when their performance, according to normative data corrected by age, was below the 10th percentile on part A or below the 20th percentile on part B.11 The time ratio TMT B/A was considered abnormal when it was greater than 3. On the COWAT, the cutoff points were 9 for patients with less than 8 years of education and 13 for patients with additional schooling.12
After psychiatric and neuropsychological evaluation, patients were openly treated with an SRI for 10 weeks. Selections of specific medications were based on the clinical judgment of the attending psychiatrist (L.F.). Doses were adjusted according to therapeutic response and tolerability. Patients were defined as treatment responders if there was a reduction of at least 35% in the initial total scores on Y-BOCS and/or a CGI of 1 (much better) or 2 (better) at the end of treatment.
Chi-square or two-tailed Fisher's exact tests were employed to compare response status (responder vs. nonresponder) and test performance (impaired vs. nonimpaired). The Mann-Whitney U-test was employed to compare severity of symptoms and test performance. The adopted level of significance was 5%. Means are reported with standard deviations.
RESULTS
The mean age of the sample was 39.15±14.09 years. Ten patients (50%) were males. In week 0, the mean Y-BOCS obsessions subscore was 8.20±6.39 (range 0–20); compulsions subscore, 13.55±4.27 (range 0–20); and total Y-BOCS score, 21.75±7.72 (range 9–38). The mean CGI was 5.20±0.89 (range 4–6).
Nineteen patients (95%) had impaired performance on at least one executive test, and 15 patients (75%) did poorly on two or more tests. Sixteen (80%) had impairment on at least one subtest of WCST: 12 (60%) on trials to complete the first category; 8 (40%) on number of categories completed; 5 (25%) on failure to maintain set; 5 (25%) on learning to learn; 5 (25%) on perseverative errors; and 6 (30%) on nonperseverative errors. Eighteen (90%) performed poorly on the Trail Making Test: 14 (70%) on Part A and 16 (80%) on Part B. Eight (40%) had abnormal TMT B/A time ratios. Five patients (25%) were impaired in performance of the COWAT.
Only one relationship between impaired performance on an executive test and the severity of symptoms emerged: patients with impaired verbal fluency, as elicited by the COWAT, had significantly greater mean obsessions subscores (15.00±4.00) than patients without this impairment (6.80±5.88; Z=–2.47, df=18, P=0.01).
Seventeen patients completed 10 weeks of treatment with an SRI: 8 were treated with clomipramine (mean daily dose=116.88 mg); 4 with sertraline (mean daily dose=187.50 mg); 3 with paroxetine (mean daily dose=60 mg), 1 with fluoxetine (40 mg/day) and 1 with fluvoxamine (350 mg/day). There were three dropouts, 1 because of unwanted effects and 2 for unknown reasons (lost to follow-up). Among the patients who completed 10 weeks of treatment, 52.9% were considered treatment responders.
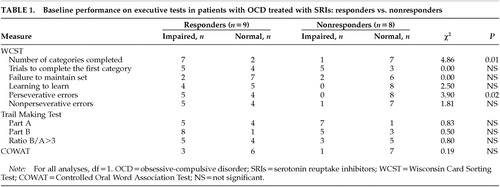
A relationship was found between positive treatment response to an SSRI and impaired performance on two subtests of WCST (Table 1): number of categories completed (χ2=4.8607, df=1, P=0.01) and perseverative errors (χ2=3.9046, df=1, P=0.02).
DISCUSSION
Our findings are consistent with previous reports describing a dysexecutive syndrome affecting patients with OCD.1–4 Specifically, there was evidence of significant impairment in SSA in a large proportion of our sample. Eighty percent of our patients had a poor performance on at least one subtest of the WCST, and among these, 8 also had a TMT B/A time ratio greater than 3.
Patients with impaired verbal fluency had significantly more severe obsessions than the other patients. To our knowledge, this association has not been described before. Our hypothesis is that the intrusion of obsessive thoughts during the testing might have interfered with the ability of some of our patients with OCD to generate words.
After patients were pharmacologically treated with an SRI, a clear relationship was found between positive treatment response and impaired SSA (as shown by poor performance on two subtests of the WCST, number of categories completed and perseverative errors). Even though we are not aware of any previous report describing this association, Hollander and Wong5 had already suggested that patients with OCD and impaired SSA have altered serotonergic tonus. Considering that the WCST is hypothesized to be a dorsolateral prefrontal task,13 this finding suggests that a subgroup of patients with OCD and a dysfunction in this area may show a more favorable therapeutic response to a short-term treatment with an SRI.
Our preliminary study has some significant limitations. First, the sample was relatively small. Second, it did not include a control group. Third, patients were treated in an open fashion, with several different SRIs and dosage schemes. There is a growing body of evidence showing that these drugs may have idiosyncratic actions at receptors other than the serotonin transporter and on various enzymes that may impart them different therapeutic characteristics.14 Nevertheless, our main finding, that impaired SSA in patients with OCD may be a predictor of positive therapeutic response to treatment with an SRI, may have significant clinical implications and needs to be further investigated in larger studies using more standardized therapeutic procedures.
ACKNOWLEDGMENTS
The authors thank Dr. Mauro Vítor Mendlowicz and Dr. Euripedes Constantino Miguel for their careful review of the manuscript. This work was supported by the Coordination for the Improvement of Higher Education Personnel Foundation (CAPES) and the National Council for Scientific and Technological Development (CNPq/Brazil).
 |
1 Harvey NS: Impaired cognitive set-shifting in obsessive-compulsive disorder. IRCS Medical Science 1986; 14:936-937Google Scholar
2 Malloy P: Frontal lobe dysfunction in obsessive-compulsive disorder, in The Frontal Lobes Revisited, edited by Perecman E. Hillsdale, NJ, Lawrence Erlbaum, 1987, pp 207-223Google Scholar
3 Lucey JV, Burness CE, Costa DC, et al: Wisconsin Card Sorting Task (WCST) errors and cerebral blood flow in obsessive-compulsive disorder (OCD). Br J Med Psychol 1997; 70:403-411Crossref, Medline, Google Scholar
4 Purcell R, Maruff P, Kyrios M, Pantelis C: Cognitive deficits in obsessive-compulsive disorder on tests of frontal-striatal function. Biol Psychiatry 1998; 43:348-357Crossref, Medline, Google Scholar
5 Hollander E, Wong CM: The relationship between executive function impairment and serotonergic sensitivity in obsessive-compulsive disorder. Neuropsychiatry Neuropsychol Behav Neurol 1996; 9:230-233Google Scholar
6 First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis I Disorders: Patient Edition (SCID- I/P, Version 2.0). New York, Biometrics Research Department, New York State Psychiatric Institute, 1996Google Scholar
7 Guy W: ECDEU Assessment manual for psychopharmacology (Publ No ADM 76-338). Rockville, MD, US Department of Health, Education, and Welfare, 1976, pp 217-222Google Scholar
8 Wechsler D: Wechsler Adult Intelligence Scale-Revised. New York, Psychological Corporation, 1981Google Scholar
9 Goodman WK, Price LH, Rasmussen SA, et al: The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry 1989; 46:1006-1011Crossref, Medline, Google Scholar
10 Heaton RK, Chelune GL, Talley J: Wisconsin Card Sorting Test (WCST) Manual Revised and Expanded. Odessa, FL, Psychological Assessment Resources, 1993Google Scholar
11 Spreen O, Strauss E (eds): A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. New York, Oxford University Press, 1998Google Scholar
12 Brucki SM, Malheiros SM, Okamoto IH, et al: Normative data on the verbal fluency test in the animal category in our milieu. Arq Neuropsiquiatr 1997; 55:56-61Crossref, Medline, Google Scholar
13 Van Horn JD, Berman KF, Weinberger DR: Functional lateralization of the prefrontal cortex during traditional frontal lobe tasks. Biol Psychiatry 1996; 39:389-399Crossref, Medline, Google Scholar
14 Stahl SM: Not so selective serotonin reuptake inhibitors. J Clin Psychiatry 1998; 59:343-344Medline, Google Scholar