Comparability of the Clinical Diagnostic Criteria for Vascular Dementia: A Critical Review. Part I
There is now an increasing effort in clinical neurosciences to detect prodromal symptoms of various dementia illnesses, 8 including that of vascular dementia. 9 , 10 Early diagnosis is certainly of great importance because nootropic drugs are now available for treatment of mild to moderate dementia. 11 Two well-recognized clinical criteria sets for the diagnosis of Alzheimer’s disease—the National Institute of Neurological and Communicative Diseases and Stroke/Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) 12 and the criteria of the Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition—are currently used and reach sensitivity rates of nearly 90%. 13 – 15 This relative diagnostic success with Alzheimer’s disease has allowed the development of criteria for the diagnosis of mild cognitive impairment of the amnestic type, which is believed to be a prodromal phase of Alzheimer’s disease. 8 , 16 On the other hand, at least eight different clinical diagnostic criteria sets for vascular dementia or multi-infarct dementia have been used in clinical and research settings: the original Hachinski Ischemic Scale 17 and its modified version, the Ischemic Scale of Rosen; 18 the criteria proposed by the DSM-III, DSM-III-R, and DSM-IV; the International Classification of Diseases, 10th Revision (ICD-10); the State of California Alzheimer’s Disease Diagnostic and Treatment Centers (ADDTC); 19 and by the National Institute of Neurological Disorders and Stroke-Association Internationale pour la Recherche et l’Enseignement en Neurosciences (NINDS-AIREN). 20 Before developing criteria for the preclinical phase of vascular dementia, the validity of the current clinical diagnostic criteria for vascular dementia should be assessed and ascertained. Therefore the current qualitative review aims at describing and comparing the above-mentioned criteria according to their respective definition of the cognitive syndrome and their description of the vascular causes necessary for the diagnosis of vascular dementia. The ultimate goal is thus to present critical issues related to the diagnosis of vascular dementia. The present article is the first part of a systematic review containing two parts. Part 2 21 examines the differential sensitivity and specificity rates of the eight diagnostic criteria and makes suggestions to improve the current criteria for vascular dementia.
Description of the Different Clinical Criteria and Their Deficit Requirements
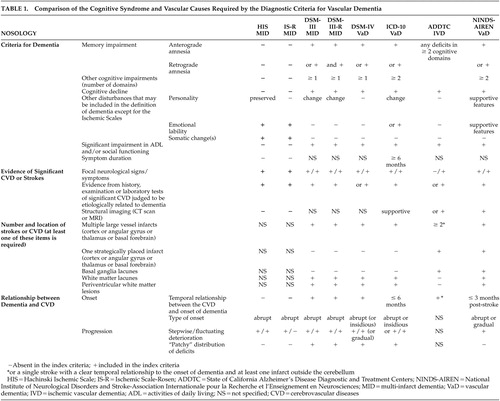
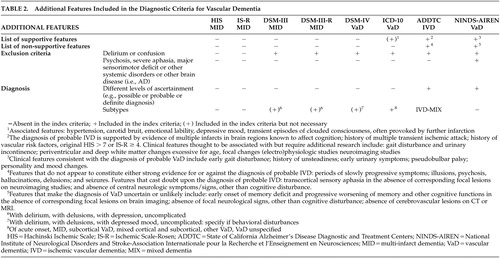
The different clinical criteria used to diagnose vascular dementia or multi-infarct dementia are detailed and compared in Table 1 and Table 2 . Table 1 presents the cognitive syndrome, vascular causes and their relationships for each set of criteria for vascular dementia, whereas Table 2 presents the additional features mentioned in these criteria.
 |
 |
The Ischemic Scales
The Hachinski Ischemic Scale 17 and the Ischemic Scale of Rosen (IS-R) 18 assign a 1 or 2 point value to each medical feature, and the final summation of these points results in an Ischemic Score. In patients with dementia, a Hachinski Ischemic Scale score ≤4 (IS-R ≤2) suggests a diagnosis of Alzheimer’s disease, whereas a Hachinski Ischemic Scale score ≥7 (IS-R=4–10) suggests a diagnosis of multi-infarct dementia. An intermediate Hachinski Ischemic Scale score of 5–6 suggests a diagnosis of mixed dementia. However, these scales do not include any definition of the cognitive syndrome associated with the diagnosis of multi-infarct dementia. They also do not mention any specific location for the vascular lesions required in order to meet the criteria of multi-infarct dementia.
The DSM Criteria
The different sets of DSM criteria—DSM-III, DSM-III-R, and DSM-IV—require memory impairment and other cognitive deficits in various cognitive domains to reach a diagnosis of vascular dementia. These deficits must be “sufficiently severe to cause impairment in occupational or social functioning” and represent a “decline from a previous higher level of functioning.” The principal difference between the various DSM sets of criteria concerns the requirements for memory impairment. The DSM-III and DSM-IV criteria require alterations either in anterograde or retrograde memory, whereas the DSM-III-R criteria require impairments in both systems of memory. Another difference between these three sets of criteria concerns their requirement for vascular disease. The DSM-III and DSM-III-R require focal neurological signs/symptoms and evidence from history or physical examination of significant cerebrovascular diseases judged to be etiologically related to the disturbances. The DSM-IV requires either focal neurological signs/symptoms or significant cerebrovascular diseases, such as multiple infarcts in the cortex and subcortical white matter, that are judged to be etiologically related to the disturbances. Moreover, the DSM-III and DSM-III-R criteria require an abrupt onset and a stepwise deteriorating course with “patchy” distribution of cognitive deficits, although according to the DSM-IV, the onset can also be insidious and followed by a gradual decline. However, none of the DSM criteria mention the mandatory vascular brain lesions or an underlying vascular explanatory mechanism, clearly characterizing vascular dementia.
The ICD-10
The ICD-10 criteria define dementia as a progressive and unequal impairment of multiple higher cortical functions including memory impairment, deteriorations in general processing of information, and judgment and thinking (such as planning or organizing), but with preserved awareness. Deterioration from a previously higher level of performance should be established for a confident clinical diagnosis, and memory impairment should clearly be present for at least 6 months. Noncognitive features, such as deterioration in emotional control, social behavior, and motivation, may also accompany dementia. The ICD-10 criteria for vascular dementia require the presence of focal neurological signs and symptoms and evidence from history, examination, or tests of significant cerebrovascular diseases, which may reasonably be judged to be etiologically related to the dementia. The onset of dementia can either be abrupt, with a stepwise deterioration, or more gradual, and there must be an unequal distribution of cognitive deficits. These criteria also mention the existence of six subtypes of vascular dementia: acute onset, multi-infarct, subcortical, mixed cortical and subcortical, other, and unspecified dementias. Confirmation of the vascular etiology can be provided by CT, positron emission tomography (PET), MRI, or ultimately by neuropathological examination. Therefore, like the DSM criteria, the ICD-10 criteria have not detailed the mandatory vascular lesions that should be found using the brain imaging techniques.
The ADDTC Criteria
The State of California Alzheimer’s Disease Diagnostic and Treatment Centers (ADDTC) criteria were initially designed specifically to diagnose ischemic vascular dementia. 19 These criteria do not prioritize memory deficits over impairments of other cognitive functions. Instead, the authors of these criteria define dementia as “a deterioration from a known or estimated prior level of intellectual function sufficient to interfere broadly with the patient’s customary affairs of life, which is not isolated to a single narrow category of intellectual performance, and which is independent of level of consciousness.” 19 Furthermore, for a diagnosis of probable vascular dementia, the ADDTC criteria require evidence of two or more ischemic strokes (at least one infarct outside the cerebellum) by history, neurological signs, and/or neuroimaging studies (CT or T1-weighted MRI). In the case of a single stroke, a temporal relationship between the stroke and onset of dementia should be clearly documented, though the time interval between the two events is not specified. A diagnosis of possible vascular dementia is made when there is no clear temporal relationship between the single stroke and the onset of dementia or in individuals with clinical and neuroimaging evidence for Binswanger’s disease. To meet the ADDTC criteria for definite vascular dementia, a histopathologic examination of the brain is required with pathological confirmation of multiple infarcts, with at least one infarct being outside the cerebellum. The criteria provide lists of features supporting the diagnosis of vascular dementia as well as features casting doubt on a diagnosis of probable ischemic vascular dementia ( Table 2 ). Finally, the ADDTC criteria allow for a diagnosis of mixed dementia, applied when one or more systemic or brain disorder (thought to be causally related to the dementia) is present. The diagnosis of mixed dementia may thus include ischemic vascular dementia with Alzheimer’s disease.
The NINDS-AIREN Criteria
The National Institute of Neurological Disorders and Stroke-Association Internationale pour la Recherche et l’Enseignement en Neurosciences (NINDS-AIREN) research criteria define dementia as a “cognitive decline from a previously higher level of functioning and manifested by impairment of memory and of two or more cognitive domains. The deficits should be severe enough to interfere with activities of daily living, and should not be due to physical effects of stroke alone.” 20 Cerebrovascular disease is defined by the presence of focal neurological signs and evidence of relevant cerebrovascular diseases revealed by brain imaging. A relationship between dementia and cerebrovascular diseases is inferred by the onset of dementia within 3 months following a recognized stroke, or by an abrupt deterioration in cognitive functions, or a fluctuating, stepwise progression of cognitive deficits. No rationale has been provided to justify the choice of a 3-month interval between cerebrovascular diseases and the onset of dementia. The criteria also include lists of features consistent with the diagnosis, as well as features making the diagnosis uncertain or unlikely ( Table 2 ). In addition, different levels of certainty for the diagnosis are defined. To meet the NINDS-AIREN criteria for probable vascular dementia, there must be a clear temporal relationship between the onset of dementia and cerebrovascular diseases and confirmation of cerebrovascular diseases by cerebral imaging. The NINDS-AIREN criteria for possible vascular dementia include cases with no brain imaging data, or no clear temporal relationship between dementia and cerebrovascular diseases, or with an atypical course of dementia. Histopathological evidence of cerebrovascular diseases must be obtained at autopsy in the absence of any other neuropathological markers such as neurofibrillary tangles, neuritic plaques, or Lewy bodies to meet the NINDS-AIREN criteria for definite vascular dementia. The NINDS-AIREN criteria provide a list of potential locations for the vascular lesions in order to meet the criteria of vascular dementia ( Table 1 ). Finally, the NINDS-AIREN criteria suggest that the term Alzheimer’s disease with cerebrovascular diseases should be reserved to classify patients fulfilling the clinical criteria for possible Alzheimer’s disease who also present clinical brain imaging evidence of relevant cerebrovascular diseases. According to the authors of these criteria, the term “mixed dementia” should be avoided.
Critical Issues
Defining the Cognitive Syndrome or Dementia
The traditional Hachinski Ischemic Scale and its modified version, the Ischemic Scale of Rosen, did not include any definition of the cognitive syndrome. The DSM-III and DSM-IV criteria required anterograde or retrograde memory impairment, and the DSM-III-R criteria required both types of memory impairments in addition to one or more additional cognitive deficits (e.g., aphasia or apraxia) that collectively caused significant impairment in social/occupational functioning. The ICD-10 criteria required an unequal distribution of deficits in higher cognitive functions such as anterograde or retrograde memory and other cognitive deficits that interfered with activities of daily living and should have been present for at least 6 months. The NINDS-AIREN criteria included memory impairment (either in anterograde or retrograde memory) as well as deficits in two other cognitive domains, severe enough to interfere with activities of daily living. The ADDTC criteria did not specify the number or domains of cognitive function to be impaired, but instead proposed a significant progressive deterioration of multiple higher cortical functions.
Clearly, memory impairment is central in the definition of the cognitive syndrome of vascular dementia per the DSM and NINDS-AIREN criteria, just as it is for the diagnosis of Alzheimer’s disease per the DSM and NINCDS-ADRDA criteria. 12 The definition of the cognitive syndrome per the ADDTC criteria, because they are less stringent than the other criteria and do not specify any type of cognitive impairment, might perhaps best capture cognitive impairments caused by vascular risk factors, 6 , 22 , 23 vascular lesions, 24 first-ever stroke, 25 , 26 or vascular dementia. 27 – 29
Indeed, several studies have shown that vascular risk factors are related to cognitive impairment or decline with aging, especially in regards to psychomotor speed, executive function, and episodic and working memory. 30 – 33 Other studies reported that patients with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, 27 typical vascular dementia, 28 or poststroke dementia 34 presented with prominent executive dysfunction. Regarding the possible prodromal phase of vascular dementia, a recent study showed that patients with mild cognitive impairment-multiple domain tend to evolve to vascular dementia over 3 years in comparison with patients presenting with mild cognitive impairment of the amnestic type. 35
In their review, McPherson and Cummings 36 observed that most studies focusing on the cognitive deficits in vascular dementia had combined all patients with cerebrovascular pathology into a single group and suggested that observed “patchy” deficits may be an artifact of studying patients with various neuropathologic changes. Vascular dementia may thus result from a summation of pathologic processes. Moreover, a patchy and unequal neuropsychological profile is not specific to vascular dementia. Several neurodegenerative processes, such as dementia with Lewy bodies, 37 – 41 semantic dementia, primary progressive aphasia, and frontotemporal dementia, 42 differentially impact cerebral regions at a given level of disease severity. Finally, other reviews of vascular dementia concluded that executive dysfunction was more frequently found than memory and language deficits. 43 , 44 However, these findings must be interpreted with caution due to possible inaccuracies in the determination of the dementia subtype and the loss of precision that might result from pooling heterogeneous subgroups of patients with vascular dementia; difficulties identifying a cognitive profile in patients who are required to present with memory impairment and other deficits to meet criteria for dementia; and the use of limited test batteries whose psychometric properties are incompletely understood. 44
Finally, all criteria proposed delirium or confusion as exclusion criteria. Only the NINDS-AIREN, however, proposed stringent exclusion criteria such as clouding of consciousness, delirium, psychosis, severe aphasia, sensorimotor impairment precluding neuropsychological testing—which may result in the false exclusion of many cases of vascular dementia following stroke—and systemic disorders or other brain disease such as Alzheimer’s disease that in and of themselves could account for deficits in memory and cognition ( Table 2 ). When systemic disorders or other brain diseases such as Alzheimer’s disease could have accounted for deficits in memory and cognition, only the ADDTC criteria provided the alternative of a mixed dementia diagnosis; the NINDS-AIREN criteria used the term “Alzheimer disease with CVD” instead.
Therefore, the lack of a clearly defined, evidence-based and consistently applied definition of the “cognitive syndrome” associated with vascular dementia, or more precise subtypes of vascular dementia, is likely to lead to a heterogeneous cohort of patients depending on which criteria are utilized.
Defining the Vascular Cause
The most prevalent types of cerebrovascular diseases include large-vessel disease leading to multi-infarct dementia or strategic cortico-subcortical stroke, small-vessel disease leading to lacunar strokes and Binswanger’s disease, cardiac embolic events, and hemodynamic mechanisms. 45 , 46 However, the vascular lesions required to diagnose cerebrovascular diseases are not included in the clinical criteria for vascular dementia per the Hachinski and Rosen ischemic scales, the DSM-III, DSM-III-R, DSM-IV, and the ICD-10 criteria. The ADDTC criteria require at least two ischemic strokes outside the cerebellum or one infarct with a clear temporal relationship to the onset of dementia as measured by CT or T1-weighted MRI, whereas periventricular and deep white matter lesions were said to be potentially associated with ischemic vascular dementia. The NINDS-AIREN criteria required multiple infarcts (more than one cortical or subcortical lacunar infarcts) or extensive white matter lesions (detected by CT or T1-weighted MRI), but also accept strategically placed single infarcts as evidence of “relevant CVD.” Notably, none of the eight clinical criteria mention the underlying mechanism of these vascular lesions (i.e., hemorrhagic versus occlusive) nor the location or extent of required lesions. In conclusion, there is a need for clarity and consistency with regard to the nature of the vascular lesions which are required to be present for a diagnosis of vascular dementia and its subtypes. It is probable that different types of lesions are associated with different forms of vascular dementia and thus associated with different cognitive profiles and/or courses of illness. This issue will require consideration in future research.
Onset and Evolution of Vascular Dementia
All the criteria, except for the ADDTC, require an abrupt onset with stepwise deterioration. The ICD-10 and NINDS-AIREN also specify a time interval between the cerebrovascular diseases and the onset of dementia (6 and 3 months, respectively). The DSM-IV, ICD-10, and NINDS-AIREN criteria mention that onset may be insidious or gradual. By contrast, the ADDTC do not specify the nature of onset and the pattern of deteriorating course, as patients with ischemic vascular dementia might experience a wide variety of natural histories. However, there is difficulty in establishing a temporal relationship between dementia and cerebrovascular diseases in terms of type of onset and evolution, which makes it difficult to properly identify patients with vascular dementia. Several data clearly suggest that some types of vascular dementia could start and develop in an insidious fashion without any clinically apparent stroke. 47 In particular, several patients with pathologically confirmed pure vascular dementia and most of those with both vascular dementia and Alzheimer’s disease did not have clinical strokes that were temporally related to the onset of their dementia. 47 Moreover, prospective imaging studies demonstrated the occurrence of clinically silent infarctions. 48 Clinically silent cerebrovascular diseases, in the form of cerebral hypoperfusion, could produce hippocampal neuronal loss 49 or severe white matter pathological changes. 50 In addition, a clinical study of patients who met research and clinical criteria for vascular dementia revealed that fewer than 20% of family members described a stepwise pattern of cognitive decline. 51 Again, consistency between diagnostic criteria, with regard to the natural history, onset, and evolution of the disease, is required.
Possible, Probable, and Definite Vascular Dementia
In contrast to other criteria, both the ADDTC and NINDS-AIREN criteria proposed different levels of certainty for the diagnosis of vascular dementia, with the terms “possible” and “probable” and “definite” vascular dementia. Neuroimaging evidence of vascular lesions and autopsy validation are respectively required for a diagnosis of probable vascular dementia and definite vascular dementia. For these two sets of criteria the difference between a possible and a probable diagnosis lies in the absence versus presence of confirming cerebral imaging data, the number of cerebrovascular accidents (several of which are more related to probable dementia), and in a typical versus atypical (plateau or amelioration) course or evolution of the disease. However, the lack of consideration of subtypes of vascular dementia according to CT or MRI findings by several diagnostic criteria such as the DSM, ICD-10, Hachinski Ischemic Scale, and Ischemic Scale of Rosen still has an impact on current case detection.
Subtypes of Vascular Dementia
According to Erkinjuntti, 52 classification of vascular dementia may be based on the primary vascular etiology, the primary type of ischemic brain lesions, the primary location of brain lesions, and the primary clinical syndrome. However, the currently proposed subtypes of vascular dementia—multi-infarct dementia, subcortical vascular dementia and strategic infarct dementia—incorporate a variable combination of the given categories, thus reflecting heterogeneity in the diagnosis of vascular dementia. None of the current clinical criteria for vascular dementia include a detailed description of these subtypes. Indeed, the ischemic scales do not mention anything in this regard, whereas the DSM criteria do not specify any subtypes related to different cerebrovascular disease mechanisms, and the ICD-10 includes six poorly described clinical subtypes. According to the ADDTC criteria, the classification of ischemic vascular dementia should specify features of the infarcts that may differentiate the disorder (i.e., location, size, distribution, severity, and etiology) but only for research purposes. The NINDS-AIREN criteria list a series of stroke lesions that may be associated with vascular dementia ( Table 1 ), but do not provide detailed descriptions of each subtype. Therefore, there is no agreement on a classification system for the vascular dementia subtypes. In fact, little research has been realized up to now comparing vascular dementia subtypes on important variables such as the pattern and severity of cognitive or functional impairment, the relationship to stroke risk factors, demographic variables, course of dementia, and cognitive syndrome. 53
Neuropathological Validation of the Diagnostic Criteria
There is currently an absence of widely accepted neuropathological markers of vascular dementia 54 as well as a heterogeneity in the pathological examination procedure used in various centers for diagnosing vascular dementia. 55 Another difficulty lies in determining, postmortem, whether a vascular lesion was causal, contributory, or coincidental to the dementia. 56 Although there is a general agreement that some types of vascular lesions are associated with cognitive impairments, 57 – 60 no consensus about the meaning of the term “vascular” has yet been reached, as is the case for the neuropathological characteristics of Alzheimer’s disease. 61 The ADDTC and NINDS-AIREN criteria only indicated a histopathological confirmation of the presence of multiple cerebral infarcts. Standards for the type, location, and extent of lesions required for vascular dementia or subtypes of vascular dementia are not yet agreed upon, whether it is for neuroimaging or autopsy findings. The degree to which infarcts or vascular lesions found in a patient contribute to dementia also remains to be determined. Moreover, in the field of neurodegenerative dementias, vascular lesions are frequently reported to be associated with Alzheimer’s disease, exaggerating the cognitive deficits of both disorders 62 and leading to a more rapid progression in Alzheimer’s disease. 63 Mixed cerebrovascular disease and Alzheimer-type pathology are indeed common at postmortem, accounting for approximately 25%–35% of cases of late-onset dementia. 64 Cerebrovascular diseases lesions (i.e., cerebral amyloid angiopathy, endothelial and vascular smooth muscle degeneration, macroscopic infarction, microinfarction, hemorrhage, and white matter changes) are found in at least one third of patients with Alzheimer’s disease, and pathological changes normally consistent with Alzheimer’s disease are found in at least one third of patients with vascular dementia. 65 Therefore, the absence of clearly defined neurobiological markers of vascular dementia constitutes a major limitation of all current clinico-pathological studies, which impedes the “gold standard” verification of a vascular dementia diagnosis.
DISCUSSION
To our knowledge, this is the first qualitative review aimed at describing and comparing the symptom requirements of eight different clinical criteria used for the diagnosis of vascular dementia. Critical issues regarding the definition of the cognitive syndrome and the vascular causes were differentially described in an effort to contrast them with current evidence reported in literature. To require the primacy of memory impairment in vascular dementia, an aspect not established on an empirical basis, induces problems that Looi and Sachdev 28 underlined a few years ago. These problems include: some patients with significant cognitive decline will not be diagnosed as having vascular dementia if their memory functioning is relatively well-preserved; in requiring memory impairment, the criteria may result in selection of the more severely cognitively impaired patients, precluding attempts at primary prevention; and the heterogeneity of cognitive impairment due to cerebrovascular lesions is likely to be underemphasized.
The reliability of the clinical diagnosis of Alzheimer’s disease has partially derived from the predictable nature and location of its neuropathology, 66 which typically starts in the limbic system and affects episodic memory primarily and most severely. Such has not been the case with respect to the diagnostic criteria for vascular dementia. Neuropathological validation was seldom carried out before the implementation of the criteria. All these clinical diagnostic criteria have been consensus criteria that were neither derived from prospective community-based studies with clinico-pathological correlations of vascular factors affecting cognition nor based on detailed natural histories. 67 , 68 In fact, the absence of a single, generally accepted, highly effective diagnostic methodology for vascular dementia clearly suggests a lack of consensus among clinicians and researchers, 69 and has made it very difficult to develop criteria for a prodromal state of vascular dementia. In addition, the available diagnostic criteria were all based on the ischemic infarct concept and have had limited validation. 68 , 70 The specification of the neuropathological requirements for the diagnosis of vascular dementia and its subtypes may help to shed some light on the current controversy regarding the existence and nature of vascular dementia. Indeed, the absence of neuropathological criteria has led to skepticism about the existence of pure vascular dementia cases. Some authors believe that vascular dementia only exists along a continuum between Alzheimer’s disease and vascular dementia 65 and that pure vascular dementia is rare, while others believe that Alzheimer’s disease is a vascular disorder. 71 More importantly, because Alzheimer’s disease is more common in older people than vascular dementia, it is argued that the occurrence of stroke merely unmasks latent Alzheimer’s disease and calls attention to its subtle cognitive impairment that had not been recognized easily before the stroke. Both Tomlinson et al. 72 and Hulette et al. 73 suggested that pure vascular dementia is uncommon at brain autopsy, and more recent neuropathologic findings showed that mixed Alzheimer’s disease/vascular dementia is more common. 74 , 75 Therefore, the cases of vascular dementia identified in the literature may result from mixed Alzheimer’s disease/vascular dementia pathology and thus prove difficult to distinguish from Alzheimer’s disease on neuropsychological testing. 28
This crucial debate may stem from the considerable heterogeneity in the concept of vascular dementia. Indeed, dementia may arise from a number of mechanisms and different vascular lesions as underlined above. The more prevalent types of cerebrovascular disorders (i.e., large artery disease, small vessel disease, cardiac embolic events, and hemodynamic mechanisms) may thus be associated with a particular neuropsychological profile and a particular course of illness. It is also possible that these different diagnostic criteria capture different thresholds or even subtypes of vascular dementia. 70 Therefore, it may be appropriate to abandon or at least narrow the classical concept of vascular dementia 76 by specifying cognitive profiles associated with different types of vascular conditions. Heterogeneous concepts such as vascular dementia with multiple subsyndromes typically result in poor prognostic value and confusion in the literature especially from a neuropsychological point of view. 76 In addition, it is very unlikely that there will be one single treatment or one single prodromal cognitive stage associated with vascular dementia. Recently, it was suggested to divide vascular dementia into more homogeneous, predictable, and reproducible subtypes, which would improve the comparability between studies and be more practical in clinical settings than the current criteria. 3 Erkinjuntti et al. 77 proposed to focus on subcortical vascular dementia and presented criteria in accordance with this subtype. This new classification incorporates small vessel disease as the primary vascular etiology, lacunar infarcts and ischemic white matter lesions as the primary type of brain lesions, subcortical location as the primary location of lesions, and frontal-subcortical syndrome as the primary clinical syndrome. 3 Another suggestion would be to apply the concept of vascular dementia only to stable conditions in which progressive neuronal dysfunction due to vascular lesions or factors is associated with a progressive overall decline in cognitive functioning (i.e., cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy). 76 The stable conditions would be the chronic condition after a stroke or after a treatable infection, all cognitive domains being dependent on the location and nature of the underlying lesion. 76 In this case, the term poststroke dementia could be applied. These distinctions are important since both subcortical vascular dementia and poststroke dementia are easily identifiable in clinical settings 78 —poststroke dementia because of an onset of cognitive decline in close temporal relationship with a transient ischemic attack or stroke event (although further refinement is needed because of various symptomatology and etiology) and subcortical vascular dementia because of the above mentioned reasons. A third and undoubtedly important subtype or “supertype” of vascular dementia, but much more difficult to identify than the first two subtypes, would be mixed Alzheimer’s disease/vascular dementia, presenting with heterogeneous clinical picture and etiology. 78
CONCLUSION
In conclusion, several sets of clinical criteria have been proposed to decrease subjectivity and disagreement among clinicians in establishing the diagnosis of vascular dementia. However, none of these criteria have been satisfactorily validated by longitudinal prospective studies. Most of them depend on first diagnosing dementia using the Alzheimer-type criteria, based on memory deficits, upon which are superimposed vascular events, usually following a stroke model (i.e., abrupt onset, stepwise deterioration). This is probably inappropriate, as memory loss is not always prominent in vascular dementia, and strokes are not the only etiology of vascular dementia. Finally, there are no accepted and widely used neuropathological markers of vascular dementia or subtypes of vascular dementia. There is now a vital need for an international agreement on clinical criteria for the diagnosis of vascular dementia as well as subtypes of vascular dementia that would take into consideration the heterogeneous nature of the vascular mechanisms; the subtypes would be disease entities with their own typical pathological and clinical features, and would be responsive to particular therapies. The definition of the cognitive syndrome, as well as the method for its assessment, and the definition of the vascular causes, as well as their associated vascular lesions on cerebral imaging, are thus of crucial importance.
1 . Jorm AF, O’Brien J: The epidemiology of vascular dementia: an overview and commentary, in Cerebrovascular Disease, Cognitive Impairment and Dementia, 2nd ed. Edited by O’Brien J, Ames D, Gustafson L, et al. London, Martin Dunitz, 2004, pp 95–100Google Scholar
2 . Bowler JV, Hachinski V: Criteria for vascular dementia: replacing dogma with data. Arch Neurol 2000; 57:170–171Google Scholar
3 . Erkinjuntti T, Inzitari D, Pantoni L, et al: Limitations of clinical criteria for the diagnosis of vascular dementia in clinical trials: is a focus on subcortical vascular dementia a solution? Ann N Y Acad Sci 2000; 903:262–272Google Scholar
4 . Hachinski V, Lassen NA, Marshall J: Multi-infarct dementia: a cause of mental deterioration in the elderly. Lancet 1974; 27:207–210Google Scholar
5 . Pasquier F, Leys D: Why are stroke patients prone to develop dementia? J Neurol 1997; 244:135–142Google Scholar
6 . Skoog I: Status of risk factors for vascular dementia. Neuroepidemiology 1998; 17:2–9Google Scholar
7 . Tatemichi TK: How acute brain failure becomes chronic: a view of the mechanisms and syndromes of the dementia related to stroke. Neurology 1990; 40:1652–1659Google Scholar
8 . Petersen RC, Smith GE, Waring SC, et al: Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 1999; 56:303–308Google Scholar
9 . Bowler JV, Hachinski V (eds): Vascular Cognitive Impairment: Preventable Dementia. Oxford, England, Oxford University Press, 2003Google Scholar
10 . Hachinski V: Vascular dementia: a radical redefinition. Dement Geriatr Cogn Disord 1994; 5:130–132Google Scholar
11 . Ringman JM, Cummings JL: Current and emerging pharmacological treatment options for dementia. Behavioral Neurol 2006; 17:5–16Google Scholar
12 . McKhann G, Drachman, Folstein M, et al: Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of the Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984; 34:939–944Google Scholar
13 . Holmes C, Cairns N, Lantos P, et al: Validity of current clinical criteria for Alzheimer’s disease, vascular dementia and dementia with Lewy bodies. Br J Psychiatry 1999; 174:45–50Google Scholar
14 . Jobst KA, Barnetson LP, Shepstone BJ: Accurate prediction of histologically confirmed Alzheimer’s disease and the differential diagnosis of dementia: the use of NINCDS-ADRDA and DSM-III-R criteria, SPECT, X-ray CT, and Apo E4 in medial temporal lobe dementias. Oxford Project to Investigate Memory and Aging. Int Psychogeriatr 1998; 10:271–302Google Scholar
15 . Nagy Z, Esiri MM, Hindley NJ, et al: Accuracy of clinical operational diagnostic criteria for Alzheimer’s disease in relation to different pathological diagnostic protocols. Dement Geriatr Cogn Disord 1998; 9:219–226Google Scholar
16 . Petersen RC: Mild cognitive impairment as a diagnostic entity. J Intern Med 2004; 256:183–194Google Scholar
17 . Hachinski VC, Iliff LD, Zilhka E, et al: Cerebral blood flow in dementia. Arch Neurol 1975; 32:632–637Google Scholar
18 . Rosen WG, Terry RD, Fuld PA, et al: Pathological verification of ischemic score in differentiation of dementias. Ann Neurol 1980; 7:486–488Google Scholar
19 . Chui HC, Victoroff JI, Margolin D, et al: Criteria for the diagnosis of ischemic vascular dementia proposed by the state of California Alzheimer’s disease diagnostic and treatment centers. Neurology 1992; 42:473–480Google Scholar
20 . Román GC, Tatemichi TK, Erkinjuntti T, et al: Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN international workshop. Neurology 1993; 43:250–260Google Scholar
21 . Wiederkehr S, Simard M, Fortin C, et al: Validity of the clinical diagnostic criteria for vascular dementia: a critical review. Part II. J Neuropsychiatry Clin Neurosci 2008; 20:162–177Google Scholar
22 . Luchsinger JA, Reitz C, Honig LS, et al: Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology 2005; 65:545–551Google Scholar
23 . Pavlik V, Hyman D, Doody R: Cardiovascular risk factors and cognitive function in adults 30–59 years old (NHANES III). Neuroepidemiology 2005; 24:42–50Google Scholar
24 . Chen CF, Lan SH, Khor GT, et al: Cognitive dysfunction after acute lacunar infarct. Kaohsiung J Med Sci 2005; 21:267–271Google Scholar
25 . Nys GM, Van Zandvoort MJ, De Kort PL, et al: Domain-specific recovery after first-ever stroke: a follow-up study of 111 cases. J Int Neuropsychol Soc 2005; 11:795–806Google Scholar
26 . Nys GM, Van Zandvoort MJ, De Kort PL, et al: The prognostic value of domain-specific cognitive abilities in acute first-ever stroke. Neurology 2005; 64:821–827Google Scholar
27 . Charlton RA, Morris RG, Nitkunan A, et al: The cognitive profiles of cadasil and sporadic small vessel disease. Neurology 2006; 66:1523–1526Google Scholar
28 . Looi JCL, Sachdev PS: Differentiation of vascular dementia from AD on neuropsychological tests. Neurology 1999; 53:670–678Google Scholar
29 . Poore QE, Rapport LJ, Fuerst DR, et al: Word list generation performance in Alzheimer’s disease and vascular dementia: neuropsychology, development, and cognition. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 2006; 13:86–94Google Scholar
30 . Knopman D, Boland LL, Mosley T, et al: Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology 2001; 56:42–48Google Scholar
31 . Saxby BK, McKeith IG, Ford GA, et al: Effects of hypertension on attention, memory, and executive function in older adults. Health Psychol 2003; 22:587–591Google Scholar
32 . Ylikoski R, Ylikoski A, Raininko R, et al: Cardiovascular diseases, health status, brain imaging findings and neuropsychological functioning in neurologically healthy elderly individuals. Arch Gerontol Geriatr 2000; 30:115–130Google Scholar
33 . Wiederkehr S, Simard M: Facteurs de risque vasculaires et cognition chez la personne âgée: revue sélective de la littérature et présentation d’une échelle de risques vasculaire cognitive. Age et Nutrition 2007; 18:1–10Google Scholar
34 . Stephens S, Kenny RA, Rowan E, et al: Neuropsychological characteristics of mild vascular cognitive impairment and dementia after stroke. Int J Geriatr Psychiatry 2004; 19:1053–1057Google Scholar
35 . Zanetti M, Ballabio C, Abbate C, et al: Mild cognitive impairment subtypes and vascular dementia in community-dwelling elderly people: a 3-year follow-up study. J Am Geriatr Soc 2006; 54:580–586Google Scholar
36 . McPherson SE, Cummings JL: Neuropsychological aspects of vascular dementia. Brain Cogn 1996; 31:261–282Google Scholar
37 . McKeith IG, Galasko D, Kosaka K, et al: Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology 1996; 47:1113–1124Google Scholar
38 . McKeith IG, Dickson DW, Lowe J, et al: Diagnosis and management of dementia with Lewy bodies: third report of the DLB consortium. Neurology 2005; 65:1863–1872Google Scholar
39 . Simard M, van Reekum R, Cohen T: A review of the cognitive and behavioral symptoms in dementia with lewy bodies. J Neuropsychiatry Clin Neurosci 2000; 12:425–450Google Scholar
40 . Simard M, van Reekum R, Myran D: Visuospatial impairment in dementia with Lewy bodies and Alzheimer’s disease: a process analysis approach. Int J Geriatr Psychiatry 2003; 18:387–391Google Scholar
41 . Simard M, van Reekum R, Myran D, et al: Differential memory impairment in dementia with Lewy bodies and Alzheimer’s disease. Brain Cogn 2002; 49:244–249Google Scholar
42 . Neary D, Snowden JS, Gustafson L, et al: Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology 1998; 51:1546–1554Google Scholar
43 . Desmond DW: The neuropsychology of vascular cognitive impairment: is there a specific cognitive deficit? J Neurol Sci 2004; 226:3–7Google Scholar
44 . Desmond DW, Erkinjuntti T, Sano M, et al: The cognitive syndrome of vascular dementia: implications for clinical trials. Alzheimer Dis Assoc Disord 1999; 13:21–29Google Scholar
45 . Amar K, Wilcock G: Vascular dementia. Br Med J 1996; 312:227–231Google Scholar
46 . Brun A: Pathology and pathophysiology of cerebrovascular dementia: pure subgroups of obstructive and hypoperfusive etiology. Dementia 1994; 5:145–147Google Scholar
47 . Knopman DS, Parisi JE, Boeve BF, et al: Vascular dementia in a population-based autopsy study. Arch Neurol 2003; 60:569–575Google Scholar
48 . Longstreth WTJ, Bernick C, Manolio TA, et al: Lacunar infarcts defined by magnetic resonance imaging of 3660 elderly people: the cardiovascular health study. Arch Neurol 1998; 55:1217–1225Google Scholar
49 . Fein G, Di Sclafani V, Tanabe J, et al: Hippocampal and cortical atrophy predict dementia in subcortical ischemic vascular disease. Neurology 2000; 55:1626–1635Google Scholar
50 . Esiri MM, Wilcock GK, Morris JH: Neuropathological assessment of the lesions of significance in vascular dementia. J Neurol Neurosurg Psychiatry 1997; 63:749–753Google Scholar
51 . Paul R, Moser D, Cohen R, et al: Dementia severity and pattern of cognitive performance in vascular dementia. Applied Neuropsychology 2001; 8:221–217Google Scholar
52 . Erkinjuntti T: Classification and criteria, in Cerebrovascular Disease and Dementia: Pathology, Neuropsychiatry, and Management. Edited by Chui E, Gustafson L, Ames D, et al. London, Martin Dunitz, 2000, pp 99–113Google Scholar
53 . Nyenhuis DL, Gorelick PB: Vascular dementia: a contemporary review of epidemiology, diagnosis, prevention, and treatment. J Am Geriatr Soc 1998; 46:1437–1448Google Scholar
54 . Jellinger KA: Pathology and pathophysiology of vascular cognitive impairment: a critical update. Panminerva Med 2004; 46:217–226Google Scholar
55 . Pantoni L, Sarti C, Alafuzoff I, et al: Postmortem examination of vascular lesions in cognitive impairment: a survey among neuropathological services. Stroke 2006; 37:1005–1009Google Scholar
56 . Chui H: Neuropathology lessons in vascular dementia. Alzheimer Dis Assoc Disord 2005; 19:45–52Google Scholar
57 . Jellinger KA: Understanding the pathology of vascular cognitive impairment. J Neurol Sci 2005; 15: 57–63, 229–330Google Scholar
58 . Mori E: Impact of subcortical ischemic lesions on behavior and cognition. Ann N Y Acad Sci 2002; 977:141–148Google Scholar
59 . Swartz RH, Black SE, Sela G, et al: Cognitive impairment in dementia: correlations with atrophy and cerebrovascular disease quantified by magnetic resonance imaging. Brain Cogn 2002; 49:228–232Google Scholar
60 . Traykov L, Baudic S, Thibaudet M-C, et al: Neuropsychological deficit in early subcortical vascular dementia: comparison to Alzheimer’s disease. Dement Geriatr Cogn Disord 2002; 14:26–32Google Scholar
61 . Mirra SS, Heyman A, McKeel D, et al: The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part II: standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 1991; 41:479–486Google Scholar
62 . Snowdon DA, Greiner LH, Mortimer JA, et al: Brain infarction and the clinical expression of Alzheimer disease: the nun study. JAMA 1997; 277:813–817Google Scholar
63 . Pasquier F, Leys D, Scheltens P: The influence of coincidental vascular pathology on symptomatology and course of Alzheimer’s disease. J Neural Transm Suppl 1998; 54:117–127Google Scholar
64 . Arvanitakis Z, Hachinski V: Vascular cognitive impairment: what else do the authors need to learn? in Alzheimer Disease, 2nd ed. Edited by Terry RD, Katzman R, Bick KL, et al. Philadelphia, Lippincott Williams & Wilkins, 1999, pp 147–160Google Scholar
65 . Kalaria RN, Ballard C: Overlap between pathology of Alzheimer disease and vascular dementia. Alzheimer Dis Assoc Disord 1999; 13:115–123Google Scholar
66 . Arnold SE, Hyman BT, Flory J, et al: The topographical and neuroanatomical distribution of neurofibrillary tangles and neuritic plaques in the cerebral cortex of patients with Alzheimer’s disease. Cereb Cortex 1991; 1:103–116Google Scholar
67 . Erkinjuntti T: Clinical criteria for vascular dementia: the NINDS-AIREN criteria. Dement Geriatr Cogn Disord 1994; 5:189–192Google Scholar
68 . Rockwood K, Parhad I, Hachinski V, et al: Diagnosis of vascular dementia: consortium of canadian centres for clinical cognitive research concensus statement. Can J Neurol Sci 1994; 21:358–364Google Scholar
69 . Gold G, Giannakopoulos P, Montes-Paixao S, et al: Sensitivity and specificity of newly proposed clinical criteria for possible vascular dementia. Neurology 1997; 49:690–694Google Scholar
70 . Erkinjuntti T, Ostbye T, Steenhuis R, et al: The effect of different diagnostic criteria on the prevalence of dementia. N Engl J Med 1997; 337:1667–1674Google Scholar
71 . De la Torre JC: Alzheimer’s disease is a vasocognopathy: a new term to describe its nature. Neurol Res 2004; 26:517–524Google Scholar
72 . Tomlinson BE, Blessed G, Roth M: Observations on the brains of demented old people. J Neurol Sci 1970; 11:205–242Google Scholar
73 . Hulette C, Nochlin D, McKeel D, et al: Clinical-neuropathologic findings in multi-infarct dementia: a report of six autopsied cases. Neurology 1997; 48:668–672Google Scholar
74 . Victoroff J, Mack WJ, Lyness SA, et al: Multicenter clinicopathological correlation in dementia. Am J Psychiatry 1995; 152:1476–1484Google Scholar
75 . Neuropathology Group, Medical Research Council Cognitive Function and Aging Study: Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS). Lancet 2001; 357:169–175Google Scholar
76 . de Haan EH, Nys GM, Van Zandvoort MJ: Cognitive function following stroke and vascular cognitive impairment. Curr Opin Neurol 2006; 19:559–564Google Scholar
77 . Erkinjuntti T, Inzitari D, Pantoni L, et al: Research criteria for subcortical vascular dementia in clinical trials. J Neural Transm Suppl 2000; 59:23–30Google Scholar
78 . Wallin A, Milos V, Sjögren M, et al: Classification and subtypes of vascular dementia. Int Psychogeriatr 2003; 15:27–37Google Scholar



