Erotomania After Aneurysmal Subarachnoid Hemorrhage
Abstract
A woman developed the delusional syndrome of erotomania 4 years after subarachnoid hemorrhage from a ruptured basilar artery aneurysm. The authors review the literature on erotomania in association with neurologic and medical conditions. Although no cause-and-effect relationship can be established between the neurologic event and erotomania in this patient, the possible neuropsychiatric correlates of this syndrome highlight the need for careful attention to neurologic and medical factors in future cases. Available information suggests that diffuse brain dysfunction may contribute to erotomania, perhaps by interfering with the operations of cerebral regions subserving complex emotional function.
Erotomania is the delusional belief that another person, usually of some social prominence, has fallen in love with the patient. The patient believes that this other person was the first to declare his or her intentions, often by special glances, signals, telepathy, or messages through the media. Usually the patient “returns” this affection by means of letters, phone calls, gifts, and visits. Even though these advances are unexpected and unwanted, any denial of affection by the object of this delusional love is dismissed by the patient as a ploy to conceal the forbidden love from the rest of the world. If the patient presses on in pursuing this delusion of a romantic relationship, the ensuing conflict may eventually come to the attention of the mental health system, the police, and the courts, not always in that order.
Although most cases of erotomania are seen in isolation or associated with schizophrenia or mood disorder, this syndrome may also occur in a variety of other settings. We present the case of a woman who developed erotomania following the rupture and surgical repair of a basilar artery aneurysm, and we review the literature of this delusional disorder in association with neurologic and medical conditions.
CASE REPORT
This 48-year-old right-handed Korean-born woman presented in 1987, at age 39, with sudden onset of headache and alteration of consciousness. Computed tomography (CT) of the head showed extensive subarachnoid hemorrhage, and cerebral arteriography demonstrated an aneurysm of the tip of the basilar artery. Subsequently, the aneurysm was surgically clipped via a right subfrontal craniotomy. A CT scan on the first postoperative day showed a right frontoparietal subdural hematoma, which was evacuated via the same craniotomy. One week later, a left frontal ventriculoperitoneal shunt was placed for persisting hydrocephalus. The patient recovered and was able to return to work after several months.
Four years after the hospitalization, the patient was treated for depression and was noted to comment about a romantic relationship that was “not working out.” It became evident she believed that a physician at the hospital where she worked was in love with her. She based this belief on the “special” look he had given her in the hospital cafeteria. There was no known prior contact between the patient and this physician. He denied any romantic inclinations, but the patient persisted in her belief. She sent gifts, made phone calls, and visited the office where he practiced. This behavior continued despite ongoing psychotherapy, treatment with neuroleptics, and a restraining order. After multiple violations of the restraining order, she was committed to a psychiatric hospital.
On admission in 1996, she was neat in appearance and had good eye contact. She steadfastly held to her belief that the physician loved her and would return her affections if he were not constrained by his job and family. She complained of recurring depressive symptoms with fleeting suicidal ideation, and dull, diffuse headaches. She denied appetite or sleep disturbance, anhedonia, crying spells, manic symptoms, anxiety, hallucinations, thought broadcasting, or thought insertion. She had some difficulty maintaining a coherent train of thought, but memory was intact, and language was normal in both Korean and English. Simple calculations, limb and facial praxis, figure and clock drawing, cortical sensory testing, Luria maneuvers, and alternating sequences were normal. Cranial nerves, power, tone, coordination, gait, reflexes, and sensation were intact.
Neuropsychological testing included the Wechsler Adult Intelligence Scale–Revised (WAIS-R), which revealed a Verbal IQ (VIQ) of 75, Performance IQ (PIQ) of 89, and Full Scale IQ (FSIQ) of 81. Testing with the Wechsler Memory Scale (WMS) yielded a memory quotient of 87. She obtained a score of 5 (borderline performance) on the Memory for Designs test. Evaluation with the Bender-Gestalt suggested difficulties with organizational abilities, and she had mild deficits with visual memory. Performance on the Trail Making Test was impaired, more so on Part B than Part A. The neuropsychologist who performed the tests felt these results represented the patient's premorbid level of function, based on her education, employment, and the fact that English was her second language.
CT scans were available from the initial illness and from 8 years later, when erotomania was fully established. The original scans indicated diffuse cerebral involvement from subarachnoid hemorrhage and hydrocephalus that was later corrected by a ventriculoperitoneal shunt.
Concurrent medical problems included non–insulin-dependent diabetes mellitus and peptic ulcer disease. Medications included risperidone, sertraline, metformin, and ranitidine. Past medical history included high blood pressure, osteoarthritis, cholecystectomy, and hysterectomy. She did not smoke and denied alcohol or drug use. She denied any family history of neurologic or psychiatric illness.
The patient was born in rural South Korea and received only 4 years of education before the outbreak of the Korean War. She had been hospitalized at the ages of 16 and 20 after suicide attempts by pill overdose. After marrying an American serviceman and coming to the United States at age 26 she had two children, and she later divorced this husband after 17 years of marriage. She remarried a year later, only to have her second husband die in 1995. She reported chronic feelings of loneliness and depression, leading to the psychiatric hospitalization 4 years earlier at the onset of her erotomanic delusion.
The patient also reported vivid memories of three near-death experiences. The first occurred when she was 8 years old; all of the children in the home, including the patient, were very ill with high fever, and one sister died. The second near-death experience occurred with a pill overdose at age 21, and the third with her ruptured aneurysm. She repeatedly stated her belief that God had worked through American doctors to make her live.
DISCUSSION
The rupture of aneurysms of the posterior circulation is a neurologic catastrophe associated with high morbidity and mortality.1 Psychiatric symptoms among survivors of subarachnoid hemorrhage are common; although psychotic or delusional symptoms are rare, most patients manifest depression or anxiety.2 In this case, erotomania developed after a Hunt grade three3 aneurysmal subarachnoid hemorrhage and has persisted despite treatment for 5 years. We first consider the syndrome of erotomania, then its association with neurologic and medical disorders, and finally the possible neuropsychiatric correlates of this syndrome.
Erotomania
This syndrome of the delusion of being loved has been labeled erotomania, de Clerambault's syndrome, psychose passionelle, amor insanus, delusional loving, old maid's insanity, and melancholia erotique. Erotomania should be distinguished from other forms of pathologic love. Excessive desire for coitus is termed nymphomania in women and satyriasis in men.4 The phantom lover syndrome is the delusion of being visited by a secret lover who does not exist.5 Obsessional love is more common than erotomania;6 in this syndrome the patient is equally obsessed with the love object but does not harbor the delusion that the object reciprocates this feeling. The term erotomania first appeared in 1640, although cases fitting this description can be found in the medical literature dating back to Hippocrates.7 The syndrome first enters the modern medical literature in 3 reports published in 1921.8–10 De Clerambault8 reported 5 cases, distinguishing between pure erotomania, when the syndrome occurs alone, and secondary erotomania, when the syndrome occurs in association with another psychiatric disorder. He believed the essential component of the syndrome was the sudden onset of the conviction of being in amorous communication with a person of much higher rank, who was the first to fall in love and the first to make advances. He suggested that the delusion fulfilled the demands of sexual pride that life had failed to provide. Kraepelin9 described the same syndrome as one of the variations of paranoia and suggested that the delusion served as a “psychological compensation for the disappointments of life.” Hart10 described a similar syndrome in elderly unmarried women, emphasizing the persecutory aspects of the delusion; he named this “old maid's insanity.”
In the last 75 years, there have been numerous reports of erotomania occurring in both men11,12 and women,13 who may be young13 or old,14 sexually and socially active13 or isolated,14 and heterosexual15 or homosexual.16 Classification of the syndrome has been controversial; some authorities maintain that erotomania occurs alone,17,18 and others contend that the pure syndrome is rarely if ever seen and is usually a component of a more generalized disorder, frequently paranoid schizophrenia or bipolar disorder.19 At present, erotomania is classified as a subtype of delusional disorder.20
Neurologic and Medical Conditions
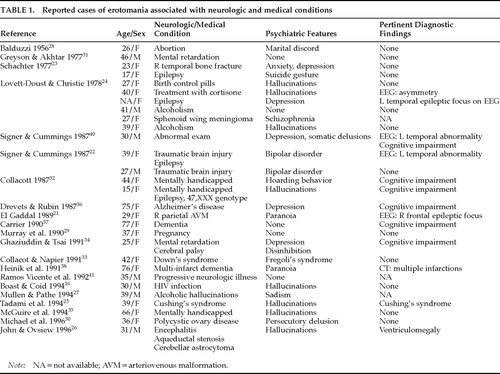
Whereas the majority of reported cases of erotomania appear either in isolation or with other psychiatric pathology, there are also cases associated with neurologic and medical conditions. Table 1 lists 29 cases in addition to ours that suggest such an association. These cases were selected from a comprehensive literature review and are discussed in detail to illustrate the wide variety of potential predisposing conditions.
Subarachnoid Hemorrhage
In addition to our case, we found one other report of erotomania associated with subarachnoid bleeding. El Gaddal21 described a woman who developed an erotomanic delusion following resection of a right parietal arteriovenous malformation that hemorrhaged. She also had paranoid ideation, seizures, left homonymous hemianopia, and left hemiparesis. An electroencephalogram (EEG) showed a right frontal epileptiform focus and a head CT scan was normal. Treatment with carbamazepine and neuroleptics reduced her paranoia but did not affect her erotomanic delusion.
Traumatic Brain Injury
Signer and Cummings22 reported two cases. The first was a woman with a history of bipolar features who developed an erotomanic delusion about another woman. This patient had sustained a traumatic brain injury as a child and had residual right hemiparesis and complex partial seizures with secondary generalization. Neuropsychological testing revealed mild memory and visuospatial disturbances. A head CT scan was normal, and an EEG showed left temporal slowing. Their second case was a man with a history of multiple head injuries and bipolar disorder. Neurologic and neuropsychological evaluations were normal. He was “slightly better” following treatment with lithium, but was lost to follow-up. Schachter23 reported the case of a woman who developed the delusion that a man was in love with her. As this delusion was clearing, having been present for 14 years, she suffered a head injury with a right temporal bone fracture that was followed by a renewed erotomanic delusion directed at a different man. A Rorschach test was interpreted to show psychological factors that explained the syndrome. No other neurological information was presented.
Seizure Disorder
Schachter23 reported a woman with seizures who developed an erotomanic delusion that lasted several months. She refused any diagnostic evaluation. Lovett-Doust and Christie24 reported the case of a woman with an erotomanic attachment to her priest. She had depressive symptoms, but no prior psychiatric history. She was given the diagnosis of psychomotor epilepsy based on the EEG finding of a “small epileptic focus in the (L) temporal area.” There is no mention of her actually having seizures.
Endocrinologic Conditions
Lovett-Doust and Christie24 described a woman who developed an erotomanic attachment to her singing teacher 5 weeks after starting birth control pills. She suffered hallucinations and was described as confused. Evaluation included an EEG and “other tests” that were unrevealing. The delusion persisted for months after the oral contraceptives were stopped; it diminished after treatment with phenothiazines. These authors reported a woman who developed the delusion that a woman friend was in love with her, shortly after treatment with cortisone for eczema.24 She also had auditory hallucinations. Evaluation included three EEGs that revealed greater amplitude on the right than the left. Neither discontinuation of the cortisone nor treatment with chlorpromazine affected the delusion, which remained intact 16 years later. Tadami et al.25 reported a woman who presented with erotomania, insomnia, and auditory hallucinations. The symptoms had been present for 2 years when she was diagnosed with Cushing's disease due to a pituitary microadenoma. Leukocytosis had been present from the time of her initial presentation and resolved with surgery for the microadenoma, suggesting that she had had Cushing's disease for the entire 2 years prior to diagnosis. Her psychiatric symptoms were slightly improved 15 months after surgery.
Brain Tumor
John and Ovsiew26 reported a man with an erotomanic attachment to a former school friend. His history included aqueductal stenosis with hydrocephalus treated with a ventriculoperitoneal shunt at the age of 3, encephalitis thought to be due to a reaction to smallpox vaccine, with 3 months of coma at age 6, and three surgical procedures for a pilocytic astrocytoma of the left cerebellar hemisphere between the ages of 13 and 21. His delusion emerged at age 30, six months after the death of his mother. He also had auditory hallucinations. Examination showed a pupil-sparing right third nerve palsy, cerebellar dysarthria, dystonic posturing of the right arm, and bilateral extensor plantar responses. Routine blood studies were normal, an EEG showed left temporal slowing, and a brain magnetic resonance imaging (MRI) scan demonstrated postoperative changes, dilated third and lateral ventricles, and recurrent tumor in the fourth ventricle. A single-photon emission computed tomography scan using [99mTc] HMPAO during a cognitive activating task (counting down from 100) revealed decreased activity in both temporal lobes, more pronounced in the inferior and posterior right temporal lobe. Neuropsychological testing identified impairment in attention, memory, visual perception, reading, math, abstraction, vocabulary, and fund of knowledge. His hallucinations and agitation improved with haloperidol, but his erotomanic delusion persisted at 6-month follow-up. A woman in Lovett-Doust and Christie's series24 had erotomania, history of schizophrenia, and a sphenoid wing meningioma found at autopsy. Neither the size nor the side of the tumor is reported. She had psychological testing that “showed organicity.”
Alcohol Abuse
Mullen and Pathe27 reported a man with alcohol dependence and hallucinosis who had an erotomanic attachment to a female social worker. Concomitant disorders included sexual sadism and a personality disorder. Two cases in Lovett-Doust and Christie's series24 were associated with alcohol. A man developed a delusional attachment to another man that fluctuated in intensity with heavy alcohol consumption. Their final case was a woman with an erotomanic delusion and hallucinations associated with heavy alcohol use. Her evaluation included normal laboratory studies and skull roentgenograms. Family history was notable for schizophrenia.
Gynecological Conditions
Erotomania associated with pregnancy has also been reported. Balduzzi28 reported a woman who developed an erotomanic attachment to the physician who performed her abortion, raising the question of an association with either the hormonal changes of pregnancy or the psychic trauma of the procedure as the trigger for the delusion. Murray et al.29 described a pregnant woman with no psychiatric history who developed the delusion that her obstetrician was in love with her and was communicating by psychic messages. This persisted for over 3 years. The report states that following treatment with trifluoperazine the patient refrained from contacting the physician for 18 months, but the status of the delusional belief is not discussed. Michael et al.30 reported a woman with polycystic ovary disease and both homosexual and heterosexual erotomania.
Infection
Boast and Coid16 reported a man with human immunodeficiency virus (HIV) infection who developed an erotomanic attachment to a male social worker. The patient had been HIV-positive for 5 years and had secondary syphilis and oral candidiasis. Limited neuropsychological testing and a head CT scan were normal. His delusion persisted despite treatment with pimozide. As he later developed further HIV-related illnesses, there was a dramatic improvement in psychiatric symptoms until his death from AIDS.
Developmental Delay
There are several reports of erotomania in developmentally delayed patients. Greyson and Akhtar31 described a man with mental retardation who developed the delusional belief that a woman loved and wished to marry him during a time when his parents were ill. This resolved with their recovery to good health, and then reemerged with another woman as the object of the delusion when his parents became ill and died. The etiology and severity of his retardation were not addressed. Collacott32 described two mentally handicapped patients with erotomanic attachments. The first was a woman with “multi-factorial” retardation. Her Clifton scale score was 12/12. She believed that a famous actor wished to marry her, and she had a good response to treatment with phenothiazines. The second patient was a woman with the 47,XXX genotype and tonic-clonic seizures who believed that the pop singer Chubby Checker was in love with her.32 She had a normal EEG and Wechsler Intelligence Scale for Children (WISC) FSIQ of 55. Her erotomanic attachment ended when another patient told her, incorrectly, that the singer was dead. She assaulted the bearer of the bad news. In a second report, Collacott and Napier33 reported a woman with Down's syndrome who developed an erotomanic attachment to her male Bible teacher; she also had the Fregoli's syndrome, in which a persecutor is believed to change faces. The delusion was still intact after 3 months despite treatment with neuroleptics. Ghaziuddin and Tsai34 reported a woman with spastic athetoid cerebral palsy and a Vineland Social Maturity Scale intellectual age of 75 months who developed an attachment to her male teacher while significantly depressed; the erotomanic delusion resolved as her depression cleared. McGuire et al.35 reported a mentally handicapped woman with no psychiatric history who developed erotomania. She had delusions and hallucinations that she was being sexually assaulted by several different men. It is not clear from the report that she believed any of these men were in love with her. Several years before, she had a WAIS VIQ of 61, PIQ of 92, and FSIQ of 73. A gynecological evaluation, EEG, and neurologic examination were all unrevealing. Treatment with pimozide led to resolution of symptoms over 6 months.
Dementia
Demented patients with erotomania have also been reported.36–38 Drevets and Rubin36 reported a woman with Alzheimer's disease who had the delusion that a young maintenance man at her apartment was in love with her. In addition to the erotomanic delusion, she had depressive symptoms, auditory and visual hallucinations, and ideas of reference. Treatment with nortriptyline, methylphenidate, vitamin B12, and ergot alkaloids did not affect her delusion, but the delusion did fade as she became progressively more demented. Carrier37 reported a woman with dementia who developed the delusion that she was loved by a priest she had met at a funeral. There was no evidence of formal thought disorder or affective symptoms, and no psychiatric history. She scored 27/30 on the Mini-Mental State Examination (MMSE),39 but results of the Hooper Visual Organization Test, the Reitan-Barter, and the Rorschach tests were “highly suggestive of mild to moderate dementia.” Heinik et al.38 reported a woman with multi-infarct dementia and the erotomanic delusion that the Prince of Wales had proposed marriage. She also held the belief that she had been married and separated from the former Israeli prime minister Shimon Peres. She scored 16/30 on the MMSE. Neurological examination revealed left visual neglect and left hyperreflexia. A head CT scan revealed bilateral lacunar infarctions, a right parieto-occipital infarct, and mild cortical atrophy. Laboratory studies were unremarkable.
Undefined Disorders
Signer and Cummings40 reported a man with an erotomanic delusion of 2 years' duration in addition to depressive symptoms and somatic delusions. He had verbal-motor dissociation with Luria maneuvers, poor word fluency, and an EEG showing “left temporal abnormalities.”
Ramos Vicente et al.41 reported a man with a “progressive neurologic illness” who developed the delusion that an English princess was in love with him and that they were to be married. This belief was based on special signs he claimed to receive from the photocopy machine he used at work. With neuroleptic treatment, he was described as “exhibiting no disturbance, and keeping himself under ambulatory control.” No further information is provided about his neurologic illness.
Neuropsychiatric Correlates
A major obstacle in evaluating potential neuropsychiatric correlates of erotomania is the paucity of neurologic and medical information provided with many case reports. A recent comprehensive textbook of neuropsychiatry could only conclude that erotomania can sometimes occur in individuals with “brain damage or epilepsy.”42 Although the literature on erotomania abounds with psychiatric detail and interpretation, neurologic and medical data, if collected, are usually given little emphasis. We believe that greater attention to these aspects of the cases would contribute significantly to the understanding of this syndrome.
The relationship between neurologic and medical conditions and erotomania remains uncertain. In our patient, 4 years elapsed between the neurologic insult and the onset of the delusion, making a causal link tenuous. She also had depressive symptoms when her erotomanic delusion developed and had previously had similar symptoms and several suicide attempts. Her psychological state, combined with her high regard for physicians, thus offers an alternative explanation for her delusion. The disorders reported in the cases we reviewed varied in severity, pathophysiology, and temporal relation to the development of the delusion. Some of the patients had other psychiatric problems, including schizophrenia, depression, mania, paranoia, and hallucinations. These disorders have also been associated with erotomania, confounding the etiologic link between neurologic and medical illness and erotomanic delusion. The combination of a neurologic or medical condition and a psychological predisposition may be necessary for the formation of this syndrome.
Representation of Emotion in the Brain
The anatomic representation of love, affection, and attachment in the human brain is not known. Damasio43 divides human emotion into the primary or “early” emotions and secondary or “adult” emotions. Examples of primary emotions are hunger and fear; secondary emotions include such feelings as altruism and friendship. The network of structures associated with the primary emotions is the limbic system, in particular the amygdala and the anterior cingulate gyrus.43,44 We would include sexual drive with the primary emotions because injury to the septal region45 and basal-frontal and diencephalic structures46 has been associated with hypersexuality.
Secondary emotions appear to involve prefrontal cortex and parietotemporal association cortices; these areas access memories and enable judgments that help interpret the actions of other individuals and the social context in which these events occur.43,47,48 In these secondary emotions, the brain regions involved in primary emotions are also required in order to manifest the autonomic and motoric expressions of an emotional response.
Considerable evidence suggests that certain emotional functions are lateralized to the right hemisphere.49 The recognition of facial expression50 and the emotional content or prosody of language51 are primarily mediated by the right hemisphere. Delusions and psychosis are associated with right hemisphere injury,52,53 and psychiatric disorders are more frequent after right-sided lesions.52,54 Two specific delusional disorders, Capgras syndrome and reduplicative paramnesia, have also been linked with lesions of the right hemisphere.53,55 Capgras syndrome is the delusion that familiar people have been replaced by identical strangers.56 Patients with reduplicative paramnesia hold the delusion that the place where they are currently located has been moved to another site.57 In some patients, a right hemisphere lesion is insufficient in itself to produce delusional or paranoid thinking, but must be superimposed on diffuse cerebral damage in order for this to occur.52
The 30 individuals we reviewed had no predominant site of cerebral pathology, although details were often unclear. In general, the neurologic and medical conditions tended to have a diffuse effect on the brain, and focal lesions were uncommon. Further study will be required to determine whether lesions confined to cerebral regions subserving emotion can also lead to erotomania.
Misinterpretation and Abnormal Belief
In patients with erotomania, there is a fundamental misinterpretation of another person's intent. The erotomanic perceives a look, a gesture, or a spoken or written word as containing a special and unique meaning. In our patient, this misinterpretation appears to have started with a look across a room. She interpreted an ordinary glance and facial expression as the look of “love at first sight.” This disturbed perception is clearly more complex than simply mistaking someone's expression; it may involve the participation of widespread cerebral networks, possibly with a right hemisphere predominance.
Misinterpretation or misunderstanding of other people's intentions is common. The normal course of action is to test and verify the veracity of the belief and to make appropriate corrections if the belief is in error. Despite total absence of confirmation, and in the face of often considerable evidence to the contrary, patients with erotomania hold firmly to their delusional system. A striking feature of erotomania is the duration of the delusional belief, which may persist for decades in the absence of any reinforcement.14 This belief is abnormal in its initial formation, its resistance to test for external validation, and its failure to extinguish when shown to be incorrect. These features imply that brain dysfunction contributes to this syndrome. Erotomania may therefore represent an opportunity to investigate the cerebral operations involved in the formation and persistence of delusional thinking and the representation of emotional function in the human brain.
 |
1. Schievink WI, Wijdicks EFM, Piepgras DG, et al: The poor prognosis of ruptured intracranial aneurysms of the posterior circulation. J Neurosurg 1995; 82:791–795Crossref, Medline, Google Scholar
2. Storey PB: Psychiatric sequelae of subarachnoid hemorrhage. British Medical Journal 1967; 3:261–266Crossref, Medline, Google Scholar
3. Hunt WE, Kosnick JP: Timing and perioperative care in intracranial aneurysm surgery. Clin Neurosurg 1974; 21:79–89Crossref, Medline, Google Scholar
4. Kaplan HI, Sadock BJ: Paraphilias and sexual disorder NOS, in Synopsis of Psychiatry, 7th edition, edited by Kaplan HI, Sadock BJ. Baltimore, Williams and Wilkins, 1994, pp 674–681Google Scholar
5. Seeman MV: Delusional loving. Arch Gen Psychiatry 1978; 35:1265–1267Crossref, Medline, Google Scholar
6. Zona MA, Sharma KK, Lane J: A comparative study of erotomanic and obsessional subjects in a forensic sample. J Forensic Sci 1993; 38:894–903Medline, Google Scholar
7. Enoch MO: De Clerambault's syndrome, in Uncommon Psychiatric Syndromes, 3rd edition, edited by Enoch MO, Trethowan WH. Cambridge, UK, Butterworth-Heinemann, 1991, pp 24–50Google Scholar
8. De Clerambault CG: Oeuvre Psychiatrique. Paris, Presses Universitaires de France, 1942Google Scholar
9. Kraepelin E: Manic Depressive Insanity and Paranoia, translated by Barclay M, edited by Robertson E. Edinburgh, Livingston, 1921Google Scholar
10. Hart B: The Psychology of Insanity. Cambridge, UK, Cambridge University Press, 1921Google Scholar
11. Taylor P, Mahendra B, Gunn J: Erotomania in males. Psychol Med 1983; 13:645–650Crossref, Medline, Google Scholar
12. Goldstein RL:More forensic romances: de Clerambault's syndrome in men. Bull Am Acad Psychiatry Law 1987; 15:267–274Medline, Google Scholar
13. Giannini AJ, Slaby AE, Robb TO: De Clerambault's syndrome in sexually experienced women. J Clin Psychiatry 1991; 52:84–86Medline, Google Scholar
14. Retterstol N, Opjordsmoen S: Erotomania: erotic self-reference psychosis in old maids, a long-term follow-up. Psychopathology 1991; 24:388–397Crossref, Medline, Google Scholar
15. Segal JH: Erotomania revisited: from Kraepelin to DSM-III-R (review). Am J Psychiatry 1989; 146:1261–1266Crossref, Medline, Google Scholar
16. Boast N, Coid J: Homosexual erotomania and HIV infection. Br J Psychiatry 1994; 164:842–846Crossref, Medline, Google Scholar
17. Munro AM: De Clerambault's syndrome: a nosological entity (letter). Br J Psychiatry 1985; 146:561Crossref, Medline, Google Scholar
18. Rudden M, Gilmore M, Frances A: Erotomania: a separate entity. Am J Psychiatry 1980; 137:1262–1263Crossref, Medline, Google Scholar
19. Ellis P, Mellsop G: De Clerambault's syndrome: a nosological entity? Br J Psychiatry 1985; 146:90–95Google Scholar
20. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Washington, DC, American Psychiatric Association, 1994Google Scholar
21. El Gaddal YY: De Clerambault's syndrome (erotomania) in organic delusional syndrome. Br J Psychiatry 1989; 154:714–716Crossref, Medline, Google Scholar
22. Signer SF, Cummings JL: De Clerambault's syndrome in organic affective disorder: two cases. Br J Psychiatry 1987; 151:404–407Crossref, Medline, Google Scholar
23. Schachter M: Erotomania or the delusional conviction of being loved: contribution to the psychopathology of the love life [French]. Ann Med Psychol 1977; 1:729–747Medline, Google Scholar
24. Lovett-Doust JW, Christie H: The pathology of love: some clinical variants of de Clerambault's syndrome. Soc Sci Med 1978; 12:99–106Medline, Google Scholar
25. Tadami S, Murata A, Wakabayashi T, et al: A case of Cushing's disease: hallucinatory paranoid state preceding physical symptoms [Japanese]. Seishin Shinkeigaku Zasshi 1994; 96:461–468Medline, Google Scholar
26. John S, Ovsiew F: Erotomania in a brain-damaged male. J Intellect Disabil Res 1996; 40:279–283Crossref, Medline, Google Scholar
27. Mullen PE, Pathe M: The pathological extensions of love. Br J Psychiatry 1994; 165:614–623Crossref, Medline, Google Scholar
28. Balduzzi E: Un caso di erotomania passionale pura secondu Clerambault [A case of pure passional erotomania after Clerambault]. Riu Sperim di Freniatria 1956; 80:407–426Google Scholar
29. Murray D, Harwood P, Eapen E: Erotomania in relation to childbirth [see comments]. Br J Psychiatry 1990; 156:896–898Crossref, Medline, Google Scholar
30. Michael A, Zolese G, Dinan TG: Bisexual erotomania with polycystic ovary disease. Psychopathology 1996; 29:181–183Crossref, Medline, Google Scholar
31. Greyson B, Akhtar S: Erotomanic delusions in a mentally retarded patient. Am J Psychiatry 1977; 143:325–326Google Scholar
32. Collacott RA: Erotomanic delusions in mentally handicapped patients: two case reports. Journal of Mental Deficiency Research 1987; 31:87–92Medline, Google Scholar
33. Collacott RA, Napier EM: Erotomania and Fregoli-like state in Down's syndrome: dynamic and developmental aspects. Journal of Mental Deficiency Research 1991; 35(pt 5):481–486Google Scholar
34. Ghaziuddin M, Tsai L: Depression-dependent erotomanic delusions in a mentally handicapped woman. Br J Psychiatry 1991; 158:127–129Crossref, Medline, Google Scholar
35. McGuire BE, Akuffo E, Choon GL: Somatic sexual hallucinations and erotomanic delusions in a mentally handicapped woman. J Intellect Disabil Res 1994; 38:79–83Crossref, Medline, Google Scholar
36. Drevets WC, Rubin EH: Erotomania and senile dementia of Alzheimer type. Br J Psychiatry 1987; 151:400–402Crossref, Medline, Google Scholar
37. Carrier L: Erotomania and senile dementia (letter). Am J Psychiatry 1990; 147:1092Medline, Google Scholar
38. Heinik J, Aharon-Peretz J, Hes JP: De Clerambault's syndrome in multi-infarct dementia. Psychiatria Fennica 1991; 22:23–26Google Scholar
39. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
40. Signer SS, Cummings JL: Erotomania and cerebral dysfunction (letter). Br J Psychiatry 1987; 151:275Medline, Google Scholar
41. Ramos Vicente YM, Seijo JCC, Martinez IL: De Clerambault's syndrome. J Clin Psychiatry 1992; 53:138–139Medline, Google Scholar
42. Benson DF, Gorman DG: Hallucinations and delusional thinking, in Neuropsychiatry, edited by Fogel BS, Schiffer RB, Rao SM. Baltimore, Williams and Wilkins, 1996, pp 307–323Google Scholar
43. Damasio AR: Descartes' Error. New York, Grosset/Putnam, 1994Google Scholar
44. Devinsky O, Morrell MJ, Vogt BA: Contributions of the anterior cingulate cortex to behaviour. Brain 1995; 118:279–306Crossref, Medline, Google Scholar
45. Gorman DG, Cummings JL: Hypersexuality following septal injury. Arch Neurol 1992; 49:308–310Crossref, Medline, Google Scholar
46. Miller BL, Cummings JL, McIntyre H, et al: Hypersexuality or altered sexual preference following brain injury. J Neurol Neurosurg Psychiatry 1986; 49:867–873Crossref, Medline, Google Scholar
47. Damasio H, Damasio AR: The neural basis of memory, language and behavioral guidance: advances with the lesion method in humans. Seminars in Neuroscience 1990; 2:277–286Google Scholar
48. Eslinger PJ, Damasio AR: Severe disturbance of higher cognition after bilateral frontal lobe ablation: patient EVR. Neurology 1985; 35:1731–1741Crossref, Medline, Google Scholar
49. Bear DM: Hemispheric specialization and the neurology of emotion. Arch Neurol 1983; 40:195–202Crossref, Medline, Google Scholar
50. Ley RG, Bryden MP: Hemispheric differences in processing emotions and faces. Brain Lang 1979; 7:127–138Crossref, Medline, Google Scholar
51. Ley RG, Bryden MP: A dissociation of right and left hemispheric effects for recognizing emotional tone and verbal content. Brain Cogn 1982; 1:3–9Crossref, Medline, Google Scholar
52. Levine DN, Grek A: The anatomic basis of delusions after right cerebral infarction. Neurology 1984; 34:577–582Crossref, Medline, Google Scholar
53. Fleminger S, Burns A: The delusional misidentification syndromes in patients with and without evidence of organic cerebral disorder: a structured review of case reports. Biol Psychiatry 1993; 33:22–32Crossref, Medline, Google Scholar
54. Price BH, Mesulam M-M: Psychiatric manifestations of right hemisphere infarctions. J Nerv Ment Dis 1985; 173:610–614Crossref, Medline, Google Scholar
55. Wilcox J, Wazari R: The Capgras symptom and nondominant cerebral dysfunction. J Clin Psychiatry 1983; 44:70–72Medline, Google Scholar
56. Capgras J, Reboul-Lachaux J: Illusion des sosies dans un delire systematisé chronique [Illusion of doubles in a chronic systematized delusion]. Bulletin de la Société Clinique de Médicine Mentale 1923; 2:6–16Google Scholar
57. Filley CM, Jarvis PE: Delayed reduplicative paramnesia. Neurology 1987; 37:701–703Crossref, Medline, Google Scholar