Abstracts
POSTER PRESENTATIONS
ABBREVIATIONS
The abbreviations defined below are used frequently within the abstracts.
AD=Alzheimer's disease; ADD=attention deficit disorder; ADHD=attention-deficit/hyperactivity disorder; ADRDA=Alzheimer's Disease and Related Disorders Association; AIDS=acquired immunodeficiency syndrome; ANOVA=analysis of variance; BDI=Beck Depression Inventory; CSF=cerebrospinal fluid; CT=computed tomography; 18FDG=[18F]fluorodeoxyglucose; fMRI=functional MRI; FSIQ=Full Scale IQ; Ham-A=Hamilton Anxiety Scale; Ham-D=Hamilton Rating Scale for Depression; HD=Huntington's disease; HIV=human immunodeficiency virus, type 1; MANOVA=multivariate analysis of variance; MMPI=Minnesota Multiphasic Personality Inventory; MMSE=Mini-Mental State Examination; MRI=magnetic resonance imaging; MS=multiple sclerosis; MTBI=mild traumatic brain injury; NARSAD=National Alliance for Research on Schizophrenia and Depression; NIA=National Institute on Aging; NIAAA=National Institute on Alcohol Abuse and Alcoholism; NIDRR=National Institute on Disability and Rehabilitation Research; NIH=National Institutes of Health; NIMH=National Institute of Mental Health; NINDS=National Institute of Neurological Disorders and Stroke; PD=Parkinson's disease; PET=positron emission tomography; PIQ=Performance IQ; PTSD=posttraumatic stress disorder; SPECT=single-photon emission computed tomography; SSRI=selective serotonin reuptake inhibitor; TBI=traumatic brain injury; UPDRS=Unified Parkinson's Disease Rating Scale; VA=Veterans Affairs; VIQ=Verbal IQ; WCST=Wisconsin Card Sorting Test; WMS=Wechsler Memory Scale.
Pediatric Neuropsychiatry and Neuropsychology
P1. Growth curve analyses of neuropsychological profiles of children with neurofibromatosis type 1 (NF1): specific cognitive functions remain “spared” and “impaired” over timeLaurie E. Cutting, Christine W. Koth, Guan-Hua Huang, Scott L. Zeger, Martha B. Denckla (Kennedy Krieger Institute, Johns Hopkins School of Medicine, and Johns Hopkins School of Hygiene and Public Health, Baltimore, MD)
Background: Cognitive deficits in neurofibromatosis type 1 have been documented in both the verbal and visuospatial domains. Previous investigations have determined a specific pattern of “spared” performance (Picture Arrangement, Picture Completion, and Rapid Automatized Naming) and “impaired” performance (Judgment of Line Orientation [JLO], Vocabulary, and Block Design) on cognitive tests in this population as compared with sibling matched control subjects in pairwise designs. Methods: To further investigate the nature and the growth pattern of these spared and impaired functions longitudinally, we conducted growth curve analyses on these cognitive tests in 7 patients with NF1 and their siblings. Results: Results indicated that over time children with NF1 do not “catch” up to their siblings on those functions that are impaired and they continue to perform similarly to their siblings on the spared functions: they continued to have significantly lower scores than their siblings on Vocabulary, Block Design, and JLO, and they remained not significantly different from their siblings on Picture Arrangement, Picture Completion, and Rapid Automatized Naming. With respect to growth rates, on average across the six cognitive functions there was no significant difference between the groups; however, the growth rate of the JLO appeared to be marginally significantly faster (P=0.0504) in NF1 probands than in their siblings at certain periods. Conclusions: The pattern of “spared” and “impaired” cognitive functions that appears to be specific to NF1, spanning the verbal and visuospatial domains, was confirmed longitudinally. There was also some suggestion of temporarily faster growth rates on the JLO exhibited by NF1 probands compared with their siblings.Support from NIH Grants P50 NS35359 and ND07414-07.
P2. Risperidone and posttraumatic stress disorder in boysJoseph P. Horrigan, L. Jarrett Barnhill (University of North Carolina, Chapel Hill, NC)
Background: Risperidone has become a popular pharmacotherapy for various neuropsychiatric disorders in childhood, including autism and Tourette's disorder (Bruun et al., J Clin Psychiatry 1996; 57:29–31). Anecdotal reports have suggested that risperidone may be useful in the treatment of PTSD in adults (Leyba et al., Psychiatr Serv 1998; 49:245–246). Reported here is a case series involving the use of risperidone in boys with severe PTSD. Methods: 18 boys (mean age 9.28 yr) with PTSD, in residential treatment, were administered risperidone in an open-label fashion. The risperidone was initiated at 0.5 mg po bid and titrated to optimal clinical response across the next 16 weeks. Clinical measurements included serial Conners scales (Conners, Psychopharmacol Bull 1973; special issue) as well as sleep data. Results: 15 of 18 boys (83%) proved to be robust responders to the risperidone, with a mean decrease in the Conners score from 22.5 to 12.2 (P<0.01). Sleep latency shortened by an average of 45 min. The mean effective dose of risperidone was 1.37 mg/day. None of the boys experienced either acute or chronic side effects, other than varying degrees of weight gain. Conclusions: Risperidone may be effective in the management of the disruptive behavior and disturbed sleep that often accompany PTSD in boys. Side effects appear to be minimal in the short term. Larger studies with more rigorous designs will be needed to confirm these findings.
P3. Clinical and neurobiological correlates of cytogenetic abnormalities in childhood-onset psychosesRob Nicolson, Jay N. Giedd, Tom Fernandez, Jeff Bedwell, Marge Lenane, Judith L. Rapoport (Child Psychiatry Branch, NIMH, Bethesda, MD)
Background: Although various cytogenetic abnormalities have been reported to be increased in schizophrenia, their role in the disorder is unknown. The purpose of this study was to investigate clinical and neurobiological correlates of chromosome abnormalities in childhood-onset psychoses. Methods: From a group of 73 patients with childhood-onset psychoses, clinical and neurobiological correlates of chromosomal abnormalities were examined in 6 patients with cytogenetic anomalies. These patients were compared to 67 patients with childhood-onset psychoses and normal cytogenetic test results on behavioral measures, neuropsychological functioning, smooth pursuit eye movements (SPEM), and brain morphometry. Results: Patients with cytogenetic abnormalities did not differ in age at onset, clinical features, neuropsychological functioning, or measures of SPEM. Patients with chromosomal anomalies had larger lateral ventricles; other brain structures did not differ. Conclusions: With the exception of increased ventricular volume, these patients with childhood-onset psychotic disorders and cytogenetic abnormalities were otherwise typical of the larger cohort of childhood-onset psychotic patients. Psychoses are most likely a final common pathway for a variety of genetic abnormalities.
P4. Case study: use of cognitive behavior therapy (CBT) for posttraumatic stress disorder in a 4-year-old with anoxic traumatic brain injuryKathleen M. O'Toole (Department of Neuropsychology, Scottish Rite Children's Medical Center, Atlanta, GA)
Background: Inpatient rehabilitation practices for pediatric patients with traumatic brain injury are well established (Prigatano, Traumatic Brain Injury: Mechanisms of Damage, Assessment, Intervention, and Outcome, Pro-ed, 1990); the treatment of accompanying PTSD is not. Psychological interventions using only behavior management and family counseling can be ineffective if PTSD is not addressed (Famularo et al., Child Abuse Negl 1996; 20:953–961). Methods: A 4-year-old male was hospitalized for 2 months with severe TBI from physical abuse. He had also been sexually abused. He refused to eat or be touched by therapists. He was cortically blind and agitated. He met DSM-IV criteria for PTSD. Individual psychotherapy using CBT (Davidson & March, Psychiatry, vol 2, WB Saunders, 1996) and co-therapy with speech, occupational, and physical therapies were used. Family members were included in treatment to increase generalization of outcome. Child psychiatry supplemented treatment with clonidine 0.025 mg toward the end of the hospital stay. Results: The child showed diminished symptoms of PTSD and increased eating and other functional activities. Cognitive functioning improved but remained within the deficient range because of TBI. Family involvement increased, as well as their understanding of underlying trauma interfering with rehabilitation efforts. Conclusions: It is crucial to diagnose and treat PTSD for optimal functional outcome in pediatric TBI. CBT appears to be a useful treatment in PTSD management in a complex pediatric case.
P5. Validity of the 6-11-Parent Rating Scale (PRS) of the Behavior Assessment System for Children (BASC), Spanish version, in the diagnosis of attention deficit disorder plus hyperactivity (ADD/+H) in Colombian childrenDavid A. Pineda, Randy Kamphaus, Isabel C. Puerta, Ofelia Mora, Luis G. Palacio, Ivan Jiménez, Mauricio Garcia, Silvia Mejia (University of Antioquia, Medellín, Colombia)
Background: The BASC is a multimethod and multidimensional approach to evaluating the behavior of children. Its rating scales have been validated on the diagnosis of ADD/+H in North American children. Methods: We selected 25 DSM-IV ADD/+H (combined subtype) male 6- to 11-yr-old children and 25 age-, sex-, and socioeconomic status (SES)-matched control children. ADD/+H children met the DSM-IV criteria for the combined subtype, and the diagnosis was confirmed by a multiprofessional staff (neurologist, psychiatrist, psychologist, and neuropsychologist). The control children were selected in a randomized approach from the same schools as the cases, and none met the DSM-IV criteria for ADD diagnosis. All children were from the high SES. The mean years of age of the ADD/+H and control children were 8.16±1.5. School grades were 2.6±1.9 in ADD/+H and 2.16±1.4 in control children. BASC-PRS (6-11) (AGS) Spanish authorized version questionnaires were completed by parents in both groups. The questionnaires were scored by BASC software and the raw scores were used for the statistical analysis. Results: On the clinical scale, ADD/+H children had significantly higher scores (MANOVA, P<0.05) in hyperactivity, conduct problems, and attention problems. On the adaptive scale, the only significant difference found was on social skills, with lower score in the ADD/+H group. A multiple regression analysis selected hyperactivity and attention problem as the best model for predicting groups (Ad-R2=0.42, P<0.0001). A discriminant analysis with these variables found a discriminant function with attention problem loading (R=0.73) and with a symmetrical predictive capability of 84% for each group. Conclusions: Our results demonstrated the validity of this multidimensional questionnaire on the screening diagnosis of ADD/+H children.
P6. Validity of the 6-l1-Teacher Rating Scale (TRS) of the Behavior Assessment System for Children (BASC), Spanish version, in the diagnosis of attention deficit disorder plus hyperactivity (ADD/+H) in Colombian childrenDavid A. Pineda, Randy Kamphaus, Isabel C. Puerta, Ofelia Mora, Luis G. Palacio, Ivan Jiménez, Mauricio Garcia, Silvia Mejia (University of Antioquia, Medellín, Colombia)
Background: The BASC is a multimethod and multidimensional approach to evaluating the behavior of children. Its rating scales have been validated in the diagnosis of ADD/+H in North American children. Methods: We selected 25 DSM-IV ADD/+H (combined subtype) male 6- to 11-year-old children and 25 age-, sex-, and socioeconomic status (SES)-matched control children. ADD/+H children met the DSM-IV criteria for the combined subtype, and the diagnosis was confirmed by a multiprofessional staff (neurologist, psychiatrist, psychologist, and neuropsychologist). The control children were selected in a randomized approach from the same schools as the cases, and none met the DSM-IV criteria for ADD diagnosis. All children were from the high SES. The mean years of age of the ADD/+H and control children were 8.16±1.5. School grades were 2.6±1.9 in ADD/+H and 2.16±1.4 in control children. BASC-TRS (6-11) (AGS) Spanish authorized version questionnaires were completed by teachers in both groups. The questionnaires were scored by BASC software and the raw scores were used for the statistical analysis. Results: On the clinical scale, ADD/+H children had significantly higher scores (MANOVA, P<0.05) in hyperactivity, aggression, conduct problems, depression, attention problems, learning problems, and atypicality. On the adaptive scale, significant differences on leadership and social skills were found, with lower scores in the ADD/+H group. A multiple regression analysis selected hyperactivity, aggression, depression, attention problems, learning problems, adaptability, and social skills as the best model for predicting groups (Ad-R2=0.53, P<0.0001). A discriminant analysis with these variables found a discriminant function with hyperactivity loading R=0.94 and with social skills loading R=–0.81. This function had a predictive capability of 84% for classifying control group and 88% for ADD/+H group. Conclusions: Our results demonstrated that this multidimensional questionnaire is very sensitive for the screening diagnosis of ADD/+H children.
P7. Attention-deficit/hyperactivity disorder (ADHD) and affect regulationWarren D. Rosen, John A. Bartok (Rush-Presbyterian-St. Luke's Medical Center, Chicago, IL)
Background: Diagnostic criteria of ADHD continue to be questioned. Parents of children with ADHD often describe emotional dysregulation, which is not a criterion for diagnosis. Overlapping neuropsychological constructs (attention and executive functioning) and overlapping/communicating neurological systems suggest a relationship between attentional and emotional dysregulation. Methods: 100 ADHD cases, inattentive type (ADD) or impulsive/hyperactive type (ADHD) between ages 5 and 18, with IQ >75, seen in a pediatric neuropsychology clinic were selected. Records were reviewed to identify possible emotional dysregulation from the diagnostic formulations developed from clinical observation and parent report (Conners, PIC, and Behavior Assessment System for Children [BASC]). Results: 33% of children with ADD and 78% with ADHD were identified as showing affective dysregulation. Of these, 64% with ADD and 50% with ADHD were also diagnosed with executive dysfunction. Conclusions: Affect regulation is conceptually and clinically a frequent, central component of a child's attention disorder, with differentially greater presence in ADHD than ADD. This finding may confirm the suggestion that ADD and ADHD are separate nosological entities. Pharmacologic, behavioral, and/or psychotherapeutic treatment of ADHD must address this component. Variations in quality of affective dysregulation will be discussed. It is crucial to determine diagnostic centrality of emotional dysregulation in future research.
Clinical Neuropsychiatry and Treatment
P8. Estrogen as an antidepressant: neurobiology, clinical applications, and an experimental modelCelso Agner, Rochelle S. Cohen, Moises Gavíria, Thomas Jobe (Departments of Anatomy/Cell Biology and Psychiatry, University of Illinois at Chicago, IL)
Background: Major depression affects a large proportion of the human population. Its prevalence is higher in women; moreover, the incidence increases over lifetime in women without estrogen replacement therapy (ERT). This fact, along with the amelioration of depressive symptoms in women after estrogen, stimulated the research into (and subsequent application of) several different forms of administration of estrogen to those patients. Methods: To narrow down the pathways of estrogen effects on depression, an animal model, the forced swim test, was selected because of its similarity to human depression (learned helplessness) and because of known estrogen effects on animal behavior in this paradigm. Estrogen has been shown to present the same effects as antidepressants in this model. Results: The results of studies using this model suggest that the effects of estrogen on the brain include 1) acute effects, through the action of estrogen on cytoplastic and nuclear receptors in neurons, and/or activation of second messenger systems such as cAMP, NOS, and PPI; 2) chronic effects, through the action on transcription factors such as CREB; and 3) vascular effects, either by an acute effect on vascular receptors or by the action on transcription factors present in endothelial cells and the surrounding glia. Comments: We will present this model to test the hypothesis that estrogen has profound effects as an antidepressant in rats. The study conducted will be the start of a process to determine the exact role of estrogen's antidepressant effects in women.
P9. Mood versus neurovegetative symptoms in Alzheimer's diseaseJim Andrikopoulos (Mercy Ruan Neuropsychology Clinic, Des Moines, IA).
Background: The prevalence of depressive symptoms in Alzheimer's disease suggests clinical depression in AD is common. Using the Geriatric Depression Scale (GDS), this study hypothesizes that neurovegetative, not mood, symptoms best account for positive GDS scores. Methods: 100 consecutive AD patients were studied. A score of 10 or greater on the GDS reflected depression. Ten items were identified from previous studies as mood items. The percentage of patients endorsing these items was calculated. For patients with positive GDS scores, the mood items were rescored in the negative direction to determine what percentage of patients remain classified as depressed when mood items are denied. Results: On average, 80% of the sample denied mood symptoms. 38% of the sample had positive GDS scores. With the mood items rescored, 11% of patients were reclassified as nondepressed, leaving 27% of the sample with positive GDS scores. Conclusions: The findings suggest AD patients infrequently endorse mood items. With the rescoring of mood items, the 27% of patients that still had positive GDS scores reflects the endorsement of neurovegetative items. Positive GDS scores are likely accounted for by neurovegetative symptoms that reflect organic personality changes associated with the disease rather than clinical depression.
P10. Post–temporal lobectomy mood disorders in patients with medically refractory complex partial seizure disorderL. Jarrett Barnhill, Robert Beach, Bradford Walters, Jean Wilkens (University of North Carolina, Chapel Hill, NC)
Background: The relationship between complex partial seizures and mood disorders is influenced by lateralization of seizure onset, treatment resistance, polypharmacy, genetic vulnerability to mood disorders, and limitations in social and occupational capacities. Medically refractory patients referred for epilepsy surgery are screened for primary psychopathology and cognitive deficits. Postoperative depression appears to fall into two subtypes: early-onset and later onset postoperative depression. The later onset group has characteristics of major depression, previous episodes, or family history of affective disorders. Methods: Clinical case studies will be presented to represent both subtypes of postoperative mood disorders. The presentation will emphasize features of epilepsy, past psychiatric history, and associated cognitive disabilities. Results: Postoperative mood disorders complicate social recovery and rehabilitation. The early-onset group reaches a peak incidence within weeks of surgery, resolving within 6 months. Later onset depression is indistinguishable from functional affective disorder. Treatment approaches for late-onset depression will be outlined. Conclusions: Postoperative depression contributes to significant social morbidity. Although fear of recurring seizures is common, this stress seems unrelated to late-onset mood disorder. Treatment requirements differ between these subtypes.
P11. Violent behavior in female inpatientsL. Jarrett Barnhill, Joseph P. Horrigan (University of North Carolina, Chapel Hill, NC)
Background: Violent behavior in women is commonly associated with mood disorders, luteal phase disorders, and psychosis. Personality disorders linked to aggression are complicated by histories of severe abuse and neglect, especially in patients with Cluster B disorders. Associated neurological soft signs and history of drug abuse will be reviewed in a group of women judged not guilty by reason of insanity or incompetent to stand trial for violent behavior due to mental illness. Methods: The patient sample includes 6 women currently treated in a forensic treatment unit that specializes in treatment-resistant violent patients. Developmental history, psychopathology, neurological examination, and treatment response will be compared. Results: Violent homicidal behavior is associated with histories of severe abuse and neglect, apparent dissociative episode, and a tendency toward luteal exacerbation of aggression or disruptive behaviors. Cognitive limitations, positive symptoms of psychosis, and family history of addiction are reported. Comments: A group of treatment-resistant, violent females will be presented. Each has periods of intense affective reactivity, with reported hallucinations and trauma. End luteal phase aggression is also prominent. Treatment approaches will be discussed.
P12. Co-occurrence of psychiatric symptoms in acute and chronic oculogyric crisisSheldon Benjamin, Craig M. Coldwell (University of Massachusetts Medical School, Worcester, MA)
Background: The association of psychiatric symptoms with oculogyric crisis (OGC), well known in encephalitis lethargica, has only occasionally been reported in neuroleptic-induced OGC. Methods: 10 cases of chronically recurring OGC were identified in the neuropsychiatry clinic of a state hospital and a tertiary care hospital over 10 years. Neuropsychiatric histories and examinations were performed, detailed descriptions of oculogyric attacks were obtained, and subjects were interviewed for presence of concurrent psychiatric symptoms during attacks. 2 cases of acute OGC were also evaluated. All patients received anticholinergic treatment following diagnosis. Results: 10/10 chronically recurring OGC cases were found to include stereotyped psychiatric symptoms during attacks. All patients had more than 5 years of neuroleptic exposure. In no case had the association been recognized. Half were not recognized to have OGC at all, but were believed to have periodic exacerbations of their psychiatric disorders. In all cases, both the OGC and associated psychiatric symptoms resolved quickly with anticholinergic treatment. 2 patients suffering from acute OGC were found to have the same association. Conclusions: The association of stereotyped psychiatric symptoms with chronically recurring neuroleptic-induced OGC is not unusual and may also be found in acute OGC. The psychiatric symptoms, like the dystonia, respond to anticholinergic treatment.
P13. Use of mirtazapine for behavioral problems in Alzheimer's diseaseCharles Bernick, Samir Saxena (University of Nevada School of Medicine, Las Vegas, NV)
Background: Behavioral problems in Alzheimer's disease are common and often difficult to manage; the pharmacological therapy is mainly empiric. Mirtazapine is a relatively new antidepressant that works by antagonism of central alpha-2 receptors (Burrows et al., J Clin Psychopharmacol 1997; 17[suppl 1]:34S–39S). Although its role in the management of Alzheimer's disease is undefined, we believe it may be a useful drug for the treatment of agitated behaviors in these patients. Methods: 8 consecutive patients with Alzheimer's disease of moderate severity (MMSE 10–20) with agitated behaviors were placed on mirtazapine at doses ranging from 15 to 30 mg/day. Behavioral change was assessed by comparing scores on the Neuropsychiatric Inventory prior to starting mirtazapine and after 4 to 8 weeks of active treatment. No additional psychotropic drugs or behavioral interventions were allowed during the study period. Results: 6 of 8 patients with agitation, 5 of 7 patients with irritability, and 5 of 7 patients with depression/dysphoria showed improvement. 4 of the 5 patients with delusions also improved. Caregiver distress decreased concomitantly. Beneficial effects on anxiety (4/6 patients), nighttime behavior (4/5 patients), and appetite (3/5 patients) were observed. Conclusions: This pilot study indicates that mirtazapine may be an effective therapeutic option for management of disruptive behaviors, including delusions, in Alzheimer's disease. Additional, more rigorous studies are warranted.
P14. Obsessive-compulsive disorder (OCD) and related personality disorders associated with supratentorial arachnoid cysts (SAC): behavioral, cognitive, and SPECT findingsMarcelo L. Berthier, Angel Posada, Carmen Puentes, Belen Gonzalez Jiménez (Clinic University Hospital and Carlos Haya Regional Hospital, Málaga, Spain)
Background: While accumulating evidence suggests that individuals with SAC are predisposed to develop neuropsychiatric disorders during childhood and adolescence (i.e., ADHD, Tourettism), there are no studies of obsessive-compulsive disorder in patients with supratentorial arachnoid cysts. Our objective was to report 5 patients with SAC who had a lifelong history of OCD and abnormal personality traits. Methods: 5 male patients (age range 26–53 yr, mean age at OCD onset 17.4 yr) with SAC involving the temporal (n=4) or the frontal lobe (n=1) and OCD and abnormal personality traits were studied with standardized psychiatric rating scales (Yale-Brown Obsessive-Compulsive Scale, MMPI), cognitive tests susceptible to frontosubcortical dysfunction, and [99mTc]HMPAO SPECT. Results: The most frequent symptoms of OCD in all 5 patients were symmetry/exactness, hoarding, and somatic obsessions and multiple compulsions. All 5 patients also met DSM-IV criteria for mixed personality disorder, and 3 of them showed an MMPI profile characterized by elevations of scales 2, 7, and 8, indicating obsessive-compulsive personality disorder. Cognitive testing demonstrated impaired performance on frontal lobe tasks, and SPECT revealed that 4 patients had bilateral hypoperfusion in morphological spared regions of the dorsolateral prefrontal, inferior frontal, orbitofrontal, and temporal cortices. The other patient had hypoperfusion in the left frontotemporal region. Conclusions: Our findings provide some clues to the developmental neurobiology of OCD and related personality disorders. Developmental brain lesions involving the temporal and/or frontal cortices may be implicated in the pathogenesis of early-onset OCD and related abnormal personality traits by inducing both local changes (i.e., decreased cortical volume due to dysgenesis) and remote functional derangements in interconnected orbital corticolimbic systems.
P15. Improved cognitive function in multiple sclerosis patients receiving methylphenidate and cognitive remediationAndrea Friedman, Michael K. Matthews, Jr., Fred Lublin (MCP/Hahnemann School of Medicine, Philadelphia, PA)
Background: 50% of patients with multiple sclerosis have cognitive impairments, mainly in short-term memory, divided attention, concentration, speed of information processing, verbal fluency, and problem solving. These symptoms resemble those reported in attention deficit disorder. We reasoned that stimulant treatment, useful in attention deficit disorder, might help in MS also. Methods: We administered the Perceived Cognitive Problems Questionnaire (PCPQ), MMSE, and BDI to 20 successive MS patients referred to our Cognitive Recovery Program due to complaints of cognitive impairment. Patients learned cognitive remediation strategies and began methylphenidate 5 mg bid at 4-hour intervals. Methylphenidate doses were adjusted based on patients' judgments of benefit. One month after a stable dose of methylphenidate was achieved, the three measures were repeated. Results: Most patients reported improvement in daily cognitive functioning, and there was a significant improvement in their scores on the PCPQ. BDI and MMSE scores were more variable. Conclusions: Methylphenidate in conjunction with cognitive remediation strategies may provide symptomatic improvement in the cognitive impairments of MS. Future research efforts should dissect the independent effects of methylphenidate versus cognitive remediation strategies alone in treating cognitive impairments in MS.
P16. The neuropsychiatric report: an integrative display of imaging and clinical neuropsychiatric dataBrad Dickerson, Juan Carlos Rivas, Moises Gavíria, Dan Pavel (University of Illinois College of Medicine, Chicago, IL)
Background: The integration of neuroanatomical, neurophysiological, and neuropsychological data is a characteristic skill of the neuropsychiatrist/behavioral neurologist. However, the union of such disparate data often faces obstacles. To improve data integration in a clinical setting, we developed a model “neuropsychiatric report,” which employs readily available computer software, provides concise feedback to the referral source, and improves multidisciplinary collaboration. Methods: Our goal was to display clinical MRI, SPECT, EEG, and neuropsychological data—and their interpretation—on a two-page report. This was accomplished by using a standard personal computer, software, and the hospital network along with standard imaging, electrophysiologic, and cognitive instruments, which are detailed in the poster. An illustrative case is presented. Results: The neuropsychiatric report was well accepted by the various teams involved in the patient's care. It was successfully used as a basis for discussion, allowing all specialists to review the same data prior to a multidisciplinary conference. Conclusions: This approach allows the integration of neuropsychiatric and imaging data in a convenient format for presentation and discussion. The computer-based format enables easy transformation of these cases into teaching files. In addition, the application of this method to remote consultation—local, national, and international—is being pursued via the Internet.
P17. Psychotherapeutic treatment of patients with nonepileptic seizures (NES)James M. Hill, Gabriela E. Höhn (UMDNJ-New Jersey Medical School, Newark, NJ)
Background: Much of the literature on nonepileptic seizures has focused on assessment and diagnosis. Although a variety of treatment approaches have been recommended, including behavior management, hypnosis, milieu therapy, individual therapy, pharmacotherapy and family therapy, there is little literature on the psychotherapeutic management of these patients. This presentation will describe a pragmatic approach to treating patients with NES. Methods: The psychotherapeutic treatment of 10 patients (6 children, 4 adults) diagnosed by EEG/video monitoring was reviewed to elucidate treatment approaches and interventions used. Results: Response of NES patients to psychotherapy is highly variable. An approach that integrates behavioral and family therapy techniques appears most effective in reducing NES events. Response to these approaches appears partially dependent on age and reinforcing factors for the NES. Conclusions: Psychotherapy can be a valuable intervention in terms of positive outcome and contribution to quality of life for these patients. Approaches to clinical management and research on therapeutic efficacy in this population are presented.
P18. Phytoestrogens in the treatment of the cognitive and somatic symptoms of menopauseGail Hochanadel, Jan Shifren, Irina Zhdanova, Tim Maher, Paul A. Spiers (Clinical Research Center, Massachusetts Institute of Technology, Cambridge, MA)
Background: Estrogen replacement therapy has been shown to be effective in treating the somatic and cognitive changes associated with menopause. Recent research has suggested that diets high in plant-derived estrogenic isoflavones, “phytoestrogens,” may also ameliorate some of these somatic symptoms, particularly hot flashes. There are no prior studies of the effect of these compounds on cognitive functioning. Methods: This was an unequally randomized double-blind placebo-controlled crossover single-center pilot study to investigate the effect of dietary phytoestrogen supplementation on somatic, mood, and cognitive disturbances associated with naturally occurring menopause. The metabolic parameters, somatic symptoms, and verbal learning performance of naturally postmenopausal women were measured while they consumed daily doses of 100 mg of an encapsulated soy isoflavone extract for 12 weeks. Results: None of the statistical comparisons between the active and placebo conditions yielded findings in support of the hypothesis that phytoestrogens may be useful for the treatment of these hormone-mediated cognitive or somatic changes.Support from the Center for Brain Sciences and the Metabolism Charitable Trust, Massachusetts Institute of Technology.
P19. Analysis of the causal complexity of stroke by “fuzzy” statisticsThomas H. Jobe (Chicago, IL)
Background: The classical definitions of ischemic stroke subtypes are based on mutually exclusive causal mechanisms: atherosclerotic, cardioembolic, lacunar, and “other.” Because of the sequential nature of diagnostic algorithms, the clinician is forced to choose one potential mechanism rather than various combinations of several interacting pathophysiologies. This is because degree of presence of the disease and concomitancy are not represented in classical probability-based statistics. This study shows how 163 ischemic stroke patients can be more fully represented by use of fuzzy statistics that do take into account degree of presence and concomitancy of occurrence. Methods: Two blinded stroke experts assigned a fuzzy information “fit” value (0,1) to the results of three broad categories of tests: heart tests, blood coagulation studies, and vascular occlusion studies. Results: 163 patient sets were mapped into the fuzzy hypercube of three dimensions such that each vertex represented each variable as either absent or maximally severe. Three cluster centers were obtained, and all clusters had moderately severe (0.6–0.7) vessel and coagulopathic conditions (n=162). Conclusions: Fuzzy clustering methods in the fuzzy hypercube allow for the representation of positive and negative synergy between variables currently excluded from conventional probability-based statistical analysis.
P20. Neuropsychiatric features of cluster headachesR. E. Jorge, J. L. Leston, R. G. Robinson (Department of Psychiatry, University of Iowa College of Medicine, Iowa City, IA)
Background: This is a case-control study of the prevalence of mood and anxiety disorders among patients with cluster headaches. Methods: We have compared a group of 21 patients with episodic cluster headaches (ECH) and a group of 21 patients with tension headaches (TH) carefully matched for age, sex, and educational level. Psychiatric diagnosis was made using a semistructured interview and DSM-IV criteria. Quantitative measures of depression and anxiety were obtained using the Ham-D and the Ham-A. In addition, all subjects received a neuropsychological evaluation that was designed to explore basic memory and executive functions. Results: Of the 21 patients with cluster headaches, 5 (23.8%) met DSM-IV criteria for an anxiety disorder during the year previous to the episode. Panic disorder was diagnosed in 2 patients (9.5%). The remaining 3 patients (14.3%) met criteria for generalized anxiety disorder. Of the 21 patients with tension headaches, 2 (9.5%) met diagnostic criteria for an adjustment disorder with a depressed mood and 1 (4.8%) met criteria for an adjustment disorder with mixed anxiety and depressed mood. Ham-A scores were significantly higher among patients with ECH (Kruskal-Wallis ANOVA, P=0.01). ECH patients also showed significantly lower Auditory Verbal Learning Test scores (Kruskal-Wallis ANOVA, P=0.004) Conclusions: When compared with a group of patients suffering tension headaches, ECH patients showed a higher frequency of anxiety disorders (panic disorder and generalized anxiety disorder) during the year preceding the onset of headaches and significantly greater Ham-A scores during the clinical episode. In addition, patients with ECH appeared to be selectively impaired in a verbal memory measure.
P21. Abstract withdrawn.
P22. Use of alternative medicines in neuropsychiatric disordersW. Curt LaFrance, Jr., James Duffy (Brown University, Providence, RI)
Background: Growing numbers of people throughout the United States are using various forms of alternative therapies. A 1993 report revealed that 34% of U.S. adults used at least one unconventional form of health care. With the population's increased awareness of and access to these alternative therapies, the number of patients using alternative interventions grows. It behooves the clinician to have a working knowledge of these supplemental therapies used frequently by their patients. Methods:medline literature search of journals from the past decade was performed to report the types and frequency of alternative therapies used. Special attention was given to the therapies used in neuropsychiatric disorders. Results: At least 40% of patients in the United States use alternative therapies for treatment of general symptoms. A summary chart and review of known mechanisms of action and interactions of the current pharmacologic and herbal treatments are given. The seven categories of alternative therapies are discussed also: mind-body interventions, bioelectromagnetic therapies, alternative systems of medical practice, manual healing methods, pharmacologic and biologic treatments, herbal medicines, and diet and nutrition. Conclusions: Increasing numbers of patients are using alternative medicines. Awareness of the therapies available will aid neuropsychiatrists in providing beneficial and safe care for their patients.
P23. Assessment of neuropsychiatric aspects of frontal lobe epilepsyLinda Mah, Ghislaine Savard, Frederick Andermann, François Dubeau, André Olivier (Montreal Neurological Hospital, McGill University, Montreal, Quebec, Canada)
Background: Frontal lobe seizures are frequently misdiagnosed as pseudoseizures due to their atypical presentation. “Frontal lobe” syndromes are associated with various neurological disorders and pose management difficulties (J Neuropsychiatry Clin Neurosci 1994; 6[3]). Neuropsychiatric assessment of frontal lobe function is not performed routinely in patients with frontal lobe epilepsy (Adv Neurol 1995; 66). We believe neuropsychiatric assessment of frontal lobe function contributes to the diagnosis and management of patients with frontal lobe epilepsy. We report 3 illustrative cases. Methods and Results (case reports): All 3 patients had intractable right frontal lobe epilepsy. The diagnosis of pseudoseizures had been considered in 2 patients. 1 patient had an “apathetic” frontal lobe syndrome and subsequently developed akinetic mutism following a complication of intra-electrode implantation. Another had a “disinhibited” type with improvement in social behavior following epilepsy surgery. The third presented with subtle deficits in interpersonal judgment despite preserved function on standard neuropsychological testing. Conclusions: Neuropsychiatric assessment of frontal lobe dysfunction in patients with frontal lobe epilepsy provides additional diagnostic information and guides management of these patients through identification of problematic “frontal lobe” behaviors.
P24. HIV-related manic syndromes: prevalence and risk factorsLinda Mah, Pascale DesRosiers (McGill University, Montreal, Quebec, Canada)
Background: Several cases of mania associated with HIV disease have been reported in the literature, but few systematic studies exist. The authors conducted a retrospective chart review to determine the frequency of HIV mania and its possible risk factors. Methods: All charts of patients with HIV seropositivity referred for psychiatric consultation at a large urban teaching hospital from 1990 through 1996 were reviewed to identify cases of mania. Patients were grouped based on the presence of personal or family history of mood disorder and were compared on a number of clinical variables. Results: 11 patients were identified: 8 with negative personal/family histories of mood disorder and 3 with prior diagnoses of bipolar affective disorder. Patients with no history of mood disorder, compared with the bipolar group, were more likely to have AIDS, low CD4+ counts, low hemoglobin, dementia, and cortical atrophy. The prevalence of HIV mania was 2.1%. The median survival time following onset of HIV mania was 6 months. Conclusions: Mania in patients with HIV seropositivity is associated with endstage disease, cognitive impairment, and low hemoglobin. We hypothesize that HIV mania is mediated by direct insult to frontal-subcortical pathways that play a role in regulating mood and cognition.
P25. Anergia after right insular strokeFacundo F. Manes, Sergio Paradiso, Robert G. Robinson (Department of Psychiatry, University of Iowa College of Medicine, Iowa City, IA)
Background: The insula is a major component of the limbic brain (Yakovlev, J Neuropathol Exp Neurol 1959; 18:22–55). The behavioral implications of insular damage, however, remain to be elucidated. We compared the neuropsychiatric profiles of patients with right and left insular damage. Methods: Subjects were 6 patients with left insular stroke and 7 patients with right insular stroke as evidenced by MRI scans. Patient groups had comparable race, age, education, and sex. Patients were included who had lesions involving the insular cortex and no more than a small portion of adjacent white matter. Between 4 and 8 weeks following acute stroke, patients were administered a neuropsychiatric battery including the Ham-D, Ham-A, Zung Depression Scale, modified Present State Examination (PSE), MMSE, Johns Hopkins Functioning Inventory (JHFI), Social Functioning Exam (SFE), and Social Ties Checklist (STC). Results: Patients with right and left damage showed comparable depression, anxiety, cognitive function, functional disability, and social functioning scores. 5 (71%) right insular lesion patients reported symptoms of anergia and underactivity compared with 1 (16%) patient with left insular damage (Pearson χ2=3.90, df=1, P<0.05). Similarly, 6 (85%) right lesion patients reported moderate to severe tiredness compared with 1 (16%) left lesion patient (two-tailed Fisher's exact test, P=0.006). No other difference on psychiatric symptoms was found to be significant. Conclusions: Symptoms of impaired level of energy were associated with right insular damage. Insular cortex has reciprocal connections with the frontal lobe (Agustine, Brain Res Brain Res Rev 1996; 22:229–244). Frontal lobe has been shown to regulate willed action (Frith et al., Proc R Soc Lond 1991; 244:241–246). Right insular damage may disrupt the frontal circuit involved in willed action and lead to anergia.
P26. Adults with profound mental retardation (PMR), severe destructive behaviors (SDB), and ventricular enlargement (VE) respond preferentially to neuroleptic medicationDavid James, Leonard Buscemi, Philip May (Hunterdon Developmental Center/Robert Wood Johnson Medical School, Clinton, NJ)
Background: We have previously reported a correlation between severe, uncontrollable destructive behaviors and ventricular enlargement in adults with profound mental retardation (J Neuropsychiatry Clin Neurosci 1995; 7:405–406). Furthermore, we suggested that destructive behaviors in association with ventricular enlargement may represent loss of frontal cortical-subcortical circuits needed for impulse control in adults with PMR. We felt it would be important to evaluate the behavioral response to different psychoactive medications in adults with PMR and to correlate their responses with ventricular size. Methods: 25 adults with PMR and SDB were evaluated for efficacy of neuroleptics plus at least one other class of psychoactive medication. Ventricular-cerebral ratio (VCR) was determined in all patients as previously described. The patients were divided into two groups: group 1, no response to neuroleptics (n=9); group 2, good response to neuroleptics (n=16). Results: Mean VCRs were as follows: group 1, 132; group 2, 210 (P=0.0011, Student's t-test). Conclusions: Ventricular enlargement in adults with PMR and SDB may be predictive of a preferentially good clinical response to neuroleptic medication, as compared with other classes of psychoactive medications. Support from New Jersey Department of Human Services, Division of Developmental Disabilities.
P27. Personality disorders among medically refractory epileptic patientsFaustino Lopez-Rodriguez, Mario F. Mendez, Lori Altshuler, Joanne Kay, Sandra Delarhim, Jerome Engel (University of California, Los Angeles, CA)
Background: Patients with epilepsy have more psychopathology than those without a seizure disorder. Most investigations of psychopathology among epileptic patients have focused on psychosis, depression, and specific personality characteristics. Methods: We investigated the frequency and nature of personality disorders among 52 medically refractory epilepsy patients referred for epilepsy surgery assessment. The majority of patients had clearly localized partial complex seizures of temporal limbic origin. The patients underwent the Structured Clinical Interview for DSM-III. Results: Among these patients, 11 (21%) were diagnosed with a personality disorder. There was no patient with a diagnosis of Cluster A personality disorder; Cluster B was present in 5.8%; and Cluster C was present in 15.4%. Dependent and avoidant personality disorders were disproportionately represented. Moreover, the presence of an epileptic aura strongly predicted the presence of personality disorder. Conclusions: We conclude that at least among severe epileptics, Cluster C symptoms are common and the presence of epileptic auras may predispose to personality changes.
P28. Treatment of organic emotionalism with selective serotonin reuptake inhibitorsUlrich Müller, Toshiya Murai, Thomas Bauer-Wittmund, D. Yves von Cramon (Department of Neurology, Max Planck Institute of Cognitive Neuroscience, Leipzig, Germany)
Background: SSRIs are the treatment of choice for organic emotionalism independent of accompanying depression (Andersen, Drugs Aging 1995; 6:105–111). In a series of 26 consecutive patients with acquired brain damage and episodes of involuntary crying, the efficacy and tolerability of paroxetine and citalopram were compared. Methods: The degree of emotionalism was rated as severe (3), moderate (2), mild (1), or absent (0) based on clinical interviews with symptom provocation. The first 13 patients (6 female, mean age 53.2±9.0 years, mean time since lesion 10.6±10.3 months) were treated with paroxetine, and another 13 patients (5 female, mean age 51.8±11.8, mean time since lesion 19.9±16.9) received citalopram in single daily doses of 10 or 20 mg. Most patients suffered from stroke (11 M/11 F), others from hypoxia (2 M/0 F) or traumatic brain injury (0 M/2 F). Results: We observed rapid onset (within 1 to 3 days) and highly significant (P<0.001) improvements of emotionalism after both paroxetine (2.4±0.5 to 0.4±0.4) and citalopram (2.1±0.3 to 0.2±0.4). There were no efficacy differences despite higher chronicity in the citalopram group. The only side effect after paroxetine was nausea, which was reversible, in 2 patients and nausea with vomiting in another 2 patients, who were switched to citalopram. Citalopram was tolerated without side effects. Conclusions: This open study shows that low doses of both SSRIs are equally effective to treat organic emotionalism. Our finding of more frequent side effects with paroxetine will require further investigation in a controlled study.
P29. Treatment of parasomnia with donepezilJohn M. Ringman, Jeffrey L. Cummings (Department of Neurology, University of Los Angeles, CA)
Background: REM sleep behavior disorder (RSBD) is a parasomnia characterized by loss of the atonia normally accompanying rapid eye movement (REM) sleep and by associated behaviors often of a violent nature. Human and animal studies indicate pathology in the brainstem cholinergic pedunculopontine nucleus as etiological. The condition in humans occurs in association with structural lesions of the brainstem and with neurodegenerative conditions. Methods (case report): A case of a 72-year-old man with a parasomnia consistent with RSBD is reported. After presenting with visual loss at age 53 he was diagnosed with a suprasellar craniopharyngioma, which was resected. Postoperatively the patient developed a sleep disorder characterized by somniloquy and threatening dreams of such things as cars driving toward him, culminating with the patient jumping out of bed. These were not treated and were unchanged until age 68, when he began to experience symptoms consistent with Alzheimer's disease and donepezil treatment was initiated. Results: On 10 mg of donepezil, the patient experienced a dramatic decrease in abnormal nocturnal behavior. Conclusions: Enhancement of cholinergic function in this patient had an ameliorative effect on his sleep disorder, possibly secondary to improvement of function in a damaged brainstem cholinergic system.Support from a grant by NIA.
P30. HIV-associated psychomotor slowing improves with combination antiretroviral therapyNed Sacktor, Richard Skolasky, Robert Lyles, Glen McFarlane, Deborah Anderson, Eric N. Miller, Ola Selnes, James Becker, Jerry Wesch, Justin McArthur (Johns Hopkins University, Baltimore, MD)
Background: The impact of combination therapy including a protease inhibitor (combo+PI) on HIV-associated psychomotor slowing is unclear. The objective of this study was to determine if psychomotor speed, a sensitive index of HIV dementia, improves with combo+PI compared with other antiretroviral treatments. Methods: 411 HIV-seropositive homosexual men in the Multicenter AIDS Cohort Study were studied from October 1995 to September 1997. Participants were classified into four treatment groups: antiretroviral-naive, monotherapy, combination therapy without protease inhibitors (combo-noPI), and combo+PI. We compared longitudinal performance on tests of psychomotor speed, the Grooved Pegboard (GP) test (nondominant and dominant hands), Trail Making Test part B, and Symbol Digit Modalities Test (SDMT). Results: Relative to antiretroviral-naive and monotherapy participants, combo+PI participants with abnormal baseline neuropsychological testing had better GP nondominant hand (P=0.02) and SDMT (P=0.03) performance. Combo-noPI participants also showed better SDMT performance (P=0.01). Conclusions: Combination therapies with and without protease inhibitors are associated with improved psychomotor speed performance in HIV-seropositive homosexual men with abnormal neuropsychological testing. Further studies are needed to determine the durability of this effect and whether it is associated with functional improvement in HIV dementia patients.Support from NIAID Grant AI35042, NCRR Grant RR00722, and NINDS Grant NS26643.
P31. Treating tardive dyskinesia with ondansetron Pinkhas Sirota (Y. Abarbanel MHC, BatYam, Israel)
Background: Tardive dyskinesia (TD) is a well-known syndrome that includes uncoordinated, involuntary, and abnormal choreoathetotic movements of the head, limbs, and body muscles. All of the old dopamine receptor antagonists have been known to cause TD. About 20% of the patients treated with dopamine antagonist for more than l year developed tardive dyskinesia. TD is probably the result of hypersensitivity of the dopamine receptors in the basal ganglia as a consequence of chronic blockade of the dopamine receptors by antipsychotic drugs. No satisfactory treatment of this disorder is available. We have examined a new treatment for TD, using ondansetron (Zofran) as a serotonin 5-HT3 antagonist. Ondansetron does not cause any extrapyramidal or endocrinologic impairments, which supports the claim that the medication does not block the dopamine receptors. The present study was designed to evaluate the safety and efficiency of ondansetron in the treatment of TD. Methods: The experimental group consisted of 10 inpatients: 7 females and 3 males, ages 42–81 years (mean±SD: 69±10.1). These 10 patients suffered from schizophrenia (DSM-IV). The duration of TD was 3 to 45 years. The clinical evaluation of TD was carried out by using the Abnormal Involuntary Movement Scale (AIMS) and ST.HANS scale. All the patients were treated with 4–8 mg/day of ondansetron for 4 weeks. The evaluation was performed three more times: at baseline, after 2 weeks, and after 4 weeks on the AIMS, ST.HANS, and Clinical Global Impression and was recorded on videotape. Laboratory examinations were also performed at these intervals. Results: A statistically significant improvement of TD was noted in these patients after 4 weeks of treatment. It paralleled the clinical improvement. Male patients had a significant improvement compared with female patients. There were no hematological or chemical laboratory impairments before or after the treatment with ondansetron. Conclusions: The treatment with ondansetron resulted in a marked decrease in TD symptoms. Our results indicate that ondansetron treatment may be effective for chronic schizophrenic patients in reducing TD symptoms and controlling aggressive behavior and anxiety. Further research is needed to determine whether or not this drug is effective in TD.
P32. Abstract withdrawn.
P33. Role of depression severity and treatment in cognitive functioning in elderly subjects with CNS diseaseRobert van Reekum, Diana Clarke, Martine Simard, David Conn (Baycrest Centre and University of Toronto, Toronto, Ontario, Canada)
Background: Although depression is believed to affect cognition in CNS disease, this conclusion is based primarily on data from stroke populations. Additionally, there is little evidence describing the relationship between cognition and the severity and treatment of depression in CNS disease. Methods: Baycrest Centre offers a day hospital for depression, where data including the Ham-D and measures of cognition are routinely collected. 112 subjects with a variety of CNS diseases have been treated; data were available for 80. Results: A logistic regression analysis using Mattis Dementia Rating Scale (MDRS) score (greater or less than cutoff for dementia) as dependent variable showed that only the Ham-D score predicted MDRS status (R=–0.16, P=0.03). Age, education, gender, and age at onset of depression did not enter the model. MMSE scores (mean±SD) for the group were 25.4±3.9 at admission and 26.1±3.1 (P<0.001) at discharge. These results are compared with results from the non-CNS-disease day-hospital attenders, in which Ham-D score did not enter a similar model (van Reekum et al., Am J Geriatr Psychiatry, in press). Conclusions: The severity of depression is a predictor of cognition in CNS disease generally, and treatment of depression causes only modest cognitive improvement.
P34. Investigation and related factor analysis of the level of IL-2 secreted by peripheral blood lymphocytes in acute cerebral vascular disorder (CVD) patientsQ. C. Zhang, C. H. Chen, S. R. Gao (Second People's Hospital, Shantou City, Guangdong Province, People's Republic of China)
Background: The findings in recent years on the neuropsycho-endocrino-immunology network perhaps will have some implications for neuroscientists seeking the causes and the treatments of neuropsychiatric disorders. CVD, as the most common cerebral disorders, will give rise to disturbances of patients' homeostasis. Interleukin-2 (IL-2) is the key lymphokin and plays important roles both in body liquid and cell immunology. Methods: All entering patients should meet the requirements of having clearly CT-proved diagnosis and no immune disorders and/or use of drugs such as steroids. The MTT (3-[4,5-dimethylthiazolzyl]-2,5-diphenyl tetrazodium bromide) method was used to determine the level of IL-2. Results: 29 acute CVD patients' lymphocytes were sampled along with those of 23 normal control subjects. The results showed that IL-2 levels of the acute CVD patients were significantly lower than those of control subjects (0.02<P<0.05). The correlated factors were longer period of disturbance of consciousness, left- or two-hemisphere lesion location, and the emotional disorders of the CVD patients. The suppression of the IL-2 level of the patients with complicated infections tended to be more obvious. Additionally, the IL-2 levels of 6 patients were reexamined; 3 of them suffered from infections. Conclusions: The level of IL-2 secretion was significantly suppressed. Results suggest that there may be some internal associations among hemispheric laterality, emotion, and immune function. The authors propose that it might be useful to apply immunostimulants for improvement of immune function, while applying antidepressants for depression after stroke, in order to improve the outcome of CVD patients.
P35. Investigation of poststroke emotional disorders and analysis of their related factorsQ. C. Zhang, C. H. Chen, S. R. Gao (Second People's Hospital, Shantou City, Guangdong Province, People's Republic of China)
Background: Cerebral vascular disorders (CVD), as brain diseases, can not only result in physical deficits, but also give rise to a variety of mental disorders for patients. These mental disorders have impacts on the prognosis of the sufferers directly or indirectly, so it may be important to investigate the occurrence rates and related factors of poststroke emotional disorders. Methods: The cutoff points of emotional scales (Ham-D and Ham-A) were used as the mental symptoms diagnostic methods. Several other scales were used to assess patients' neurological function, past and associated physical diseases, intelligence level, activities of daily living (ADL), quality of life, and self-perceived social support. Several CT parameters were also recorded. The investigation was done at two time points: acute stage and 3 months later. Single and multiple factors analyses were conducted. Results: 121 consecutive CVD patients were examined. 32 cases (26.4%) were diagnosed as having poststroke depression and 48 as having poststroke anxiety disorders. 3 months after, the remaining number of patients was 118 (3 died), the number of cases with depressive disorder was 26 (22.1%), and the number with anxiety disorder was 31 (26.3%). At both time points the production of depression and anxiety were related to marked ADL impairment, severe neurological deficits, poor quality of life, dementia (assessed by MMSE), not enough social support, left anterior and/or cortical lesion location, and large lesion volume. Conclusions: Poststroke emotional disorders are very common mental complications of CVD patients. Although the causes of poststroke emotional disorders may be characterized with a biopsychosocial model, brain damage itself perhaps is essential.
P36. Schizophrenia-like syndrome after stroke, with 17 case reportsQ. C. Zhang, C. H. Chen, S. R. Gao (Second People's Hospital, Shantou City, Guangdong Province, People's Republic of China)
Background: The psychotic syndrome after stroke is a relatively rare mental complication of stroke, and its etiologies and its meaning for functional psychosis are rarely studied. Methods: The CCMD-2-R (Chinese Classification and Diagnostic Criteria of Mental Disorders, 2nd edition, revised) were adopted as the diagnostic criteria for the psychotic syndrome. CT examination was done for all the stroke patients. Results: 17 cases were diagnosed among the 118 consecutive-admission stroke patients (13 male, 4 female; 9 left lesion location, 5 right, 3 both; 12 infarction, 5 hemorrhage). 6 of 9 with left lesion location were complicated with both schizophrenia-like and emotional symptoms, and all were self-critical of the contents of their delusions. At follow-up, their symptoms had lessened or disappeared. But patients with right lesion location were often evidently paranoid, and their psychotic symptoms were persistent at follow-up. Compared with the CVD patients without the syndrome, the study group had larger lesion volume. Conclusions: The onset of the schizophrenia syndrome was related to the global decline of brain function, and the laterality was responsible for the different symptoms of the patients with different hemisphere lesion locations observed.
P37. Poststroke mania-like syndrome, with 6 case reportsQ. C. Zhang, C. H. Chen, S. R. Gao (Second People's Hospital, Shantou City, Guangdong Province, People's Republic of China)
Background: The poststroke mania-like syndrome is a very rare complication of stroke. 6 patients were reported and the etiologies were analyzed. Methods: The CCMD-2-R (Chinese Classification and Diagnostic Criteria of Mental Disorders, 2nd edition, revised) was adopted for this study. Patients with personal and/or family psychiatric history were excluded. Results: 6 cases were diagnosed among the 118 consecutive-admission stroke patients (3 male, 3 female; mean age 55.1 yr; 4 cerebral hemorrhage, 2 cerebral infarction; 1 left lesion location, 5 right lesion location). All of the 6 cases are acute onset, and the time period is more than 2 weeks. The displayed characteristics are mania-like, including excitement, talkativeness with a certain degree of attractiveness, the feeling of speedy thinking, increased appetite and sexual drive, and absent or decreased self-insight and less treatment compliance. 3 months later all the symptoms had disappeared except that 2 patients remained talkative. Conclusions: Personality traits and right hemispheric lesion location are the two major contributing factors to the syndrome. This perhaps reflects the different roles the two hemispheres play in the production of emotion.
P38. Psychosomatic disturbances of cerebral vascular disease (CVD) patients' major caregiversQ. C. Zhang, C. H. Chen, S. R. Gao (Second People's Hospital, Shantou City, Guangdong Province, People's Republic of China)
Background: CVD is not only a devastating disorder for the victims, but it also has severe impact on the psychosomatic status of their family members, especially the major caregivers. In turn, the caregivers' psychosomatic status will potentially interact with CVD patients' rehabilitation. Methods: The major caregiver is defined as the main relative who lives with and is responsible for the daily activity and medical-related issues of the patients. The standard scales and questionnaires were used to assess the psychosomatic status of patients and their caregivers. Single and multiple factor analyses were conducted. Results: The psychosomatic status of 108 patients with a 3-month history of CVD and their caregivers were investigated. 28 (25.9%) of the caregivers reported that their health was affected as a result of looking after the patient. 27 (25.0%) of them suffered from depressive disturbances, and 15 (13.9%) had anxiety symptoms. Both were associated with sleep disturbance (87.0%), worrying about patients having accidents (84.2%), and feelings of incompetence (79.6%). Multiple regression analysis revealed that those who took care of patients with emotional disorders and received poor social support were more vulnerable to emotional problems, too. Conclusions: Psychosomatic problems were very common among the caregivers. It is recommended that psychological counseling and social support be given to CVD patients' caregivers.
P39. Atypical antipsychotics in frontotemporal dementia (FTD): a pilot studyLeonardo F. Caixeta, Ricardo Nitrini (University of São Paulo School of Medicine, São Paulo, Brazil)
Background: Atypical antipsychotics (clozapine and risperidone) have provided good results in hypofrontality-related symptoms of schizophrenia (negative symptoms), and these effects are related hypothetically with dopamine D4 receptor affinities at the prefrontal cortex. Frontotemporal dementia is characterized by behavioral symptoms, many of them resembling schizophrenic symptoms (apathy, social withdrawal, poor insight and abstraction, perseveration, stereotypy, concreteness of language, poor performance on executive functions). Methods: 10 patients were administered risperidone (0.5 to 6 mg/day) and 2 clozapine (up to 250 mg/day) for at least 6 months. All were diagnosed as having FTD (Lund and Manchester criteria) and evaluated clinically and with the Frontal Behavior Inventory (Kertesz et al., Can J Neurol Sci 1997; 24:29–36) before and after 4 months of treatment. Results: All patients showed some benefit from using the medication, mainly improvement of positive symptoms (agitation, logorrhea, wandering, aggression). Negative symptoms apparently did not change, but with the reduction of some positive symptoms (such as agitation, aggression) social adequacy and inattention improved a little. The main side effect in these patients was sedation, sometimes even at low doses. Extrapyramidal side effects were observed in only 5 patients (1 of whom had presented these symptoms before beginning the medication) and usually in doses greater than 2 mg/day. Conclusions: Atypical antipsychotics may represent a safe option to treat positive symptoms of FTD because of their low potential for extrapyramidal side effects (a great advantage for those patients who are susceptible to these effects) when compared with classic antipsychotics. Negative symptoms, however, may not improve with their use or may improve only a little as a consequence of their effect on positive symptoms.
Dementia and Aging
P40. Aspects of the evolution of frontotemporal dementia: a clinical and neuroimaging studyLeonardo F. Caixeta, Ricardo Nitrini, Adriana De Simone, Carlos Buchpiguel (University of São Paulo School of Medicine, São Paulo, Brazil)
Background: Frontotemporal dementia (FTD) has a progressive, deteriorating course, in which some symptoms are ephemeral, and can suffer modifications in its phenomenology. Different symptoms appear to occur at different stages of the evolution, some appearing in the early, others in the middle or final phases of the condition. Methods: 5 patients with FTD (Lund and Manchester criteria) were evaluated cognitively (neuropsychologically and with the MMSE), with behavioral assessment (descriptive psychopathology and Lhermitte's protocol for utilization and imitation behavior), and with neuroimaging methods (SPECT and MRI and/or CT) in two different moments of their evolution (t1 and t2)—t1 referring to the beginning of the evaluation and t2 to important modifications in the clinical picture of these patients (e.g., when a previously disinhibited case becomes predominantly apathetic). Results: 4 patients evolved from a previous disinhibited behavior (t1) to a predominantly apathetic one with intensification of repetitive behavior (t2). Neuroimaging in t2 showed enlargement of atrophy and frontotemporal hypoperfusion with some extension to anterior parietal regions when compared with t1. One patient evolved from apathy to disinhibition after ECT, but frontal hypoperfusion observed in t1 continued in t2. In the neuropsychological evaluation, all patients showed worsening from t1 to t2, except for 1 who improved in memory but not executive function. Intensification of repetitive behavior was correlated with some degree of basal ganglia atrophy in t2. Progressive anterior cingulate atrophy was observed in some cases. Conclusions: The cognitive decline and the switch from disinhibited to apathetic clinical pictures is gradual and is usually followed by intensification of the frontotemporal atrophy (as a consequence of neuronal loss in these regions). Evolutional clinical and neuroimage correlation studies are important in the generation of physiopathological hypotheses based on the relation of the beginning (or disappearance) of symptoms with the functional and anatomical brain modifications.
P41. Positron emission tomography study of priming in normal elderly subjectsK. E. Anderson, L. Cooper, N. Zubin, N. Szerlip, A. Di Mauro, A. Park, Y. Stern (Columbia University, New York State Psychiatric Institute, New York, NY)
Background: Priming (improvement of performance following prior exposure) is generally preserved in normal aging. It is unclear whether priming is stable over time in the elderly, as it is in young subjects. To address this question, we studied nonverbal priming immediately and at delay. Methods: 5 cognitively intact elderly subjects (mean age=74 yr) participated. Subjects indicated whether objects were possible or impossible in three-dimensional space during H215O PET scans. PET data were analyzed by using statistical parametric mapping. Results: During immediate decisions about previously seen possible objects, all subjects demonstrated a significant priming effect (14.6% improvement in identification of previously seen objects compared with novel objects). Subjects showed a trend toward significant activation of the left precuneus during priming, with bilateral deactivation of the fusiform gyri. At 1-hour delay, subjects did not show significant priming and did not activate the precuneus. Conclusions: These data suggest that priming is not preserved in elders over delay. Activation of the precuneus occurred only during initial priming and may indicate analysis of spatial information during nonverbal priming. Fusiform deactivation differs from results seen in young subjects on this task and could reflect processing differences in elderly subjects. Deactivation of this area may partially explain why nonverbal priming does not remain intact over time in these elders.Support from the Dana Foundation and NIA Grant AG14671.
P42. Changes in electrical activity in the human brain: quantitative EEG after a single dose of a nootropic drug, aniracetam, in healthy volunteersAlejandro G. Andersson, Carlos Hoffman, Miguel A. Miranda, Marisa Kalemkarian, Gabriela Dognibene, María del Carmen Garcia (Instituto de Neurologia, Buenos Aires, Argentina)
Background: We analyzed the effects on EEG power spectra after a single dose of aniracetam, a cognitive-enhancing substance, in healthy volunteers. Methods: 30 healthy volunteers free of medication and without a history of clinical or neurological problems, ages between 25 and 49 years, 16 women and 14 men, participated in the study. The first recording session was free of drug, with 23 grass gold cup electrodes applied to the scalp with the International 10-20 System. At the end of the first recording session, volunteers received placebo, 375 mg aniracetam, or 1,500 mg aniracetam in orange juice. The second recording session, postmedication, was 180 minutes later. We used Akonic Bio-Pc hardware and software. A 21-channel EEG was monitored continuously on screen. Monopolar EEG was recorded with biauricular reference. A single dose of aniracetam—a nootropic medication especially used for long-term treatment of cognitive impairment in aged patients—influenced the functional state of the brain of healthy volunteers in a dose-dependent manner as measured with qEEG. Results: We found an association with an increase of alpha relative power after a single dose of aniracetam. Changes were significant with 1,500 mg of aniracetam (ANOVA: P=0.026) but nonsignificant with 375 mg (P=0.97) and with placebo (P=0.99).Support from Laboratorio Rontag.
P43. Changes in human brain electrical activity: quantitative EEG after a single dose of a nootropic drug, aniracetam, in patients with cognitive deteriorationAlejandro G. Andersson, Carlos Hoffman, Miguel A. Miranda, Marisa Kalemkarian, Gabriela Dognibene, María del Carmen Garcia (Instituto de Neurologia, Buenos Aires, Argentina)
Background: We analyzed the effects on EEG power spectra after a single dose of aniracetam in patients with cognitive deterioration. Methods: We used Akonic-Bio-Pc hardware and software. A 21-channel EEG was monitored continuously on screen. Monopolar EEG was recorded with biauricular reference. 27 patients with cognitive deterioration, between 45 and 70 years old, 10 men and 17 women, participated in the study. We used the Global Deterioration Scale (GDS) to classify them. We had 9 patients with GDS scores of 2 or 3; 9 with GDS of 4 or 5; and 9 with GDS of 6 or 7. The first recording session was free of drug, with 23 grass gold cup electrodes applied to the scalp with the International 10-20 System. At the end of the first recording session, patients received 1,500 mg aniracetam. The second recording session, postmedication, was 180 minutes later. Results: We found an association between the dose of 1,500 mg of aniracetam and increase of alpha power. This was more important in mild deterioration (GDS 2 and 3: Z=0.0014) and in moderate deterioration (GDS 4 and 5: Z=0.00065), and nonsignificant in severe deterioration (GDS 6 or 7: Z=0.10).Support from Laboratorio Rontag.
P44. Reliability of four clinical diagnostic criteria for the diagnosis of neurodegenerative dementiasKaryn E. Catt, Oscar L. Lopez, Irene Litvan, James T. Becker, Robert Stowe, William Klunk, Daniel I. Kaufer, Steven T. DeKosky (Pittsburgh, PA)
Background: Although reliability of the clinical diagnosis of Alzheimer's disease has been established, there are no reliability studies for the recently developed criteria for progressive supranuclear palsy (PSP) and frontotemporal lobe dementia (FTD). Furthermore, there have been no studies of diagnostic reliability using such criteria in a mixed sample of patients with neurodegenerative processes. Methods: Four experienced clinicians reviewed clinical data abstracted from the records of 42 pathologically diagnosed demented subjects. They were asked to apply the NINDS-SPSP (Society for Progressive Supranuclear Palsy) clinical criteria for PSP, the Lund-Manchester criteria for FTD, the NINCDS-ADRDA criteria for AD, and the Consensus Guidelines for Dementia With Lewy Bodies (DLB). Results: The interrater agreement for AD ranged from 0.58 to 0.90 (generalized kappa=0.75); for PSP, from 0.59 to 0.80 (generalized kappa=0.70); for FTD, from 0.54 to 0.91 (generalized kappa=0.74); and for DLB, from 0.06 to 0.72 (generalized kappa=0.34). The kappa pool test showed a statistically significant difference between DLB and the other dementias, and no differences were observed among AD, FTD, and PSP. Conclusions: This study shows an increased reliability for dementia among clinicians compared with earlier studies, especially for AD. Similarly, there was a substantial interrater agreement on the most recently developed clinical criteria for the less frequent forms of dementia (e.g., PSP, FTD). However, reliability for dementia is still not perfect, even among experienced clinicians. Heterogeneity of the clinical presentation of DLB significantly affected interrater agreement.Support from Alzheimer's Disease Research Center Grant AG05133.
P45. Prediction of cognitive decline in individuals with cognitive loss, no dementiaBarbara J. Collins, Katharina Schulze (Ottawa Hospital, Ottawa, Ontario, Canada)
Background: Most individuals experience some decline in cognitive function as they age. In most cases, these cognitive changes have a relatively slow, benign course, but in a minority they are the harbingers of progressive dementia. We sought to identify clinical features that might predict the evolution of age-associated cognitive deficits. Methods: Subjects were 46 individuals assessed in a memory clinic and diagnosed with cognitive loss but no dementia (19 males, 27 females; mean age 68.7 yr, SD=8.59). Cognitive functioning of all subjects was assessed at intake and after an average interval of 479±285 days and was indexed at each time point by combining scores on an extended MMSE and the Dementia Rating Scale (DRS). Annual change in mental status was computed as the difference between the two mental status indexes, divided by delay and multiplied by 365. Age at initial assessment, a composite measure of language functioning (composed of initial scores on the language section of the MMSE, measures of semantic and letter fluency, and a brief test of confrontation naming), and family history of dementia were examined for their ability to predict mental status change, since these factors have all been found to have prognostic value in progressive dementia. Results: There was little change in the average mental status index from intake (160/184) to reassessment (157/184). However, there was considerable variability in the change index (SD=10.83), with scores ranging from a gain of 21 points to a loss of 41 points. Both age (r=0.42, P=0.002) and language (r=0.39, P=0.005) correlated significantly with mental status change. Family history of dementia was not correlated with cognitive decline (r=0.08, P=0.32), but this information was not available for all subjects. Both age and aphasia entered a stepwise regression analysis, and the final regression equation was highly significant (multiple R=0.61, P<0.0001). Conclusions: Older age at onset and aphasic symptoms independently predict decline in mental status among nondemented individuals with cognitive problems.
P46. Clinical features of very early onset (ages 27–35) familial Alzheimer's diseaseGayatri Devi, Alexandra Fotiou, Adria Gonzalez, Vincent Santana, Darlene Jyrinji (Columbia University, New York, NY)
Background: Alzheimer's disease with age at onset in the 20s has been reported in 2 families, linked to mutations of the presenilin-1 gene and characterized by an aggressive course with death in 5 years. Methods: We followed the atypical clinical course of AD in a family with both early- and late-onset AD. Results: The proband, his father, and his brother are affected; there is an unaffected brother, age 27. The proband's paternal and maternal grandmothers both have late-onset AD (onset in late 70s). The proband developed mood swings at age 29 and was demented by 31. He was aphasic by 35, developed myoclonus progressing to generalized tonic-clonic seizures, and is now institutionalized at age 36. His father had mood swings at age 35 to 36, followed by memory loss and myoclonus leading to institutionalization at 39. He was mute and not ambulatory by age 40, lost his ability to swallow by 50, and died at 60, with an autopsy confirming AD. The proband's younger brother had mood swings at age 27 and by age 29 had memory difficulties. Myoclonus began by 30, and at 32 he is globally aphasic but able to ambulate. Conclusions: The course of AD in this early-onset family is unusual in the course to death of over 25 years in the father and both sons now being 5 to 7 years into the course of the illness. The AD in this family may be due to 1) modification of a presenilin-1 mutation by another gene and/or environmental factors or 2) mutation on other gene(s) as yet unidentified.Support from NIA Grants AG07232, AG10963, and AG08702.
P47. CADASIL: neurobehavioral features in a confirmed caseChristopher M. Filley, Laetitia L. Thompson, Chun-I Sze, Jack A. Simon, James A. Paskavitz, Bette K. Kleinschmidt-DeMasters (University of Colorado School of Medicine, Denver, CO)
Background: Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is a recognized form of vascular dementia, but neurobehavioral features of the disease have not been fully described. Methods: We studied a 62-year-old right-handed man with dementia and leukodystrophy on magnetic resonance imaging. Clinical evaluation, neuropsychological testing, brain and skin biopsy, and genetic analysis were performed. Results: Personality change, psychosis, and mood disorder preceded dementia, which was only evident 20 years after disease onset. The etiology of these syndromes was unknown for most of the clinical course. The dementia was characterized neuropsychologically by cognitive slowing, inattention, impaired learning with intact recognition, and perseveration, a pattern of deficits consistent with subcortical white matter involvement. The diagnosis of CADASIL was confirmed by electron microscopy of the skin biopsy showing granular osmiophilic material, and by a characteristic gene mutation on chromosome 19q12. Conclusions: The clinical presentation of CADASIL may involve a variety of neuropsychiatric syndromes that precede dementia by many years. When the dementia occurs, a subcortical pattern of neuropsychological impairment reflecting involvement of cerebral white matter can be detected.
P48. Validation of SyndromKurztest (SKT): a brief and efficient neuropsychological test for the diagnosis of dementiaLuis Fornazzari, Francisco Cumsille, Renate Flaskamp, Pilar Quiroga (Toronto, Ontario, Canada)
Background: Our aim was validation and harmonization of SKT, a test designed for the investigation of acute and chronic cognitive impairment—particularly naming, praxis, immediate recall, recent memory, and attention—in a brief format of nine subtests. The results are expressed in rough or normative data based on 10,000 evaluations done in Germany. Methods: From an urban population of 2,500 Chileans previously evaluated in the WHO Age-Associated Dementia Project, a stratified subsample of 168 was selected for the present study. The mean age of the subsample was 77.5 years (range 64–97), 63% were women, and 80 had a diagnosis of dementia (28 mild, 30 moderate, 20 severe). We also selected 90 normal, matched control subjects. Of the sample, 44% were illiterate. Diagnosis was defined by ICD-10, MMSE, and the Functional Assessment of Pffefer. The investigators were unaware of the diagnosis of the subjects. Results (Table 1): Significant differences were found between normal and demented subjects in both SKT and MMSE scores. Highly significant results were obtained for each of the nine subtests (P>0.0000001) between the three groups (normal, mild-moderate, and severe dementia). There was no influence of schooling on the scores. Age was significantly related to SKT scores. Conclusions: In our sample, SKT was useful for the diagnosis of dementia and correlated well with MMSE. The scores were independent of literacy but significantly correlated with age. The test may discriminate mild-moderate dementia from severe dementia.Support from Bayer of Chile.
P49. Slow Creutzfeldt-Jakob disease (CJD) with negative 14-3-3 proteinDean J. Foti, Olinka Hrebicek, Christopher R. Honey (University of British Columbia, Vancouver, BC, Canada)
Background: The slow variants of CJD previously reported are usually associated with prominent cerebellar signs, a long prodrome of neuropsychiatric changes, or a prolonged advanced nonfunctional state. The 14-3-3 protein isolated from CSF has been reported to have high sensitivity for typical CJD but has not been evaluated in atypical cases with slower progression. The 14-3-3 protein has been falsely positive with recent stroke. Methods: Case report with neuropathological confirmation. Literature review. Results: A 72-year-old woman presented with rapidly progressive cognitive decline with frontal-subcortical dysfunction and prominent right hemisphere hypoperfusion on SPECT imaging. She remained clinically stable with moderate dementia over a period of 6 months, with little functional progression. She remains ambulatory 18 months after symptom onset and continues to live at home. Cortical biopsy confirmed a spongiform encephalopathy. EEG was negative for periodicity, and minimal myoclonus was present. CSF evaluation of 14-3-3 protein was negative 16 months into her illness. Conclusions: CJD may present with slow progression and asymmetry. The 14-3-3 protein is likely not specific for CJD and may be a marker of rapid neuronal destruction. The 14-3-3 assay may not be clinically useful to rule out CJD in atypical dementia of slower onset where neuronal loss is less rapid.
P50. Psychiatric medication and abnormal behavior as predictors of progression in probable Alzheimer's diseaseOscar L. Lopez, Stephen R. Wisniewski, James T. Becker, François Boller, Cecilia Tutor, Steven T. DeKosky (Neuropsychology Research Program, Pittsburgh, PA)
Background: Psychiatric symptoms, especially psychotic symptoms, are important predictors of progression in AD. However, there are no data about how psychiatric medications affect progression of the disease. Methods: We examined baseline and follow-up behavioral symptoms (e.g., psychosis, depression, agitation, aggression, insomnia) and the use of psychiatric medication (e.g., sedatives-hypnotics, antidepressants, antipsychotics) in 179 mildly-moderately impaired probable AD patients participating in a longitudinal study of dementia. Patients were followed from 2.4 to 172 months (mean 49.5±27.4). Results: 9 patients (5%) were taking sedative-hypnotics, 16 (9%) antipsychotics, and 22 (12%) antidepressants at study entry. Patients on antipsychotics had lower MMSE scores and higher Blessed Dementia Rating Scale (BDRS) ratings for activities of daily living than patients without any medication. Proportional hazard analysis with time-dependent covariates for individual psychiatric symptoms and medications revealed that 1) the development of psychosis was associated with functional decline (time to BDRS≥15) and institutionalization and 2) aggression and agitation were associated with functional decline, after adjusting for age at study entry, education, MMSE, and BDRS. Antipsychotic medication was associated with functional decline, and sedative-hypnotics with death. Neither the presence of psychiatric symptoms nor the use of medication was associated with rate of cognitive decline (time to MMSE≤9). Conclusions: These findings indicate that the use of antipsychotics and sedatives in AD can affect the natural course of the disease. Psychosis, agitation, and aggression are important predictors of outcome in AD, even when the medication to treat them is taken into account.Support from Alzheimer's Disease Research Center Grant AG05133.
P51. Clinicopathological comparison of community-based and clinic-based cohorts of patients with dementiaFadi Massoud, Gayatri Devi, Yaakov Stern, Richard Mayeux (Columbia University, New York, NY)
Background: No studies have correlated clinical and pathological diagnoses of Alzheimer's disease in a community-based sample. Methods: We compared the sensitivity and specificity of clinical diagnosis of AD and neuropathologic diagnoses of two groups of demented patients: 63 patients from a memory disorder clinic and 26 from a community-based study. Results: Of the 63 clinic patients, 22 (35%) had a pathological diagnosis of pure AD, 22 (35%) a diagnosis of mixed AD, and 19 (30%) a diagnosis of “other dementia.” In the community sample, 6 (23%) had pure AD, 6 (23%) had mixed AD, 6 (23%) had vascular dementia, and 8 (31%) had a diagnosis of “other dementia.” For clinic patients, the sensitivity of the clinical diagnosis of AD was 98% and the specificity was 84%, while in the community, the sensitivity was 92% and the specificity was 79%. Conclusions: The sensitivity and specificity of clinical diagnosis of AD were not significantly different statistically between a group of clinic and community patients. Vascular dementia was more prevalent in the community sample. This difference may be accounted for by the fact that community patients were more likely to be older, less educated, African American, or Hispanic.Support from the McLaughlin Foundation and Grants AG07232, AG08702, and AG10963.
P52. Relationship of executive abilities to everyday tasks in Alzheimer's diseaseRaymond L. Ownby, David Loewenstein, Lynn Schram, Brian Mogosky (University of Miami Medical School, Miami, FL)
Background: It has been speculated that executive abilities deficits might be related to impairment in everyday functional activities in patients with AD. This study assessed the relationship of executive abilities to performance on a checkbook-balancing task in patients with mild to moderate AD. Methods: As part of a multidisciplinary assessment, patients were administered a battery of cognitive measures that included assessment of general intellectual as well as executive abilities (e.g., Trail Making Test, part B). Patients were administered the Direct Assessment of Functional Status (DAFS), a standardized battery that includes a checkbook-balancing task. The usefulness of executive function measures in addition to general cognitive measures in predicting patients' scores on the checkbook-balancing task was assessed via multiple regression. Results: After controlling for general cognitive ability, the Trail Making Test independently contributed to patients' scores on the checkbook-balancing task. Consistent with our hypothesis, a measure of executive abilities significantly added to prediction of performance on this real-life task. Conclusions: These results show that assessment of executive function in AD may be useful and related to functional behavioral deficits. The results thus suggest the importance of such assessment in patients with AD.
P53. Executive function deficits in Alzheimer's diseaseRaymond L. Ownby, David Loewenstein, Lynn Schram, Brian Mogosky (University of Miami Medical School, Miami, FL)
Background: Several authors (e.g., Albert, Proc Natl Acad Sci USA 1996; 23:13547–13551) have argued that executive functions are differentially more affected in early AD in relation to other cognitive functions. This study examined the usefulness of several measures of executive functioning in discriminating between patients with and without AD. Methods: As part of a multidisciplinary assessment at an outpatient memory disorders clinic, patients were administered a battery of cognitive measures that included assessment of general intellectual function, verbal skills, and memory as well as executive functions (e.g., Trail Making Test, part B). We assessed, via logistic regression, the additional usefulness of executive function measures over general cognitive measures in predicting which patients received a diagnosis of AD. Results: Although results showed that general cognitive measures were most important in discriminating between patients with and without AD, consistent with our hypothesis, measures of executive function significantly added to prediction of AD diagnosis. Conclusions: These results show that executive function assessment in AD may be useful and support the hypothesis that these functions are differentially affected in AD.
P54. A prospective study of Lewy body diseaseMichelle Papka, Randolph Schiffer, Carolyn Valone (University of Rochester School of Medicine and Dentistry, Rochester, NY)
Background: Lewy body disease (LBD) is coming to be recognized as the second most common cause of dementia in elderly people after Alzheimer's disease. Many of the clinical symptoms of LBD are similar to those associated with AD and Parkinson's disease. The purpose of this pilot study was to collect detailed, prospective, clinical data on patients with LBD, AD, and PD and to determine which, if any, measures may be useful in differentiating these patient groups for clinical diagnosis. Methods: Subjects were 8 patients who met consensus criteria for probable LBD, 10 AD patients (NINCDS-ADRDA criteria), 7 idiopathic PD patients who developed dementia at least 1 year following diagnosis, and 10 normal control subjects. A comprehensive standardized neuropsychological battery and a computerized cognitive battery (CDR, Inc.) were administered. Extrapyramidal signs and neuropsychiatric symptoms were assessed with the UPDRS and the Neuropsychiatric Inventory (NPI), respectively. Results: Patients and control subjects differed significantly on most measures, but there were few significant differences between patient groups. On the standardized neuropsychological battery, LBD patients were slower than AD patients on a test of psychomotor speed; semantic cues on a naming task were more helpful to PD than AD patients. On the computerized battery, AD patients were slower than LBD patients on a choice reaction time task, and LBD patients had slower reactions times than PD patients on a facial recognition task. UPDRS scores were higher in the PD group than any other group, and LBD patients had more extrapyramidal findings than AD patients. Resting tremor and difficulty with rapid alternating hand movements were greater in PD than LBD patients. The only patient group difference on the NPI was greater depression in AD compared with LBD patients. Conclusions: With the exception of psychomotor slowing and reaction times, comprehensive neuropsychological testing was not helpful in differentiating LBD from AD and PD patients. Neuropsychiatric symptoms also did not differentiate these patient groups, although depression was more predominant in AD than LBD. Neurological assessment of extrapyramidal signs was at least marginally helpful in distinguishing LBD from other patient groups. Given the small sample size tested, some potentially significant differences may not have been realized. We are continuing to assess patients in these populations for comparative purposes. The interpretation of these data also is limited by the lack of diagnostic certainty, which may be obtained only by neuropathological diagnosis.Support from NIH Training Grant T32 AG00107 and Rochester Alzheimer's Disease Research Center Grant P30 AG08665.
P55. Clinical and psychosocial characteristics of Caribbean and Anglo-Saxon dementia referrals in South FloridaRafael Rivas-Vazquez, Gustavo J. Rey, Enrique Carraza, Regina Mendoza, David Racher (Neurologic Center of South Florida, Miami, FL)
Background: The clinical and psychosocial characteristics of Hispanics presenting with dementia syndromes in the United States have not been well documented. We present data on a series of consecutive referrals for assessment of dementia in a large neurology practice in Miami, FL. Methods: 120 consecutive referrals for the evaluation of dementia syndrome were studied. Subjects were divided according to their place of birth (United States vs. Latin America/Caribbean). We examined differences between the groups in regard to diagnosis, severity of dementia (per MMSE and select neuropsychological variables), duration of disease, neurological utilization practices, and psychosocial variables (current living arrangements, education level). Results: The two groups did not differ significantly in overall education level or severity of dementia. The groups did differ in the presenting complaints that generated the neurological contact by the patient and family. Psychosocial variables, including neurological utilization practices and living arrangements, were also different between groups. Conclusions: These data demonstrate clinical and psychosocial differences between the groups. These findings provide important information regarding the clinical management of patients from different ethnic backgrounds.
P56. Combination therapies for vascular dementia: statistical analysis of clinical trial design issuesJeffrey L. Saver (University of California, Los Angeles, CA)
Background: Several vasoactive and neuroprotective agents for slowing progression of vascular dementia are currently available for clinical trial testing. These agents may have additive or antagonistic effects when used in combination. Methods: Systematic literature review identified drugs for vascular dementia presently available for definitive phase 3 trial testing. Agents in preclinical or phase 1–2 clinical development were excluded from this analysis. Clinical trials testing these agents were modeled, using international guidelines for dementia drug development. Results: 10 candidate agent classes were identified: salicylates (aspirin), thienopyridines (clopidogrel, ticlopidine), phosphodiesterase inhibitors (propentofylline), anticoagulants (warfarin), hormones (estrogen), antioxidants (alpha-tocopherol), deamination antioxidants (selegiline), calcium-channel blockers, choline precursors (citicoline), and gingko biloba. Taking only one agent from each category, possible regimens combining two or more agents number 1,024 (210). With liberal sample sizes of 350 patients per trial, phase 3 head-to-head testing of all combination regimens to determine the superior therapy would require enrolling 358,000 vascular dementia patients. To perform these studies in the United States at current enrollment rates in dementia trials would require performing trials for the next 180 years. Conclusions: Testing of multiple available agents for vascular dementia poses difficult challenges to the principles of evidence-based medicine. Potential solutions include hierarchical and multi-armed trials, surrogate outcome measures, and targeted preclinical testing.
P57. Alzheimer's disease and Parkinson's disease: differential awareness of cognitive and motor symptomsBenjamin Seltzer, Jennifer J. Vasterling, Charles Matthias (Tulane Medical School, VA Medical Center, New Orleans, LA)
Background: Alzheimer's disease patients underestimate their deficits, especially in cognitive function, compared with estimates provided by their caregivers and objective measures. We hypothesized that this is a disease-specific phenomenon that may not extend to all dementia syndromes. Methods: 13 Alzheimer's disease and 12 Parkinson's disease patients, equated for dementia severity as measured by MMSE and Dementia Rating Scale (DRS) total scores, were compared on their self-ratings of memory, self-care, and motor function as measured by the UPDRS. External measures were obtained by querying caregivers on the same UPDRS ratings, the clinician-based UPDRS motor exam, and cognitive testing. Results: PD patients reported more severe motor and self-care deficits than AD patients. Furthermore, these self-ratings reflected both caregiver- and clinician-based measures of these functions. In contrast, although AD patients were more impaired on the memory subscale of the DRS, the two groups did not differ in their self-ratings of memory. Conclusions: Awareness of deficit is not a pervasive phenomenon across all dementias and may relate to specific anatomical and pathological substrates.Support from the Department of Veterans Affairs and Tulane University.
P58. Depression and denial in Alzheimer's diseaseS. Sevush, A. Bertran, G. Peruyera (University of Miami, Miami, FL)
Background: Reports regarding the relationship between denial and depression in Alzheimer's disease have been conflicting. Differences in whether depression was measured by self-report or by caregiver report may have contributed to the variable findings. In the present study, the relationship between denial and depression was examined separately for self-reported and caregiver-reported patient depression. Methods: 297 patients with NINCDS-ADRDA probable AD were studied. Denial of memory impairment was assessed with the Awareness of Memory Impairment Scale (AMIS). Depression was assessed with the Cornell Depression Scale (CDS), with separate self-report and caregiver-report forms. Patient age, gender, education, disease duration, MMSE score, and caregiver's own mood served as covariates in multiple regression analyses. Results: Self-report CDS scores were lower than caregiver-report CDS scores (t-test, P<0.0001). Self-report CDS scores predicted AMIS scores (P<0.0001); caregiver-report CDS scores did not predict AMIS scores (P=0.48). Conclusions: AD patient awareness of memory deficit is correlated with self-reported, but not caregiver-reported, patient depression, a discrepancy that may explain some of the variability in prior studies. The findings suggest that AD denial extends beyond denial of memory deficit to denial of depressive symptoms as well.Support from the State of Florida Alzheimer's Disease Initiative.
P59. Cognition in late-onset depression subjects with delusionsMartine Simard, Diana Clarke, Robert van Reekum (Baycrest Centre and University of Toronto, Toronto, Ontario, Canada)
Background: There is now some evidence that late onset of depression (LOD) in elderly patients could be an early sign of dementia (van Reekum et al., Am J Geriatr Psychiatry, in press). Other data suggest that psychotic symptoms can predict more severe dementia (Lopez et al., Neurology 1997; 48:1521–1525). Little is known about cognition in LOD subjects with psychosis. Methods: The Mattis Dementia Rating Scale (MDRS) and the Ham-D are included in the admission evaluation for Baycrest Centre's Day Hospital for Depression. 93 LOD patients without CNS disease entered the program; 14 had delusions. Results: A logistic regression using MDRS status (≤123) as dependent variable showed that education (R=–0.27, P=0.00) and age (R=0.21, P=0.04) predicted MDRS status. Ham-D scores (R=0.11, P=0.06) and presence of delusions (R=0.08, P=0.09) tended to be predictors. After removing age and education, delusions tended to remain the only predictors. LOD+delusions patients stayed in the program for shorter periods (t-tests, P=0.039), tended to have higher Ham-D scores, and tended to derive less cognitive benefit from the program than did LOD patients without delusions (respectively, MMSE scores of 27.05±2.7 and 25.6±3.8 at baseline and, at discharge, 27.4±1.2 and 26.9±2.7). Conclusions: Delusions in LOD patients are associated with cognitive impairment.Support from a postdoctoral fellowship from the Alzheimer's Disease Society of Canada (M.S.) and from the Kunin-Lunenfeld Applied Research Unit of Baycrest Centre.
P60. Personality changes and degeneration of cerebral white matter in dentatorubral pallidoluysian atrophyChiharu Tamagaki, Akira Murata, Tetsuji Sakata, Satoru Asai, Kazutoshi Gonno, Katsunori Takase, Toshihiko Kinoshita (Kansai Medical University, Moriguchi City, Osaka, Japan)
Background: Dentatorubral-pallidoluysian atrophy (DRPLA) is a progressive brain disease that is often encountered in Japan. DRPLA seems rare outside Japan. Its cardinal symptoms are myoclonus, epileptic seizures, ataxia, choreoathetosis, and dementia. Dementia of DRPLA is thought to represent a subcortical dementia, and the main neuropathologic changes are a combined degeneration of the dentatorubral and pallidoluysian systems (Naito, Neuropathology 1996; 16:43–47). Personality changes are also common symptoms in DRPLA. Methods: Subjects were 9 cases of DRPLA, including 4 autopsy cases. The diagnosis of DRPLA was confirmed by DNA analysis (expansion of the CAG trinucleotide repeat). We analyzed correlation between clinical symptoms and neuroimaging (SPECT findings and MR images). Results: SPECT revealed basal ganglia hypoperfusion in all cases. Degeneration of cerebral white matter was seen in 5 of 9 cases (high-intensity area in T2-weighted MRI and myelin pallor in histological examination), in which there were also severe personality changes. Conclusions: All patients had subcortical dementia, which was associated with basal ganglia impairments. Also, we think that degeneration of cerebral white matter in DRPLA is associated with personality changes.
P61. Significant clinical and demographic moderators of effect on neuropsychological function in patients with Alzheimer's diseaseKonstantine K. Zakzanis (York University, Toronto, Ontario, Canada)
Background: It is well recognized that patients with dementia of the Alzheimer's type (DAT) undergo steadily progressive intellectual deterioration. Indeed, the sequence in which higher cognitive functions are lost and the temporal order in which behavioral and neurologic disabilities occur are important clues for establishing the clinical diagnosis. It is important, however, to document potential clinical and demographic variables of patients with DAT that might be related to cognitive deterioration (as it is indexed with commonly employed neuropsychological measures). Accordingly, a quantitative review of the literature was conducted. Methods: Meta-analytic methods were employed. Quasi-experimental studies published between 1984 and 1997 that incorporated patient samples meeting NINCDS-ADRDA criteria for probable Alzheimer's disease were included in the meta-analysis. Results: 199 studies met criteria for inclusion in the analysis. In total, clinical and demographic characteristics and neuropsychological test results from 7,156 patients with DAT and 8,772 normal healthy control subjects were recorded across primary studies. Significant product-moment correlations were evinced between age, duration of illness, education, and gender on several neurocognitive tasks and test variables. Conclusions: By knowing the effect of clinical and demographic variables on neuropsychological measures in patients with DAT, the clinician interpreting the results of a neuropsychological assessment is better able to establish the clinical diagnosis.
P62. Mildly demented Alzheimer's disease patients, but not mildly cognitively impaired Parkinson's disease patients, lack insight regarding their level of everyday executive functioningRonald F. Zec, Beverly Matthews, Kevin Vost, Rodger Elble, Stephen J. Markwell (Southern Illinois University School of Medicine, Springfield, IL)
Background: Executive functioning affects instrumental activities of daily living, and insight into the level and adequacy of one's own executive functioning skills is an important factor in developing and using compensatory strategies to improve everyday functioning. The rating scores of a mildly demented AD group, a mildly cognitively impaired PD group, and two separate normal elderly control samples were compared on ratings of everyday executive functioning done by the subject and by an independent rater (family member or friend). Methods: Subjects were 27 nondemented PD patients with mild cognitive impairment, 27 demographically matched normal subjects, and 18 mildly demented AD patients and their control group of 28 subjects. All PD subjects and all control subjects had MMSE scores ≥26. All AD patients had scores on the Alzheimer Disease Assessment Scale <15 (mean MMSE score=24.2). Everyday executive functioning was rated with the Dysexecutive Self-Rating (DEXs) and the Dysexecutive Independent Rating (DEXi) from the Behavioural Assessment of the Dysexecutive Syndrome. Results: On the DEX independent rater scores, the mildly demented AD group had considerably greater difficulty with executive functioning in everyday activities than the nondemented but mildly cognitively impaired PD group. A double disassociation was found with respect to the self-ratings of the groups in this study. The AD patient group rated themselves as less impaired than their control group rated themselves, whereas the PD patient group rated themselves as more impaired than their control group rated themselves. A double disassociation was also found with respect to the comparison of self-ratings and the independent ratings for the groups in this study. The AD group greatly underestimated their degree of executive functioning impairment relative to the DEX ratings provided by the independent raters, whereas the control groups and the PD group tended to rate themselves as having somewhat more difficulty with everyday executive functioning activities than indicated by the independent raters. Conclusions: This study demonstrates a lack of insight into everyday executive functioning impairments in a mildly demented AD group, but good insight in a nondemented PD group with mild cognitive impairment. Lack of insight can be interpreted as a breakdown in metacognitive processes in which patients have increasing difficulty self-monitoring and predicting their own performance.
P63. No evidence for a global or disproportionate impairment in executive functioning in nondemented patients with Parkinson's diseaseBeverly Matthews, Ronald F. Zec, Rodger Elble, Stephen J. Markwell (Adler School of Professional Psychology, Chicago, IL)
Background: Neuroanatomical and neuroimaging studies implicate involvement of frontal subcortical systems in the cognitive deficits of Parkinson's disease, and even nondemented PD patients have been described as having a frontal systems disorder characterized by deficits in executive functioning. We predicted that we would find disproportionate impairment on a battery of executive functioning relative to a battery of non-executive cognitive measures in PD patients. Methods: Subjects were 27 nondemented PD patients and 27 normal control subjects matched for age, education, and gender. All subjects had to have MMSE scores ≥26. The “cognitively intact” subgroups (9 PD patients and 18 normal control subjects) displayed intact performance on the battery of non-executive cognitive measures compared with age norms. Each subject was administered a battery of cognitive tests and a battery of executive functioning measures. Results: The PD groups were not impaired on a greater percentage of executive functioning measures than other cognitive measures. In the PD groups, 35% of the non-executive cognitive measures (44 of 127) were statistically impaired and 27% (39 of 143) of the executive functioning measures were impaired. Furthermore, when the cognitively intact PD and cognitively intact control subgroups were compared, virtually all of the statistically significant impairments in this PD subgroup disappeared; only 2% of the measures remained statistically significant on the executive functioning battery. Two measures that were statistically significant were two versions of a verbal planning test. Conclusions: Our prediction that a disproportionate percentage of the measures in the comprehensive battery of executive functioning would be significantly impaired in nondemented PD patients was not confirmed. It appears that both a bradyphrenia causing general cognitive impairment and specific executive functioning impairments account for these test results.
Assessment
P64. Relationship between substance abuse severity indicators and cognitive performance in a dual-diagnosis populationJeffery B. Allen (Center for Psychological Services, Dayton, OH)
Background: The high concurrence rate of traumatic brain injury and substance abuse are well known (Drubach et al., Maryland Medical Journal, October 1993, pp 989–993). Indeed, estimates of substance abuse in the TBI population approach 67% by some accounts (Sparedeo & Gill, Journal of Head Trauma Rehabilitation 1989; 4[1]:75–82). Additionally, the relationship between cognitive deficits and substance abuse treatment outcome has been indicated (Glenn & Parsons, International Journal of Addictions 1991; 26:237–254; Goldman, Neuropsychol Rev 1990; 11:75–101). However, the relationship between neuropsychological functioning and readiness for treatment has yet to be examined. The current study investigated the relationship between substance abuse severity, neuropsychological functioning, and readiness to enter treatment. Methods: The current study included 28 individuals dually diagnosed with a neurological disorder and substance abuse difficulties (52% males; mean age 33 years; 68% Caucasian, 21% African American; 80% reported 12 or more years of education). Upon admission to a treatment program, each individual was administered a number of measures of substance abuse severity (MAST), readiness for change/treatment (SOCRATES), community integration (CIQ) and quality of life (SWLS). The clients were also administered the Cognistat as a brief indicator of neuropsychological status. Along with descriptive information on the sample, correlation and regression analysis were used in an attempt to identify the general relationship between the various cognitive domains measured by the Cognistat and the SOCRATES as a measure of treatment readiness. Results: The mental calculation subtest of the Cognistat was significantly related to clients' readiness for change (r=0.393, P<0.05). The memory subtest of the Cognistat was also related to overall scores on the CIQ (r=0.337, P<0.05). An expected relationship between the client's reported substance abuse symptomology and general quality of life also emerged (r=0.327, P<0.05). Conclusions: Implications of patients' cognitive functioning levels for decision making regarding time to enter treatment, as well as the need for flexibility in the manner in which treatment is delivered, are discussed.
P65. Usefulness of the Visual Verbal Test as a measure of executive function in the assessment of dementiaBarbara Collins, Andrée Tellier, Katharina Schulze (Ottawa Hospital, General Site, Ottawa, Ontario, Canada)
Background: Failure to address executive functions is a serious shortcoming of most dementia screening tests. We have previously suggested that the Visual-Verbal Test (VVT) might be easily adapted for this purpose. The VVT requires that the respondent choose three of four figural stimuli that have a common attribute not shared by the fourth and, having done so, select three of the same four stimuli according to a second principle. In a previous study (Collins & Tellier, Canadian Journal on Aging 1994; 13:368–377), we identified a subset of the VVT items, which we called the modified VVT (mVVT), for which the two target responses appeared to be of equal difficulty and on which failure to obtain the second response could thus be regarded as a set-shifting error. We found that second-response errors on the mVVT correlated significantly with perseverative errors, but not nonperseverative errors, on the Wisconsin Card Sorting Test. In contrast, first-response errors on the mVVT did not correlate with either WCST error measure. Methods: The current study sought to extend these findings in a sample of 17 individuals with age-associated memory impairment (10 females and 7 males; mean age 68.18, SD=8.43). Results: In contrast to our previous findings, a significant bias in response order was found for 4 of the 10 test items on the mVVT (χ2<0.05). Again, however, the 2 target responses on all 10 of the mVVT test items were obtained with equal frequency by our subjects (χ2>0.05). We again found that the second-response score on the mVVT correlated significantly with WCST perseverative responses (r=–0.42, P<0.05), but not with WCST nonperseverative errors (r=–0.13, P=0.32). The first-response score on the mVVT did not correlate with either of these WCST variables. Neither total score nor second-response score on the mVVT correlated with either frontal or parietal perfusion on SPECT. However, a trend toward significance (P<0.10) was noted in correlations between the mVVT first-response score and both frontal and parietal flow. Conclusions: These results corroborate our previous findings that second-response errors on the mVVT reflect set-shifting problems. We recommend adding the mVVT to the dementia screening battery as a brief measure of executive function.
P66. Neuropsychological performance on fluency tasks in male and female college-level athletes with a history of previous head injuryLaura J. Julian, Naomi E. Shoss, Ruben J. Echemendia (Pennsylvania State University, University Park, PA)
Background: Researchers have begun to evaluate the presence of long-term and cumulative effects of previous mild head injuries on cognitive functioning. The purpose of this investigation is to evaluate performance on both nonverbal and verbal fluency tasks in individuals with and without a history of previous head injury. Methods: Neuropsychological tests used included the Ruff Figural Fluency Task (RFFT) and the Controlled Oral Word Association Test (COWAT). Researchers have previously concluded that parts 1, 4, and 5 of the RFFT are distinct and can be considered analogous to the three letter cues used in the COWAT. Participants included male and female college level athletes (N=75) who participated in a larger investigation evaluating mild head injuries in athletic populations. Results: Among males with a history of head injury, performance on these two measures was significantly correlated (r=0.88). Gender differences on these fluency measures were also noted. Statistical results and clinical implications will be discussed.
P67. Assessing neuropsychiatric symptoms in clinical practice: the Neuropsychiatric Inventory Questionnaire (NPI-Q)Daniel I. Kaufer, Jeffrey L. Cummings, Patrick Ketchel, Vanessa Smith, Audrey MacMillan, Oscar L. Lopez, Steven T. DeKosky (University of Pittsburgh, Pittsburgh, PA)
Background: Clinical research studies using the Neuropsychiatric Inventory (NPI), a validated informant-based interview, have demonstrated differential symptom profiles among dementia syndromes and shown it to be sensitive to therapeutic interventions in Alzheimer's disease. The purpose of this study is to cross-validate a brief questionnaire form of the NPI (NPI-Q) for assessing neuropsychiatric symptoms and their response to treatment in routine clinical practice. Methods: The 12 NPI symptom domains are assessed on the NPI-Q by a screening question. Positive symptom domains are rated in terms of Severity and associated Caregiver Distress by using NPI scaling criteria. Data comparing the NPI and NPI-Q were obtained from 57 AD patients and their caregivers. Results: Spearman correlations between NPI Total and NPI-Q Severity scores (r=0.88) and between NPI and NPI-Q Distress scores (r=0.87) were highly significant (both P<0.0001). The number of symptoms reported per subject was slightly higher on the NPI-Q (mean=4.5) than the NPI (4.3). The frequency of parallel individual symptoms differed on average by less than 5%. Conclusions: The Neuropsychiatric Inventory Questionnaire shows good agreement with the NPI and provides a brief, informant-based neuropsychiatric symptom assessment suitable for use in everyday clinical practice.Support from NIA, John Douglas French Alzheimer's Foundation, and a Merck-AFAR Clinical Geriatric Pharmacology Fellowship.
P68. Pre-injury neuropsychological assessment of college athletes at risk for mild head injuryR. Scott Mackin, Ruben J. Echemendia (Pennsylvania State University, University Park, PA)
Background: The Pennsylvania State University Cerebral Concussion Program (PSUCCP) uses a neuropsychological screening battery to assess cognitive functioning in college athletes who are at high risk for incurring head injuries. A unique aspect of this program is the acquisition of baseline (pre-injury) neuropsychological data. Collecting individual baseline data rather than using group norms is time and labor intensive, yet it allows for individualized comparisons of neuropsychological functioning preinjury and postinjury. The purpose of this investigation is to evaluate the presence of individual differences on the baseline measures in this population. Methods: 425 university athletes were assessed prior to mild head injury by using the PSUCCP testing battery (11 neuropsychological tests) during the 1995–1998 seasons. Results: Analysis of the baseline neuropsychological data (ANOVA) indicates significant variability in this population on measures of attention, concentration, and speed of information processing. Conclusions: These results emphasize the critical importance of baseline neuropsychological testing in athletes who are at risk for cerebral trauma. The clinical implications of these results within the context of assessment procedures will be discussed.
P69. Litigation versus nonlitigation patient performance on the Portland Digit Recognition Test and the Victoria Symptom Validity TestEdward A. Peck, Stephanie A. Mitchell, Erin B. Doudera, Anne W. Peck (Neuropsychological Services of Virginia, Richmond, VA)
Background: The increased use of neuropsychological assessment in litigation has led to renewed attempts to clarify the role of motivation on test performance. The Portland Digit Recognition Test (PDRT) has been shown to be a valid test of patient motivation. However, the PDRT can take up to 40 minutes to administer. Consequently, a test that requires less time to administer, such as the Victoria Symptom Validity Test (VSVT), needs to be investigated as another measurement of test-taking motivation. This study measures the relationship of the VSVT with the PDRT in assessing the test-taking attitude of patients participating in neuropsychological testing. Methods: 60 adult patients with defined medical problems were seen for comprehensive neuropsychological assessment. The subjects were grouped on the basis of whether or not they were involved in litigation/compensation issues relating to their health problems. 35 were assigned to the litigation group and 25 were assigned to the nonlitigation group. Results: The VSVT and the PDRT appeared to generate similar pass/fail performances for the nonlitigation group. There were no failures for the nonlitigation group on either the PDRT or the VSVT. Failures were found only in the litigation group. Statistical analysis of PDRT and VSVT scores revealed statistically significant differences based on litigation versus nonlitigation assignment. Several other neuropsychological tests were also found to be significantly different on the basis of this grouping. Conclusions: It does appear that the classification of a patient on the basis of involvement in litigation can be a factor in neuropsychological test performance. This reinforces the need to provide objective measurement of test-taking motivation as part of the standard of practice for patients involved in litigation. The rationale for additional research in this area is discussed.
P70. Variability in the Boston Diagnostic Aphasia Examination in a healthy Colombian worker populationDavid A. Pineda, Silvia Mejia, Monica Rosselli, Alfredo Ardila, Maria G. Romero, Claudia Perez (University of San Buenaventura, Medellín, Colombia)
Background: The aim of this study was to analyze the influence of age, gender, socioeconomic status (SES), academic achievement (education), and type of occupation on the performance of the Boston Diagnostic Aphasia Examination (BDAE), Spanish version. Methods: The BDAE was administered to a group of 156 normal subjects who were 19 to 60 years old and occupationally active. Results: A descriptive analysis showed that some subjects (1% to 3%) scored in the pathological range of the centiles and profiles of the BDAE. Multivariate analysis of variance (P<0.05) demonstrated a significant effect of education over most of the BDAE subtests. Females outperformed males on some reading and writing subtests. SES had an effect on Body Part Identification and Naming. Significant differences were observed between younger and middle-aged groups in Confrontation Naming and Oral and Word Picture Reading. The older group scored significantly lower than the younger group in Serial Writing and Sentences to Dictation. No differences were observed between the older and the middle groups. Only oral spelling was affected by the type of occupation, but a significant interaction of occupation and level of education was found. Conclusions: Language tests are influenced by demographic variables, particularly education. Normal variability on the BDAE should be considered when dealing with clinical populations. (Revista de Neurologia, in press.)
P71. Influence of age, gender, education, socioeconomic status, and occupation on the Boston Diagnostic Aphasia Examination, Spanish version: factor and stepwise regression analysesDavid A. Pineda, Monica Rosselli, Alfredo Ardila, Silvia Mejia, Maria G. Romero (University of Antioquia, Medellín, Colombia)
Background: The Boston Diagnostic Aphasia Examination Battery (BDAE) is one of the most widely used aphasia tests worldwide. Information about general population performance, however, is limited. This paper analyzes the effects of gender, age, socioeconomic status (SES), academic achievement, and occupation on the BDAE, Spanish version. Methods: The BDAE was administered to 156 occupationally active participants (ages 19–60; 75 males, 81 females) from two SES groups. Results: Gender and age had a significant effect on some reading and writing subtests. Body-part identification and naming scores were significantly decreased in the low SES group. Education had a significant impact on most of the BDAE subtests. A stepwise regression model showed that academic achievement was best able to predict the variance of several BDAE scores with a low (<15%) to modest (>17%) but significant capability (MANOVA, P<0.01). A factor analysis disclosed seven factors that explained 67% of the total variance.
P72. Evaluation of “executive” functions in HispanicsGustavo J. Rey, Rafael Rivas-Vazquez, Esther Feldman, Enrique Carrazana (Neurologic Center of South Florida, Miami, FL)
Background: The assessment of executive functions is an integral component of neurobehavioral evaluations. Disruption of these skills is related to pathology of frontal brain systems and typically results in serious impairments in the performance of psychosocial and vocational responsibilities. These alterations may not be evident in bedside exams, and formal neurobehavioral assessment is frequently required to characterize the nature and severity of the disorder. For the first time in the literature, we present data on the performance of Hispanics residing in South Florida on two commonly used measures of executive skills: the Wisconsin Card Sorting Test and the Spanish Stroop Color-Word Test (SSCWT). Methods: Subjects were drawn from a sample of 120 normal controls participating in more extensive standardization study of neuropsychological instruments in South Florida. Exclusionary criteria included a history of neurological or psychiatric disorder. The MMSE and BDI were administered to all subjects to exclude individuals meeting criteria for dementia and depression, respectively. Results: For both variables, education and age proved to influence significantly performance on the test instruments. For the WCST, the pattern of performance was nearly identical to that published for the English-speaking, North American sample. Normative data will be presented for the SSCWT broken down by age and education. Conclusions: We present new normative data on two measures of executive functioning in Hispanic subjects residing in South Florida. The pattern of performance on the WCST was nearly identical to the existing, published North American norms. For the first time, we introduce the SSCWT and provide normative data on this measure.
P73. Prevalence and severity of executive cognitive impairment among diabetic outpatientsDonald R. Royall, Laura K. Chiodo, Marsha J. Polk (Departments of Psychiatry, Medicine, and Clinical Pharmacology, University of Texas at San Antonio, TX)
Background: Diabetes mellitus has been associated with both mild cognitive impairment and frontal cerebral blood flow reductions by SPECT. We wondered if diabetic outpatients show executive cognitive function (ECF) impairment as well. Methods: Subjects were 117 Hispanic diabetic outpatients (means: age, 63.3±13.6 yr; education, 10.4±5.4 yr). Inclusion criteria were 1) history of non-insulin-dependent (type II) diabetes mellitus; 2) age >55 years; 3) presence of one or more diabetic complications. Exclusion criteria were 1) history of Alzheimer's disease; 2) evidence of cortical stroke (by chart review) or clinical hemiparesis; 3) history of psychosis; 4) history of alcohol or substance abuse; 5) history of anxiety or posttraumatic stress disorder; 6) corrected vision <20/200 OU; 7) <6 years of formal education. Subjects were given a brief psychometric evaluation that included the Executive Interview (EXIT25, mean=16.4±6.4; impaired scores), the MMSE (mean=26.0±3.0), and an Executive Clock-drawing Task (CLOX). The CLOX is subdivided into an ECF-sensitive paradigm (CLOX1; mean=9.9±2.9; impaired scores) and an alternative that is more sensitive to constructional skills (CLOX2; mean=13.1±1.7). Results: 26 subjects (22% of the sample) failed the MMSE at 24/30. 69 subjects (59%) failed the EXIT25 at 15/50. Of these, 44 (64%) had MMSE scores >24/30. ECF-impaired cases (EXIT25 >15/50) detected by the MMSE differed from those not detected only with regard to their CLOX1 scores (detected: n=25, CLOX1=8.2±3.4; not detected: n=44, CLOX1=10.0±2.2; different by ANOVA: F=7.7, df=1,67, P<0.001). These differences persisted after adjusting for age, first language, and education (MANOVA: F=7.9, df=1,64, P=0.006). Conclusions: The majority of diabetics seeking outpatient treatment for diabetic complications may have clinically significant ECF impairment. This impairment is not well detected by the MMSE. Possible causes for this impairment include depression, vasculopathy, and iatrogenic hypoglycemia. ECF impairment is a potentially reversible cause of disability.Support from the South Texas Health Research Center.
P74. Evolution of the traditional mental status examination of cognition: from unstructured to structured evaluationJames R. Slaughter, Kathy Slaughter, George Johnstone, Laura Schopp, Stacey Holmes (Department of Psychiatry, University of Missouri, Columbia, MO)
Background: We hypothesize that the mental status examination is undergoing an evolution from an unstructured to a structured examination. We analyzed the components of the mental status examination prior to structured examinations and the original reports of structured instruments. Methods: Content and methodological criteria based on expert opinion were used to critique the studies identified by medline and PsychINFO literature searches. We reviewed more than 5,000 citations and abstracts and analyzed 96 scientific reports concerning mental evaluation of cognition. Results: Structured mental status examinations based on the traditional mental status examination of cognition yielded a wide range of compliance with content and methodological criteria, yet structured instruments, such as the MMSE, yielded high compliance rates. Conclusions: Our data support the evolution of the mental status examination to a structured evaluation.Support from the Department of Veterans Affairs, HSD, HPE Grant 51-85-001.
P75. Assessing internal mood state in dementia: validation of the Visual Analog Mood ScalesJennifer A. Latham, Geoffrey Tremont, Jessica A. Somerville, James E. Arruda, Robert A. Stern (University of Rhode Island, Kingston, RI)
Background: The Visual Analog Mood Scales (VAMS) were developed by Stern and colleagues (Stern, Psychological Assessment Resources, Inc., 1997; Stern et al., Aphasiology 1997; 11:59–71) to provide a brief, standardized measure of mood state appropriate for patients with neurologic disease who have limited cognitive and linguistic abilities. Each scale consists of a labeled face representing a mood (e.g., “sad”) at the bottom of the page, connected by a 100-mm vertical line to a labeled neutral face at the top of the page. Patients are asked to place a mark across the line at the point that represents how they currently feel. Although the VAMS have proven to be a valid measure for use with psychiatric, neurorehabilitation, and acute stroke patients, their validity in assessing mood in dementia patients has yet to be established. Methods: Subjects included 18 inpatients and outpatients referred for neuropsychological evaluation, all of whom met criteria for dementia (Alzheimer's, vascular, hydrocephalus, or mixed). Subjects completed the VAMS and a modified (yes-no) version of the Profile of Mood States (POMS). The convergent and discriminant validity of the VAMS was analyzed by statistically examining the multitrait-multimethod correlation matrix by way of a Monte Carlo Multitrait-Multimethod Analysis Package. Results: All dementia patients were able to complete the VAMS in less than 5 minutes. The scales demonstrated good convergent validity (monotrait-heteromethod, Mr=0.63, P<0.01), which also indicates a strong contribution of trait variance. Discriminant validity was supported by the large contribution of trait variance relative to the nonsignificant contribution of method variance (heterotrait-monomethod, Mr=0.20, P>0.05). Conclusions: The VAMS provide a brief, valid, easily administered means of assessing mood state in patients with a wide range of neuropsychiatric conditions, including dementia.
P76. The Hooper Visual Organization Test: modification for use in dementia assessmentAndrée Tellier, Barbara Collins, Katharina Shulze (Ottawa Hospital, General Site, Ottawa, Ontario, Canada)
Background: Although originally designed for the generic detection of “organic brain pathology,” the Hooper Visual Organization Test (HVOT) has come to be known for its visual-perceptual demands and for its capacity to detect frontal system dysfunction given its requirements for organization and synthesis and its ability to elicit fragmented responses. Its sensitivity to frontal impairment (such an index being traditionally absent from standard mental status testing), brief administration time, and the lack of aversion to it have helped promote its popularity in the context of geriatric cognitive assessments. However, more data are needed on the capacity of the HVOT to differentiate between various types of dementias. As well, its split-half reliability needs to be established in an elderly clinical sample in order to determine the soundness of using split forms of the test when wishing to avoid practice effect in the context of serial neuropsychological testing. Methods: The sample consisted of 106 outpatients referred to a specialized memory disorder clinic (56.6% female; mean age 71.04 yr, SD=8.33; mean education 11.51 yr, SD=3.95). Results: The split-half reliability of the HVOT based on the overall sample was high (r=0.72, P<0.000). The overall HVOT performance of two distinct clinical dementia groups matched on MMSE severity (40 Alzheimer and 43 other causes, including vascular changes, alcohol, Lewy body disease, hypoxia, remote head injury, and frontotemporal dementias) was virtually identical (respective means of 19.4 and 19.0; t=0.37, df=81, P=0.72). Conclusions: The present findings provide support for the use of split halves of the test in the context of serial testing of elderly individuals. However, the test lacks the ability to differentiate among various types of dementias.
P77. A new test of verbal switching for the detection of frontal lobe dysfunctionElizabeth K. Warrington (Dementia Research Group, National Hospital for Neurology and Neurosurgery, London, UK)
Background: Executive functions in their broadest sense may be impaired in patients with frontal lobe lesions. The Wisconsin Card Sorting Test, perhaps the most robust test for frontal lobe dysfunction, requires the flexibility to switch a response pattern to meet the change in task demands. However, this task has only two category switches, and normal subjects tend to score at ceiling. Verbal fluency tasks also incorporate a switching component, and it was hypothesized that a word generation task that maximized a switching requirement might provide a more satisfactory verbal measure of frontal lobe dysfunction. Methods: We devised a new test of homophone meaning generation that requires multiple switches between verbal concepts (e.g., tick=insect, correct, etc.). Normative data were obtained from a sample of 170 control subjects. 71 patients with unilateral anterior or posterior cerebral lesions were also tested. Results: A normal distribution of scores was obtained in the standardization sample. The anterior lesion groups were more impaired than the posterior groups. There were no significant differences due to laterality. Conclusions: This homophone meaning generation task is a valid measure of frontal lobe dysfunction, and it has the advantage of psychometric properties that permit measurement of the degree of impairment.
P78. Validity of neuropsychiatric measures with dichotomously scored itemsJohn L. Woodard, Bradley N. Axelrod (Memory Assessment Clinic and Alzheimer's Disease Program, Georgia State University, Atlanta, GA)
Background: Neuropsychiatric measures consisting of dichotomously scored items are commonly used in clinical assessment. Clinical guidelines frequently recommend cutoff scores be used after summing these items to determine the presence or degree of a particular attribute, such as depression. However, blind application of such cutoffs neglects the question of whether the total score is significantly different from chance. Methods: The z approximation for the binomial theorem was used to establish the range of scores on the Geriatric Depression Scale (GDS) that was not significantly different from chance, and the proportion of GDS scores inside and outside this range was examined in a convenience sample of 334 elderly patients (mean age=75.5 yr, SD=7.7) who were seen for neuropsychological evaluation. Results: Of the total sample, 241 patients obtained scores of 122 or lower on the Mattis Dementia Rating Scale (impaired range). Of these patients, 46.5% (n=112) obtained GDS scores in the chance range at the P<0.01 level (i.e., scores from 9 through 22)—raising possible questions regarding their accuracy in responding and overall test-taking approach—contrasted with 46.5% below a score of 9 and 7% above a score of 22. Conclusions: The binomial theorem can be helpful in identifying scores on measures with dichotomously scored items that exceed chance performance. These scores may be interpreted with the greatest confidence, particularly when assessing incomplete effort or random responding for patients who may vary with respect to response accuracy.
P79. A new measure in the assessment of amnesiaKonstantine K. Zakzanis, Larry Leach, Morris Moscovitch (Department of Psychology, Baycrest Centre for Geriatric Care, Toronto, Ontario, Canada)
Background: Severely impaired memory isolates individuals from emotionally or practically meaningful contact with the world about them and deprives them of a sense of personal continuity, rendering them passive and helplessly dependent. Several neuropsychological tasks have been developed to document the severity of amnesia in terms of “memory span” or “supraspan.” Although such tasks remain popular for documenting short-term retention, their ecological validity is not immediately obvious. Methods: We present a bedside task that can measure the time span within which the patient with amnesia experiences continuity. We call this measure “span of temporal continuity.” That is, the integrity of memory function was tested in a way that eliminated the formal experimental paradigm by engaging the patient in everyday behavior such as informal conversation, where memory span could be quantifiably documented. Results: The results of an experiment on 3 patients across 8 weeks are presented. Conclusions: On the basis of our findings, we conclude that our measure of continuity can document the severity of amnesia without concern about task generalizability or task artifact from potential moderators of effect such as gender, education, race, or difficulty. Moreover, span of continuity can provide an index of recovery from neurological insult that is free of practice effects on test-retest evaluation and can perhaps provide an index of the day-to-day progression of memory deterioration seen in dementia.
Traumatic Brain Injury
P80. Head injury in sex offenders with and without bipolar disorderMelissa P. DelBello, Cesar A. Soutullo, Molly E. Zimmerman, Kenji W. Sax, Susan L. McElroy, Stephen M. Strakowski (University of Cincinnati, Cincinnati, OH)
Background: Although up to 33% of sex offenders may have bipolar disorder, the relationship between sexual violence and affective disorders remains unclear (McElroy et al., American Psychiatric Association Annual Meeting, 1998, NR424). One potential mediating factor may be head injury, which has been associated with the onset of both abnormal sexual behaviors and mania. We examined the occurrence of head trauma in sex offenders with and without bipolar disorder. Methods: 25 sex offenders with (n=9) and without (n=16) bipolar disorder were assessed with the Structured Clinical Interview for DSM-IV and were evaluated for previous episodes of loss of consciousness (LOC) resulting from head trauma. Results: Sex offenders with bipolar disorder had significantly more episodes of LOC (n=7; 77%) resulting from head trauma than those without bipolar disorder (n=4; 25%; F=4.48, df=1,22, P=0.05). 6 of the 7 subjects with bipolar disorder and head trauma had their first LOC episode prior to the onset of bipolar disorder and/or their first sexual offense. Conclusions: Sex offenders with bipolar disorder were more likely to experience an episode of head trauma than offenders without bipolar disorder. In most subjects, head injury occurred prior to their first sexual offense and/or the onset of bipolar disorder, suggesting that sex offenders with a history of head trauma should be carefully assessed for the presence of bipolar disorder.
P81. Profound amnesia and confabulation following traumatic brain injuryJason A. Demery, Robert E. Hanlon (University of Florida, Gainesville, FL)
Background: It is axiomatic that amnestic disorder and confabulation may persist following aneurysmal hemorrhage of the anterior communicating artery, alcoholic Korsakoff's syndrome, or dementia of the Alzheimer's type. However, there is a paucity of literature that addresses this issue following traumatic brain injury. Methods: We present the case of a 43-year-old male who was involved in a motorcycle accident and sustained right temporal and left frontotemporal contusions. Follow-up CT scan at 7 months postinjury confirmed these findings and showed encephalomalacia of the contused sites. Our patient underwent neuropsychological evaluations at 2 months and 9½ months postinjury to identify any resolution of his neurocognitive impairments. Results: Acute neuropsychological findings revealed profound amnesia and confabulation typically observed in the acute phase of recovery. However, follow-up evaluation at 9½ months postinjury showed persistent and severe global amnesia and profound confabulation despite superior nonverbal intelligence, above-average attentional and perceptual abilities, and preserved procedural memory. Conclusions: This case suggests that amnesia and concomitant confabulation may also persist following TBI and supports previous research suggesting a disassociation between declarative and procedural memory functions. The role of the frontal lobes in confabulation and implications for neurorehabilitation are addressed.
P82. Chronic pain effects on neuropsychological test findings: differential diagnostic dilemmaMichael F. Martelli (Concussion Care Centre of Virginia, Glen Allen, VA)
Background: The assessment of neuropsychological functioning has become a common practice in the evaluation of patients sustaining traumatic brain injury. Frequently, diagnosis of mild traumatic brain injury is based on neuropsychological test findings as the primary and most sensitive measure of such injuries. Given the frequent presence of posttraumatic headache and other types of chronic pain, however, the validity and utility of neuropsychological test-based inferences necessarily depend on assurances that chronic pain does not affect neuropsychological test results. Methods: In the current paper, investigations of the effects of headache and general chronic pain on neuropsychological test findings are reviewed. Results and Conclusions: This review reveals that chronic headache pain, and chronic pain generally, exert a significant and negative effect that poses a challenge to differential diagnostic efforts in the evaluation of mild brain injury. Further, the pattern of neuropsychological impairments observed appear quite similar to those produced by persons sustaining mild brain injuries. Consistent recent findings regarding regional cerebral blood flow abnormalities in persons with chronic pain offer added support for these conclusions. In differential diagnosis in cases of neuropsychological evaluation for brain injury, especially for suspected mild brain injury, these findings clearly indicate that pain is to be considered a factor in interpreting test results.
P83. Abnormal brain activation following mild traumatic brain injury: a functional MRI study of working memory processing loadT. McAllister, A. Saykin, L. Flashman, S. Johnson, M. Sparling, S. Guerin, C. Moritz, J. Weaver, A. Mamourian, N. Yanofsky (Dartmouth Medical School, Lebanon, NH)
Background: Although there is evidence that memory, attention, and speed of information processing are impaired shortly after mild traumatic brain injury, there is controversy about the etiology and extent of these cognitive deficits. We examined patterns of regional brain activation during a working memory task using functional MRI. Methods: 12 consecutive MTBI patients (Glasgow Coma Scale score: 13–15, loss of consciousness <20 min) were studied an average of 3 weeks after their injury and compared with 11 control subjects. Both groups completed symptom checklists, a comprehensive neuropsychological assessment, structural MRI, and echo-planar fMRI (GE 1.5-T scanner with local gradient coil). Subjects performed a working memory task (the auditory N-Back) during the fMRI. Results: The MTBI group had no neuropsychological deficits other than slowed reaction times, but they had significantly more complaints about their memory function. fMRI activation in regions associated with working memory occurred in both groups with increased activation in response to higher processing demand. With a further increase in working memory load, control subjects showed little increase in activation, whereas the MTBI group showed an extensive increase in activation, despite equivalent accuracy. Conclusions: These results provide evidence of abnormal brain activation patterns in patients shortly after MTBI. Subjects with MTBI appear to recruit additional neural resources in order to maintain equivalent task performance. Longitudinal studies of these activation changes are in process and may shed light on the physiological substrate of recovery from MTBI.Support from NIDRR Grant H-133670031.
P84. Relationship of psychopathology to postconcussive symptoms one month after mild traumatic brain injuryThomas W. McAllister, Laura A. Flashman, Molly B. Sparling, Andrew J. Saykin, Robert Ferguson, Norm Yanofsky (Dartmouth Medical School, Lebanon, NH)
Background: MTBI results in a variety of cognitive, somatic, and emotional sequelae often referred to as the postconcussive syndrome (PCS). About 10% of MTBI patients develop a persistent PCS, which has been variously attributed to neural injury, premorbid psychopathology, comorbid depression, posttraumatic stress disorder, and compensation issues. Few studies have evaluated prospectively these putative etiological factors shortly after MTBI that may be predictive of persistent symptoms. Methods: 14 consecutive MTBI patients (Glasgow Coma Scale score 13–15; LOC <20 minutes) were studied 1 month postinjury and compared with 14 control subjects. Both groups were given a head injury symptom checklist, neuropsychological assessment, SCID, Ham-D, State-Trait Anxiety Inventory, and a self-report measure assessing acute and PTSD symptoms (PCL-S). Results: None of the MTBI patients had a diagnosable psychiatric disorder or were actively pursuing compensation claims at the time of assessment. Patients did have significantly higher scores on the head injury checklist and on the PCL-S than did control subjects. Even when corrected for two items that directly overlap with the PCS (lack of memory for traumatic event, trouble with attention/concentration), there remained a strong trend, with several patients experiencing clinically significant stress-related symptoms. Although Ham-D scores were elevated in the MTBI group, much of this was related to items overlapping with PCS. State-trait anxiety scores did not differ between groups. Conclusions: Within 1 month of their TBI, patients developed PCS symptoms in the absence of premorbid psychopathology or significant levels of postinjury depression, anxiety, or stress-related symptoms. This is consistent with a neural injury model of PCS symptom causation. However, a subgroup of MTBI patients also reported clinically significant, although subthreshold, stress-related symptoms. These patients will be followed longitudinally to determine whether this predicts development of persistent PCS.Support from NIDRR Grant H-133670031.
P85. Attention deficits and IQ in patients with closed head injuryAleksandra M. Milović, Dragan M. Pavlović, Gordana G. Ocić (Institute of Neurology, Belgrade, Serbia)
Background: Attention is a basic brain function necessary for normal cognition. Traumatic brain injury has deleterious effects on attentional processes and impairs various cognitive functions. We examined the mutual impact of attentional deficits and IQ in patients with traumatic brain injury. Methods: In 38 patients with moderate to severe closed traumatic brain injury, we administered the Wechsler Intelligence Test–Serbian version, Trail Making Test part B (TMT-B), and WMS-R Attention and Concentration Index. Patients were divided into two groups: those with IQ ≥90 and those with IQ ≤89. Results: Attention and Concentration index and all scores on this scale as well as TMT-B score were lower in the group with lower IQ. The mean index in the higher IQ group was 99.94 and in the lower IQ group, 76.50. TMT-B was 138.06 in the first and 232.00 in the second group. Conclusions: Attention and intelligence are impaired in patients with closed traumatic brain injury. Lower IQ is usually associated with more pronounced deficits of attention and concentration.
P86. Developing, implementing, and evaluating a mild traumatic brain injury programDavid D. Nowell (DATAHR Rehabilitation Institute, Brookfield, CT)
Background: Mild traumatic brain injury has only recently begun to be acknowledged as a cause of neurologic deficit (Zasler, Journal of Head Trauma Rehabilitation 1993; 8[3]:13–29). Sequelae may include headache, fatigue, and cognitive inefficiency (Alexander, Neurology 1995; 45:1253–1260; Ciccerone et al., Journal of Head Trauma Rehabilitation 1995; 10[3]:1–17) Methods: In our MTBI treatment program, management of the postconcussive patient may include consultation with neurologist for treatment of sleep, pain, and mood complaints; speech therapist for cognitive rehabilitation; physical and occupational therapists for functional limitations; and psychotherapist for adjustment to subjective disability. Neuropsychological evaluation may assist patient and treatment team in understanding the nature and severity of cognitive deficits. Follow-up questionnaires completed by MTBI program participants reflected patient satisfaction as well as symptom reduction and functional gains. At this writing, data are available for the 7/95–6/97 program period. Results: Participants reported that the MTBI program met or exceeded their expectations. 78% of participants reported returning to normal community functioning. 92% reported symptom reduction in the areas of presenting complaints. 82% demonstrated improvement on a measure of cognitive efficiency. Conclusions: Participation in a multidisciplinary MTBI program may increase return to normal functioning and relieve somatic and cognitive complaints associated with MTBI.
P87. Lateralization of memory impairments in closed traumatic brain injuryGordana G. Ocić, Dragan M. Pavlović, Aleksandra M. Milović (Institute of Neurology, Belgrade, Serbia)
Background: Declarative memory systems are thought to be lateralized, with verbal memory served by the left and visual by the right hemisphere. Lesions in traumatic brain injury are typically located in temporal and frontal lobes and can serve as a model to explore lateralization of memory. Methods: Patients were 41 traumatic closed brain injury victims with moderate and severe trauma, 11 (26.83%) with lesion only in the right hemisphere, 12 (29.27%) only in the left, and 18 (43.90%) with lesions in both hemispheres. Lateralization was determined by CT scans. Patients were tested with WMS-R; Rey Auditory Verbal Learning Test (RAVLT) learning, delayed recall, and recognition; and Rey Complex Figure (RCF) copy and delayed recall. Results: Bilateral lesions group showed the lowest scores on all measures of memory. Left lesion group had lower scores than right lesion group on general, verbal, visual, and delayed memory on WMS-R, as well as RAVLT learning, but higher on RAVLT delayed recall and RCF copy and delayed recall. Conclusions: Bilateral lesions have the greatest impact on memory; left hemisphere lesions have a greater impact on both verbal and visual memory (more on verbal); and right hemisphere lesions have impact on visual memory.
P88. Impact of executive functions on constructional apraxia in patients with closed traumatic brain injuryDragan M. Pavlović, Aleksandra M. Milović, Gordana G. Ocić (Institute of Neurology, Belgrade, Serbia)
Background: Constructional praxia can be impaired by several mechanisms. We examined the impact of impairment of executive functions on constructional activity in two dimensions in patients with TBI. Methods: We examined 41 patients with moderate and severe closed traumatic brain injury, 11 (26.83%) with right hemisphere lesion, 12 (29.27%) with left hemisphere lesion, and 18 (43.90%) with bilateral lesions according to computerized scan findings. Patients were tested with WCST and copy format of Rey Complex Figure (RCF). Results: Copy score of RCF was 30.63 in left hemisphere lesion group, 28.68 in right hemisphere lesion group, and 27.39 in bilateral lesions group. Left hemisphere group patients were better in WCST perseverative responses and categories than the right hemisphere group. Patients with bilateral lesions were the worst on all measures. Conclusions: Patients with right hemisphere lesions have more constructional apraxia and executive dysfunctions than those with left hemisphere lesions, but less than patients with bilateral lesions. This pattern may reflect the impact of executive functions on constructional activity in two-dimensional tasks.
P89. “My baby—myself”: dynamics of change and integration in the primipara mother after severe traumatic brain injuryEsther Klag, Yigal Gross, Shaul Schreiber (Department of Psychology, The Hebrew University of Jerusalem, Israel)
Background: Disruptions in self-concept are often among the sequelae of traumatic brain injury. The gradual process of integrating a whole sense of self during cognitive and emotional rehabilitation has been described by some clients as “giving birth to myself.” Methods: We report the case of a 28-year-old woman who some years earlier had suffered severe brain injury with consequent cognitive deficits, severe emotional disturbance, and regressive functioning. Treatment over a 2-year period, including medication, psychotherapy, and cognitive remediation, resulted in partial alleviation of symptoms and very modest achievements. The client, who had married her boyfriend shortly after her injury, then became pregnant. Medication was withdrawn for the first trimester and mild dosage prescribed for the remaining months. Supportive therapy was maintained. Results: Although the birth itself was a difficult one, the client reported satisfaction that “at last, my body is doing something right.” She demonstrated immediate bonding with the infant and became completely involved in her daughter's development. She subsequently appeared to develop cognitively and emotionally along with her daughter's developing needs. She showed marked improvement in symptoms and functioning and was able to benefit significantly from further therapy. The improvement has been consistently maintained. Conclusions: A situation fraught with anxiety for the female patient seems to offer a chance for growth and integration, in addition to fulfilling a need. Questions are raised about intervention and counseling needs, ethical issues, value systems, and family support.
P90. Possible beneficial effect of risperidone on REM sleep disturbance following traumatic brain injuryShaul Schreiber, Esther Klag, Yigal Gross, Chaim G. Pick (Department of Psychiatry C, The Chaim Sheba Medical Center, Tel-Hashomer, Israel)
Background: Severe disturbances of sleep architecture and circadian rhythms are common in traumatic brain injury patients; however, complete absence of the rapid eye movement (REM) sleep stage is very rare. Methods: We report the case of a 63-year-old man who suffered severe brain injury with consequent cognitive deficits, paranoid delusions, and depressed mood. He further suffered from insomnia characterized by extremely disturbed polysomnographic patterns, including no REM sleep. Following several trials with conventional antipsychotics, his psychotic state stabilized; however, he continued to complain of insomnia and daytime fatigue, and on repeated polysomnographic evaluation he continued to have no REM sleep. Results: Four weeks after risperidone treatment (2 mg/day) was instituted, the patient reported a reduction in psychotic symptoms, an improvement of insomnia, and waking up in the mornings with the sensation of having dreamed vividly; his daytime alertness increased. Conclusions: Total or near total absence of REM sleep is associated with severe brain damage, a condition thought to be a nonreversible. The possible restoration of dream-sleep following treatment with risperidone may be a unique finding that needs both further evaluation and interpretation.
P91. Lack of gender difference in mood and anxiety disorders after traumatic brain injuryDeborah L. Warden, Mary Rosner, Mary Coyle, Elisabeth Moy Martin, Sharon Woods, Saeed Ahmed, Dan Kowler, Angela Drake, Andres Salazar (Walter Reed Army Medical Center, Washington, DC)
Background: Males are at greater risk of sustaining TBI, although military females have a risk equivalent to that of civilian males (Ommaya et al., J Trauma 1996; 40:211–217). This study was undertaken to determine if incidence of post-TBI psychopathology is different between genders. Methods: 17 head-injured females and 21 males (matched for age, race, education, time from injury, and severity of injury) who were evaluated in the Defense and Veterans Head Injury Program were studied. The incidence of DSM-IV mood disorder due to TBI-major depressive type (MD) and anxiety disorder due to TBI-generalized anxiety type (GA) was computed on the basis of symptoms reported during an interview using the Present State Examination. The criterion for anxiety disorder due to GA in this study was fulfilling DSM-IV criteria for generalized anxiety disorder. Results: Mood disorder due to TBI-MD and anxiety disorder due to TBI-GA were equally represented (females: 29%, 12%; males: 33%, 9%; Fisher's exact test, P=0.54, 0.61, respectively). Total number of DSM-IV depressive symptoms and total 18-item Ham-D scores were not significantly different. Conclusions: Diagnoses of mood disorder due to TBI-MD and anxiety disorder due to TBI-GA occurred with equal frequency in this sample of head-injured patients.
Neuroimaging and Electroencephalography
P92. MRI volumes of amygdala and hippocampus in non–mentally retarded autistic adolescents and adultsElizabeth H. Aylward, Nancy J. Minshew, Gerald Goldstein (University of Washington, Seattle, WA)
Background: Neuropathologic studies of autism have found decreased neuronal size, increased cell packing density, and decreased complexity of dendritic arbors in hippocampus, amygdala, and other limbic structures (Bauman, J Autism Dev Disord 1994; 26:199–203; Raymond et al., Acta Neuropathol 1996; 91:117–119). Methods: Volumes of hippocampus, amygdala, and total brain were measured on 1.5-mm MRI scans from 14 non–mentally retarded autistic male adolescents and young adults and 14 individually matched healthy community volunteers. Results: Amygdala volume was significantly smaller in the autistic subjects, both with (P=0.006) and without (P=0.01) correcting for total brain volume. Total brain volume and absolute hippocampal volume did not differ significantly between groups, but hippocampal volume, when corrected for total brain volume, was significantly reduced (P=0.04) in the autistic subjects. Conclusions: These findings provide evidence in autism of a reduction in the volume of amygdala and hippocampus, particularly relative total brain volume. The histopathology reported for autism suggests that this volume reduction is related to a reduction in the neuropil, which, in turn, may suggest a reduction in neural connections between limbic structures and other parts of the brain. Support from NINDS Grant NS33355 and the Department of Veterans Affairs.
P93. The left intraparietal sulcus as the generator of conceptual praxis: an fMRI task subtraction studyJ. Moll, R. Oliveira-Souza, F. C. Souza-Lima, P. A. Andreiuolo (LABS, UNI-Rio, and UFRJ, Rio de Janeiro, Brazil)
Background: Apraxia has been classically assigned to damage of the inferior parietal lobule of the dominant hemisphere. It is still debated, however, where in the brain the idea of a transitive action is born. In the present study, we investigated tool use behavior of normal subjects with fMRI. Methods: Eight normal adults were asked to pantomime the use of 18 tools and utensils with each hand. The control task consisted of a complex sequence of overlearned, meaningless hand movements. A complete study of activation control was done for each hand. Dynamic T2* echo-planar images were acquired with a 1.5-T scanner through 10 oblique planes during 8 alternating task and control periods. Activation maps were generated by cross-correlation analysis. Results: The left intraparietal sulcus was the only area activated in every subject regardless of the hand used. Correlations between stimulus and signal were highest in the intraparietal sulcus (P<0.001). The inferior parietal lobule was not predictably activated in our sample. Conclusions: The dominant intraparietal sulcus area may be essential for the genesis of actions mediated by tools and utensils. Ideational apraxia may result from lesions a) of the intraparietal sulcus region in the occipitoparietal transition or b) in the white matter underlying the cortex of the caudal inferior parietal lobule, where projections of the intraparietal sulcus are conveyed to the rostral forebrain by the superior longitudinal fasciculus.
P94. Cerebellar correlates of the Stroop Color-Word Test (SCWT) and Continuous Performance Test (CPT) in healthy volunteersDavid E. Fleck, Melissa P. DelBello, Molly E. Zimmerman, Kenji W. Sax, Stephen M. Strakowski (University of Cincinnati, Cincinnati, OH)
Background: Recent functional MRI studies reveal cerebellar activation on tests of selective attention (Le et al., J Neurophysiol 1998; 79:1535–1548; Allen et al., Science 1997; 275:1940–1943), but there have been no investigations examining associations between cerebellar neuroanatomy and specific neurocognitive components of attention. Methods: 12 healthy volunteers were imaged with a 1.5-T MRI scanner. The SCWT and CPT were used to measure two distinct aspects of attention: resistance to interference and sustained attention, respectively. Morphometric measurements were obtained for prefrontal cortex, caudate, thalamus, and hippocampus, structures previously associated with attention (Strakowski et al., submitted), plus cerebellar vermis (DelBello et al., submitted). Results: The SCWT was significantly correlated with cerebellar vermal area V2 (r=0.98, P<0.05) and the CPT was correlated with area V3 (r=–0.82, P<0.05). Both tests were marginally correlated with prefrontal cortex (r=0.73 and –0.80, respectively, P<0.10). Conclusions: Resistance to attentional interference may be associated with the posterior lobe of the cerebellar vermis, whereas sustained attention appears to be associated with the posterior and flocculonodular lobes. These preliminary results may be relevant to studies of morphometric abnormalities in patients who suffer from psychiatric illness with attention deficits and distractibility (e.g., Sax et al., Am J Psychiatry; in press).
P95. Effect of hydration on MRI brain volumesBeng-Choon Ho, Susan Schultz, Kathleen Travis, Nancy C. Andreasen (MHCRC, Department of Psychiatry, University of Iowa, Iowa City, IA)
Background: A substantial proportion of patients with chronic schizophrenia are polydipsic. Although gender, parental socioeconomic status, total brain volume, and nutritional state are known potential confounding factors in quantitative MRI studies, the effects of polydipsia on brain volumes are unknown. This study examines whether hydrational state affects brain volumes among schizophrenic patients with polydipsia. Methods: 14 polydipsic subjects with DSM-IV schizophrenia underwent 48 hours of fluid restriction (<3 liters/day). Brain volumes were measured by using MRI scans obtained before and after fluid restriction. Results: 4 subjects did not complete the study because they could not tolerate fluid restriction. 1 subject was excluded from the analyses because of extreme changes in brain volumes, possibly due to previous frontal lobotomy. During fluid restriction, the remaining 9 subjects consumed a mean of 2.1 liters less fluid (SE=0.87). When subjects were allowed fluids ad lib, total brain volume increased by a mean of 3.3 cc (SE=4.0), total intracranial CSF volume decreased by 1.6 cc (SE=3.2), and the mean difference in ventricular volume was zero (SE=0.3). These differences were not statistically significant (t=0.83, –0.51, and –0.18, respectively; P>0.39). Conclusions: The volume of fluid intake preceding MR imaging does not significantly affect volumetric measurements of tissue and CSF among schizophrenic patients with polydipsia. These preliminary findings suggest that quantitative MRI studies need not covary for fluid intake differences.Support from NARSAD, NIMH, and the Nellie Ball Trust Fund.
P96. fMRI demonstration of distant translocation of complex cortical functions in patients with arteriovenous malformationsC. David Hunt, Gabriela Höhn, Gudrun Lange (UMDNJ-New Jersey Medical School, Newark, NJ)
Background: Translocation of language and other functions has been shown in the literature on neuronal plasticity. Cortical lesions such as arteriovenous malformations (AVMs) can alter functional localization, either during development or subsequently by ischemic dysfunction from vascular steal or ablations secondary to hemorrhage. Others have noted receptive language functions in unexpected areas. Short-term influences on cortical organization following modification of sensory input have also been shown, as well as delayed translocation of some language skills under conditions of brain disease. Methods: Multimodal functional investigations of patients with AVMs were performed for preoperative planning, including neuropsychological assessment and fMRI evaluations of selected speech and motor functions. Results: As expected, some cortical functions are locally displaced by the pathological lesions. Of distinct interest is the frequent translocation of fMRI activation to distant regions, not routinely normally activated, that are functionally rather than structurally related to the activity expected in the pathologically involved sites. Conclusions: Displacement of motor and language functions is not merely anatomic but also functional, implying adaptation by meta-organizational plasticity in the presence of some AVMs. This finding is consistent with others' demonstrations of somatotropic modifiability. It is also consistent with the hypothesis of the unmasking of functionally organized silent cortical connections.
P97. An anatomical method using external markers for the use of repetitive magnetic stimulation (rTMS)Facundo F. Manes, Jeremy Bockholt, James Bailey, Robert G. Robinson (Department of Psychiatry, University of Iowa College of Medicine, Iowa City, IA)
Background: Left dorsolateral prefrontal cortex (area 46) stimulation with rTMS can potentially treat depression. Studies are warranted that use MRI-guided anatomical localization of stimulation site to control for differences in brain morphology and skull size. Methods: A swim cap was placed on the patient's head by using reference points. Vitamin E capsules were glued to the cap at the F3 point in relation to International 10-20 System (point A) and at the point of maximum stimulation of the right abductor pollicis brevis muscle (point B). The subjects then had structural 3D MRI scans. On the basis of the 3D reconstruction, we identified area 46 in Talairach coordinates and calculated the “skull area 46” point and its distance from points A and B. Results: We have identified the skull area 46 point and its distance from points A and B in 9 subjects. Intrarater and interrater reliability for identifying the two measured distances to area 46 was high (intraclass correlations 0.95 and 0.99, respectively). The average distance to the skull area 46 from point A was 14.3 mm posterior and 5.1 mm above; the average distance from point B was 5.2 cm anterior. Conclusions: This method offers an objective means of identifying a specific cortical site for rTMS stimulation. It is hoped that site-specific stimulation will lead to more consistent therapeutic response.
P98. Are the boundaries of normal analog EEG well defined?Hugh A. Mirolo, Nashaat Boutros (Department of Psychiatry, Yale University, New Haven, CT)
Background: The unquantified analog EEG remains the sole technique that can detect cerebral epileptiform discharges. The analog EEG is also capable of detecting significant focal slowing that is indicative of structural abnormalities and generalized slowing that is indicative of diffuse pathology. In order for this technique to be reliable, the boundaries of normality should be well defined. Methods: We reviewed the world literature to ascertain whether or not studies that define the boundaries of normal analog EEG can be considered adequate for neuropsychiatric purposes. We found 56 articles addressing normal EEGs as controls for psychiatric studies, from 1936 until the present. We established the criteria for normality to be followed as a standard, and the Methods section of each paper was critically examined to see if those criteria were met. Results: After review of the studies it becomes evident that the criteria for normality taken into consideration in the world literature for “normal” analog EEG range from poor to absent. The neuropsychiatric history of the subjects was disregarded in the majority of studies. Conclusions: We conclude that in neuropsychiatry, the boundaries for normal analog EEG are poorly defined. To make it possible to better define and study analog EEG abnormalities in neuropsychiatric populations, well-designed normative studies are needed.
P99. Use of statistical parametric mapping in evaluation of 18FDG PET scans ordered for clinical workup of neuropsychiatric syndromesWilliam E. Ottowitz, Edward Kovalik, Mark M. Mandelkern, Charles Brown, Barbara Swartz (Brown University, Providence, RI)
Background: Conventional visual analysis of an 18FDG PET scan is evaluator dependent and is therefore a subjective process. Thus, it is important to evaluate how frequently scan interpretations differ and to consider alternatives to simple visual analysis. Research methodologies frequently use statistical parametric mapping (SPM) to evaluate differences between scans. Preliminary investigation (Swartz et al., Neurology 1998; 50:A192–A193) suggests that this tool is also effective in the evaluation of scans ordered for the clinical workup of epilepsy. This application deserves investigation for other neuropsychiatric syndromes, such as dementia. Methods: Two nuclear medicine physicians evaluated PET scans from 50 dementia cases while blinded to each other's interpretations. Agreement between their interpretations was evaluated by kappa analysis. The 50 scans were then compared with a normal database by using SPM. Results: Kappa analysis demonstrated a 0.52 agreement between the interpretations of the two nuclear medicine physicians. This is considered fair. Approximately 85% of the dementia scans lent themselves to analysis by SPM. Our most frequent problem was poor alignment of the patient in the scanner. Conclusions: Simple visual analysis of PET scans may not offer high interrater reliability. SPM, typically used in research, offers a quantitative alternative for clinical use.
P100. FLAIR is more sensitive than proton density weighting for visualizing and measuring subcortical hyperintensities in geriatric hypertensive patientsStephen Salloway, Melissa Jenkins, Jorge Intal, Debbie Javorsky, Paul Malloy (Brown University, Providence, RI)
Background: Proton density (PD)-weighted images have been used to measure subcortical hyperintensities (SH) in MRI studies because of good contrast between the bright SH and dark CSF. Recently introduced fluid-attenuated inversion recovery (FLAIR) methodology is superior for visualizing some subcortical abnormalities, such as multiple sclerosis lesions. Methods: Hypertension clinic patients ages 60 to 80 (N=7) completed an MRI protocol in which both FLAIR and PD-weighted images were obtained (Siemens 1.5 T, FLAIR TR=9,000, TE=105, TI=2,500; PD TR=2,500, TE=15, 4 mm, skip 0 axial slices). Three periventricular axial cuts were quantified by two trained raters using semiautomated methods. Results: SH were easier to visualize and quantify on the FLAIR images. A significantly greater amount of SH was detected on FLAIR images (mean 649 mm2) versus PD (mean 369 mm2, P<0.04). Greater contrast was seen between the brightness of SH and ventricles (P<0.02) and SH and normal white matter (P<0.01) on FLAIR than on PD images. An average of 9.7 lesions per FLAIR axial slice and 6.5 per PD slice were detected (P=0.13). Conclusions: SH appeared brighter, lesion area was greater, and there was increased contrast ratio between lesions and surrounding white matter and CSF on FLAIR compared with PD. FLAIR images should be considered for use in clinical and research scans for the evaluation of SH.
P101. Changes in regional brain function on recovery from depression: relationship with specific clinical dimensionKengo Shimoda, Mahito Kimura, Amane Tateno, Takao Mori, Hiroko Suzuki, Shunkichi Endo (Nippon Medical School, Tokyo, Japan)
Background: Functional neuroimaging studies of depressed patients have reported that significant decreases in regional cerebral blood flow (rCBF) were confined to the frontal cortex, basal ganglia, and inferior anterior cingulate cortex. Event-related potential (ERP) studies of depressed patients have also shown a significant decrease of P300 amplitude. Although state changes in regional brain function were confirmed by many previous studies of depression, only a few studies examined the influence of specific clinical dimension of depression on changes in regional brain function. Methods: Subjects included 15 patients who met DSM-IV criteria for major depressive disorder with melancholic features. 123I-IMP SPECT and EEG were performed when the patients were ill and after recovery. Subjects were divided according to predominant clinical dimension into a psychomotor agitation/anxiety group and a psychomotor retardation group by using dimensions of the Ham-D score. Results: The predominant clinical dimension, but not state changes, significantly affected rCBF in left prefrontal cortex and left basal ganglia. The specific clinical dimension also significantly affected P300 amplitude. Conclusions: These data suggest that the predominant clinical dimension plays an important role in the changes in regional brain function in depressed patients. These data also suggest that anxious depression and psychomotor retarded depression may be based on different mechanisms.
P102. Four cases of leukodystrophy: correlation between clinical symptoms and neuroimagingChiharu Tamagaki, Akira Murata, Akemi Saito, Gaku Okugawa, Tetsuji Sakata, Tokio Ohara, Toshihiko Kinoshita (Kansai Medical University, Osaka, Japan)
Background: Leukodystrophy is one of the most important syndromes of white matter dementia (Merrian et al., Neuropsychiatry Neuropsychol Behav Neurol 1990; 3:217–235). The salient neurobehavioral deficit of white matter dementia is attentional dysfunction (Filly et al., Neuropsychiatry Neuropsychol Behav Neurol 1988; 1:239–254). However, there are few reports of correlation between clinical symptoms and MR images and SPECT. Methods: Subjects included 4 cases of leukodystrophy, comprising 2 adult-onset adrenoleukodystrophy (ALD) and 2 adult-type metachromatic leukodystrophy (MLD) cases. All subjects were examined by MR imaging and SPECT. Their clinical symptoms were also observed. Results: T2-weighted MR images of the 4 cases showed high intensity in cerebral white matter. This spread in an inner-outward fashion and progressed in a rostrocaudal manner. In their initial stage, SPECT of ALD patients showed no abnormal findings and SPECT of MLD patients showed mild reduction in the regional cerebral blood flow (rCBF) of frontal lobe. Reduction of rCBF spread to cerebral cortex after change of MR images. Conclusions: The discrepancy between MR images and SPECT findings in their initial stages was characteristic. It means that clinical symptoms of leukodystrophy are attributable to cerebral white matter degeneration.
P103. Late-onset paranoid psychosis as a separate clinicopathological entity: clinical and MRI dataJoseph Tonkonogy (University of Massachusetts Medical Center, Worcester, MA)
Background: Late-onset paranoid psychosis (LOPP) has long been accepted as a late-onset schizophrenia or schizophrenia-like psychosis. Head CT and MRI findings of white matter lesions have been recently described in cases with LOPP, but no results of direct comparison between LOPP and age-matched group of elderly patients with early-onset schizophrenia have been reported. Methods: Subjects included 15 patients with LOPP, mean age 66.33 years, and 35 elderly patients with early-onset paranoid schizophrenia (PSCH), mean age 63.89. Clinical evaluation and MRI studies were done for all 50 patients. Results: As was found in previous studies, delusions and hallucinations were observed in both groups of patients. Patients with LOPP differed from the PSCH group by the mild degree or absence of negative symptoms, the absence of formal thought disorders, and the prevalence of female patients. MRI data revealed statistically significant differences between the two groups of patients. White matter hyperintensity was almost threefold more frequent in LOPP than in PSCH (66.6% vs. 22.9%). At the same time, ventricular enlargement and cortical atrophy were more frequent in the PSCH group, with moderate to severe abnormalities (22.9% for ventricular enlargement and 28.6% for cortical atrophy in the PSCH group), while prominent abnormalities were absent in LOPP group. Conclusions: Clinical features and MRI data differ in patients with late-onset paranoid psychosis and elderly patients with early onset of paranoid schizophrenia, pointing to the possibility that LOPP is a separate clinicopathological entity with white matter lesions underlying its development in a significant percentage of cases. The vascular origin of white matter lesions in LOPP will be discussed.
Neuropsychology and Cognitive Neuroscience
P104. Neuropsychological differentiation of Alzheimer's disease and depressionSoh-Yeon Ahn, Ji-Hae Kim, Doh-Kwan Kim (Samsung Medical Center, Seoul, Korea)
Background: The purposes of the present study were 1) to compare Alzheimer's disease patients with depressed patients in neuropsychological function and 2) to investigate the accuracy of neuropsychological tests in distinguishing AD and depression. Methods: The neuropsychological testing of 12 AD patients was compared with that of 12 elderly depressed patients, controlled by age, education, and level of MMSE score. Results: AD patients performed significantly worse than depressed patients in the Korean Boston Naming Test (K-BNT), false positive error and discrimination index of Korean Hopkins Verbal Learning Test (K-HVLT), contrasting program, go/no-go test, alternating hand movement, and fist-edge-palm task, but not in Rey-Osterrieth Complex Figure Test. Several tests clearly differentiated between AD and depressed patients, including K-BNT, go/no-go test, and alternating hand movement task. Sensitivity and specificity were 91.7% and 91.7% for considering these three variables simultaneously. Conclusions: AD patients showed more deficit in confrontational naming ability and frontal lobe function. Neuropsychological tests to evaluate these functions were highly sensitive and specific in distinguishing AD from depression.
P105. Comparative memory performance in multiple sclerosis patientsRicardo F. Allegri, Marina Drake, Adriana Carra (Department of Neurology, Buenos Aires British Hospital, Argentina)
Background: The presence of cognitive impairment during the course of multiple sclerosis has been recognized since Charcot's description in 1868, but the profile of memory impairment has been described more recently. The aim of our study was to investigate memory deficits in MS patients, analyzing the particular profile considering the episodic and semantic memory performance. Methods: 30 patients with MS and 25 normal subjects matched for age and educational level were evaluated. As part of a wider neuropsychological evaluation, the episodic memory assessment consisted of a modified version of Signoret's protocol (logic memory, immediate and delayed; serial learning of a list of 12 words; delayed free recall of the list; semantic cued recall; recognition trial; and digit span forward and backward). As measures of semantic memory, we used the Boston Naming Test and a task of verbal fluency. Patients were classified by disease type as relapsing-remitting, secondary progressive, or primary progressive. Results: MS patients performed worse in serial learning and serial recall tasks than control subjects. In the recognition trial as well as in tests of semantic memory, the two groups showed similar results. Conclusions: The memory performance pattern found in our patients correlates with that described in the literature (Coolidge et al., Arch Clin Neuropsychol 1996; 11:605–611) and matches the subcortical type.
P106. Differences between burden and personality traits among caregivers of demented and aphasic patientsRicardo F. Allegri, Carlos A. Mangone, Raúl L. Arizaga, Juan A. Ollari, Fernando Taragano, Ana De Pascale, Denisse Baumann, Claudio Goscilo, Paula Harris (Department of Neurology, University of Buenos Aires, Argentina)
Background: Dementia is a progressive global cognitive decline. Vascular aphasia is a nonprogressive focal communicative disorder. The two syndromes generate different levels of caregiver burden. In this study, our objectives were 1) to study the caregiver's burden in both syndromes; 2) to define the caregiver's personality profile; and 3) to correlate the personality profile with the risk of developing high burden. Methods: A modified version of the NEO FFI (five-factor inventory for personality profiles: neuroticism, extraversion, openness, agreeableness, and conscientiousness) was administered to 53 caregivers of demented patients and 18 caregivers of severe aphasic patients. Index of caregiver's burden (ICB) was assessed with the Zarit burden interview. Nonparametric tests were used to study statistical differences among groups and their correlation. Results: Impairments in instrumental activities of daily living (Spearman rank correlation coefficients, S=0.74, P<0.01) and behavioral problems were correlated with ICB for dementia, and severity of aphasia was correlated with ICB for aphasia (0.534, P<0.05). ICB of demented patients had a positive correlation with neuroticism (0.35, P=0.01) and openness (0.31, P<0.05) and a trend for a negative correlation with agreeableness (0.18, P<0.001). Conclusions: Although these two diseases are quite different, the personality profiles of those caregivers at risk for presenting high burden are quite similar. These results strengthen the need for a regular assessment of the personality profiles in these caregivers for preventive purposes.
P107. Roles of the amygdala, prefrontal cortex, and right somatosensory/insular cortex in decision making and emotional processingAntoine Bechara, Daniel Tranel, Andrea Hindes (University of Iowa, Iowa City, IA)
Background: The somatic marker hypothesis proposes that the amygdala (A), the ventromedial prefrontal cortex (VM), and the right somatosensory/insular cortex (RSS/I) are components of a neural system subserving decision making and emotional processing. Here, we investigated whether the three structures provide similar or different contributions to the process. Methods: We used the Gambling Task, a well-established paradigm that measures decision-making performance, and electrodermal activity as an index of somatic state activation in normal control subjects (n=6) and in subjects with bilateral A (n=5), VM (n=5), or unilateral RSS/I (n=4) lesions. We also tested the same subjects in a fear conditioning experiment, using four different colors of monochrome slides as conditioned stimuli and a startlingly loud sound as the unconditioned stimulus. Electrodermal activity (SCR) was the dependent measure of autonomic conditioning. Results: Compared with control subjects, all A, VM, and RSS/I subjects were 1) impaired on the Gambling Task and 2) unable to develop anticipatory SCR while they pondered risky choices. All control, VM, and RSS/I subjects acquired the conditioning, but the A subjects failed to do so. In related experiments, we found that VM and A subjects were able to imagine and reexperience a previous emotional situation but RSS/I subjects were unable to do so. Conclusions: Disruption of emotional functioning interferes with decision making. The A is necessary for acquiring conditioned emotional responses, but not for the retrieval of the emotion of an experience. By contrast, the RSS/I is not necessary for acquiring conditioned emotional responses, but it is important for reconstructing the emotion associated with a previous experience. The VM is essential for coupling complex stimulus configurations with appropriate somatic states and for the use of these emotional signals in guiding decisions.Support from NINDS Grant P01 NS19632.
P108. Separating the cognitive effects of epilepsy and antiepileptic drugs: a quasi-experimental studyJenn-Yeu Chen, Jing-Jane Tsai (National Chung-Cheng University, Chia-Yi, Taiwan)
Background: The question of whether epilepsy and/or antiepileptic drugs (AEDs) can cause adverse effects on patients' cognitive functioning has not been answered satisfactorily because the two factors were often confounded in the previous research. The present study attempted to separate these two factors to provide a more definitive answer. Methods: Three adult patient groups and one normal control group (n=15 each) were examined twice on a set of attention, memory, and reaction time tests. The On-Off group were tested once when they were on AEDs and a second time when AEDs were completely withdrawn. The On-On group were tested when they were on AEDs on both occasions. The Off-On group were fresh patients who were tested once before receiving any AEDs and a second time when they were put on AEDs. The four groups were matched as much as possible on several demographic and clinical variables. Results: There were no reliable differences among the groups on any of the cognitive tests. Conclusions: Contrary to the view held by a number of authors who had reviewed the research in this field, our findings showed that neither epilepsy nor antiepileptic drugs had any adverse effects on the cognitive functioning of the epileptic patients. This conclusion is consistent with the recent findings on children by Aldenkamp and colleagues (Aldenkamp et al., Neurology 1993; 43:41–50; Vermeulen & Aldenkamp, Epilepsy Res 1995; 22:65–95).Support from the National Science Council of the Republic of China.
P109. Impairment of attentional set-shifting in patients with Parkinson's diseaseAnne W. Justus, Peter G. Como, David Song, Roger Kurlan, Suzanne N. Haber (University of Rochester Medical Center, Rochester, NY)
Background: Cognitive dysfunction in Parkinson's disease is related to impairment of the frontostriatal system, contributing to deficits in working memory, attention set-shifting, and organization/planning, contributing to a so-called subcortical-frontal dementia. This specificity of cognitive impairment in PD may be related to decreased dopamine (DA) transport to limbic and frontal regions and/or impaired DA receptor activity in the frontal lobes. This study used the Cambridge Neuropsychological Test Automated Batteries (CANTAB), which can be administered to both humans and nonhuman primates to assess for evidence of impairment in attentional set-shifting, which is believed to be among the early indicators of cognitive dysfunction in PD. The ultimate goal is to develop an animal model of early cognitive changes in PD that may be associated with DA dysfunction. Methods: Subjects included 23 PD patients (17 males, 6 females) with a mean age of 64±12 yr. Mean duration of PD was 9.3±6.6 yr. Mean Hoehn and Yahr PD stage was 2.3±0.6, corresponding to mild disease. Mean education was 15±3 yr. Estimate of premorbid IQ using a standardized reading test was 110±11. The PD patients were administered the intra/extradimensional (ID/ED) set-shifting task from the CANTAB. This task involves shifting attention from a previously relevant dimension (i.e., shapes) to the previously irrelevant dimension (i.e., lines). Results: PD patients had difficulty completing the set-shifting task, with mean performance at the 25th percentile compared with normative data. 8/23 patients (35%) also had difficulty completing the ID/ED shift, which was independent of PD stage. Conclusions: These results suggest that evidence of a cognitive deficit may be detected in attentional set-shifting tasks in patients with early PD who do not otherwise show evidence of substantial cognitive impairment. These tests may be useful in developing an animal model of early DA dysfunction and subsequent cognitive changes in PD. Pilot studies are currently under way in nonhuman primates, using a comparable version of CANTAB.Support from the National Parkinson's Disease Foundation Center of Excellence.
P110. Extraversion and the stability of P300 amplitudeJorge H. Daruna (Tulane University School of Medicine, New Orleans, LA)
Background: P300 amplitude variation across individuals has been found to reflect personality traits such as introversion-extraversion (Daruna et al., Biol Psychol 1985; 20:249–259). Typically, introverts are found to have larger amplitude P300s. This has been attributed to the better ability of introverts to sustain arousal over time. Methods: Subjects (N=13) were healthy young adults (21–24 years of age). During sessions conducted 2 to 3 months apart, they performed a visual choice reaction time task requiring a spatial orientation judgment. Event-related potentials were computed from artifact-free trials. P300 was defined as the maximum positive point beyond 250 ms. An overall amplitude measure was computed for each session by summing the P300 amplitudes at Fz, Cz, and Pz. P300 amplitude change between sessions and the subjects' score on the introversion-extraversion scale on the Eysenck Personality Questionnaire–Revised were correlated. Results: There was a significant decrease in P300 amplitude between sessions conducted 2 to 3 months apart. The magnitude of the change was significantly related (r=0.702, P=0.008) to the subjects' extraversion score. P300 amplitude decreased more for the extraverts. Conclusions: These findings further underscore the role of extraversion in modulating the P300 amplitude, most likely due to changes in arousal over time and with experience. Support from NIAAA Grant AA07548.
P111. Neuropsychological assessment of mild brain injury and recovery of function in college athletesRuben J. Echemendia, R. Scott Mackin, Laura Julian, Kevin Kachin, Naomi Shoss, Cathy Elsinger (Pennsylvania State University, University Park, PA)
Background: Cerebral concussions or mild head injuries are common in athletic competition at all levels. A frequent concern for those who care for these athletes is when to safely return the athlete to sport. Traditional radiologic techniques generally have not been very useful in this decision. The Penn State Concussion Program was developed as a prospective neuropsychological study of men and women college athletes. Data from injured athletes are compared with preinjury data obtained from pre-participation neuropsychological screening in order to assist in the return-to-play decision. Methods: Approximately 425 athletes from sports at risk for concussion (ice hockey, football, soccer, basketball) and those not at risk (swimming, tennis, baseball) were administered a neuropsychological screening battery. Approximately 30 athletes sustained concussions ranging from mild (momentary disorientation with headache) to severe (loss of consciousness). Injured athletes were assessed serially at 2 hours, 48 hours, 1 week, and 1 month postinjury. Results: Postinjury neuropsychological test data demonstrate significant declines from baseline data. Recovery of neurocognitive functions is generally complete within 10 days of injury. Conclusions: Neuropsychological baseline screening is useful in detecting the neurocognitive changes that occur after cerebral concussion. Prospective data allow for the examination of recovery of function following concussion.
P112. The cerebellum and cognition: familial cerebellar degeneration with dementiaLisa M. Bateman, Dean J. Foti (University of British Columbia, Vancouver, BC, Canada)
Background: The cerebellum has been regarded mostly as a structure for motor control. However, recent studies have been recognizing that the cerebellum may play an important role in cognition, especially in executive functions. A unique family with autosomal dominant cerebellar degeneration with dementia is presented to highlight the potential role of the cerebellum in cognition. Methods: 11 family members over 3 generations were subjected to neurobehavioral examination, and affected members received SPECT and CT/MRI imaging. Literature review of cerebellar degenerations and cerebellar-cognitive processing was conducted. Results: 4 of the 11 family members were clinically affected, having prominent frontal subcortical dysfunction, memory retrieval deficits, and behavioral disturbances with disinhibition. 3 of the 4 affected patients showed marked cerebellar atrophy on imaging, and 2 of these 3 showed cerebellar hypoperfusion with normal or increased parasaggital cortical perfusion. The patient with normal imaging is young and early in her course. Testing for SCA 1,2,3 mutations was negative. No similar family with autosomal dominant cerebellar degeneration has been described; milder cognitive deficits are usually found. Conclusions: The cerebellum may play an integral role in cognition, likely through the loss of cerebellar-cortical inhibitory pathways. This unique family highlights the role the cerebellum may play in learning, behavior, and executive function. Neuropathological confirmation will further clarify the anatomic substrate of dementia in this family.
P113. Cognitive and motor deficits in presymptomatic individuals genetically positive for Huntington's diseaseDaniel L. Gripshover, Meribeth Jones, Pat Allinson, Madaline Harrison, Amy Alderson, Carol Manning (University of Virginia Health Sciences Center, Charlottesville, VA)
Background: Individuals symptomatic for Huntington's disease often evidence early impairments in complex visuomotor tracking, verbal fluency, and executive functions (Grant & Adams, Neuropsychological Assessment of Neuropsychiatric Disorders, 2nd ed., Oxford UP, 1996). HD patients generally have good awareness of cognitive deficits (McGlynn & Kasniak, in Prigatano & Schacter (eds.), Awareness of Deficit After Brain Injury: Clinical and Theoretical Issues, Oxford UP, 1991) but lesser awareness of motor symptoms (Snowden et al., Arch Neurol 1998; 55:801–805). However, it is less clear if asymptomatic individuals positive for the HD gene will manifest cognitive and motor deficits on formal evaluations. Methods: Participants included 28 individuals symptomatic and gene-positive for HD, 8 individuals grossly asymptomatic and gene-positive for HD, and 19 individuals asymptomatic and gene-negative for HD. Participants were administered the Controlled Oral Word Association, Symbol Digit Modalities Test, and Stroop Test and were examined by a neurologist. Results: All groups significantly differed from each other on these three tests. On all measures, asymptomatic individuals with the HD gene were more impaired than individuals without the HD gene but less impaired than HD-symptomatic individuals. Conclusions: Asymptomatic individuals with the HD gene differed significantly on measures of verbal fluency, complex visuomotor tracking, and inhibition of habitual responses from both HD-symptomatic individuals and individuals without the HD gene.
P114. Cognitive impairment in acute and subacute strokeMichael Hoffmann, Ann Watts (Department of Neurology, University of Natal, Durban, South Africa)
Background: Our aim was to determine the frequency and extent of cognitive disorders in the acute and subacute stroke period in the indigenous population, using a battery of predefined higher cortical function tests. Methods: This was a hospital-based consecutive stroke (WHO-defined) case series in association with an acute stroke unit. A three-tier hierarchical, investigative protocol incorporating contemporary neuroinvestigative modalities was used, and all patients were evaluated with a comprehensive battery of predefined, bedside higher cortical function tests. Standardized scales for etiology, neurological deficit, clinical stroke, and disability were incorporated to quantitate neurological presentation of stroke in categories of disease, deficit, stroke subtype, and handicap. Results: Patients evaluated (N=1,100) comprised 605 men and 495 women. All patients had a CT brain scan (761; 69%), and/or an MRI brain scan (533; 48%); 37% had both. One or more higher cortical function abnormalities was detected in 60.7% of nondrowsy patients (drowsy, coma, or delirious: n=45). The most numerous categories were aphasias (25.2%), apraxias (14.5%), amnesias (11.6%), and frontal systems syndromes (9.2%). In 76 patients, neuropsychological testing (used as the gold standard) was performed, and comparison with the higher cortical function deficit (HCFD) test revealed for the latter a sensitivity of 80.2% (CI: 72%–88%) and specificity of 100%. Cognitive impairment occurred without elementary neurological deficits (motor, sensory, or visual impairment) in 137/608 (22.5%). Univariate and multivariate analyses of risk factors and likelihood of developing HCFD revealed increasing age, black race, overweight, and recent infection to be independent variables (P<0.05). HCFD did not differ significantly in younger versus older patients (P=0.194). Frontal system syndromes were more common in subcortical (32.3%) versus cortical (23.5%) lesions and were more common in younger versus older patients (P=0.001). Conclusions: 1) Cognitive disturbance is present in the majority of all types of stroke; 2) cognitive disturbance may be the sole presentation of stroke, unaccompanied by long tract signs; 3) subcortical stroke is commonly associated with cognitive impairment, usually of a frontal system; 4) risk factors for developing cognitive impairment in the indigenous stroke population included increasing age, black race, overweight body habitus, and recent infection.
P115. Cognition in first-episode maniaRobert Krikorian, Eric R. Larson, Stephen M. Strakowski, Paula K. Shear (University of Cincinnati, Cincinnati, OH)
Background: The nature of cognitive impairment and its relationship to mood disturbance and associated cerebral dysfunction are not established in bipolar disorder. Although a variety of cognitive impairments have been observed, studies using patient samples with heterogeneous mood states and variable duration of illness have contributed to inconsistent neuropsychological findings. This study assessed whether cognitive impairment is evident at the time of onset of bipolar disorder in a homogeneous sample of young patients with mania. Methods: 25 patients with bipolar I disorder, single manic episode, and 23 subjects without psychiatric disturbance were recruited. All patients and control subjects were administered the SCID-P to establish diagnoses, as well as a neuropsychological protocol that included measures of executive function, attention, and memory. Results: The subjects were high school–educated young adults. The patient group performed more poorly than the control group on all neuropsychological measures, including executive planning ability (mean=13.8 vs. 15.5), attention (mean=23.3 vs. 26.6), and memory (mean=4.5 vs. 6.1), and this was confirmed by a multivariate analysis of covariance with age and education as covariates (Wilks's lambda=0.77, P<0.02). A discriminant function analysis indicated that executive planning ability was the most discriminating measure. Conclusions: These data indicate that young patients with first-episode mania have cognitive deficits at the time of onset of the disorder, as is the case in schizophrenia. It remains to be demonstrated whether cognitive impairment persists in such patients during periods of euthymia. Although deficits were evident in a number of domains, the impairment of planning ability was the most prominent, suggesting that executive function impairment may be the fundamental cognitive deficit and may contribute to the mood disturbance as well.
P116. Pathological laughing and crying in amyotrophic lateral sclerosis (ALS): a role for the prefrontal cortex?Scott R. McCullagh, Anthony Feinstein, Marek Gawel (University of Toronto, Ontario, Canada)
Background: Pathological laughing and crying (PLC) occurs in many neurological disorders, including ALS. The etiology of the syndrome is unclear, but frontal-subcortical circuits may be involved, given their known association with mood and affect regulation. Methods: Three matched, nondemented groups were enrolled: ALS with PLC (n=10), ALS without PLC (n=6), and healthy control (n=10). They were compared on indices of orbitofrontal integrity (Gambling Task and olfactory discrimination using the University of Pennsylvania Smell Identification test), dorsolateral function (Wisconsin Card Sorting Test), global cognitive ability (MMSE, Raven's matrices), and mood (Hospital Anxiety and Depression Scale). Results: There were no significant differences among the three groups with respect to global cognitive ability, mood, olfaction, and performance on the Gambling Task. However, patients with PLC showed a trend toward making more errors, both total and perseverative, on the WCST while completing fewer categories. A similar picture, albeit weaker, emerged on the gambling and olfaction tests. A discriminant function analysis revealed that the WCST variable Total Errors correctly predicted the presence or absence of pathological affect in 70% of cases. Conclusions: PLC appears mediated, in part, by abnormalities in prefrontal-subcortical circuits. Although orbitofrontal involvement is not suggested by our data, further neuropsychological investigation of this area with a larger sample size appears warranted.
P117. Individual differences in memory and executive function abilities during normal agingSilvia Mejia, David Pineda, Lina M. Alvarez, Alfredo Ardila (University of San Beunaventura, Medellín, Colombia)
Background: The purpose of this study was to analyze the effects of some individual variables on memory and executive function test performance in normal aging individuals. Methods: 60 subjects (21 males, 39 females) with mean age of 69.66 years (SD=7.09) were selected. The following neuropsychological tests were administered: Associative Learning and Logical Memory from the WMS; Associative Memory with Semantic Enhancement Test; Wisconsin Card Sorting Test; and Verbal Fluency (Phonological and Semantic). The effects of demographic (age, education, gender) and some individual variables (academic history, working history, physical activity, and leisure activities) were measured. Results: Age and education effects on test scores were observed, but no effect of gender was found. Working history and leisure activities established significant differences in some test scores. A multiple regression analysis was performed. Conclusions: Not only demographic factors, but also individual variables have a significant effect on cognitive changes observed during normal aging.
P118. Subclinical cognitive deficits in presymptomatic Huntington's diseaseMichael H. Miller, Betty Tobia, John Holt, and Michael McCormack (Robert Wood Johnson Medical School, Piscataway, NJ)
Background: Huntington's disease is an autosomal dominant genetic disorder. Individuals begin life at a 50% risk for the illness. Preclinical identification, by the use of neuropsychological methods, of at-risk-positive individuals in whom the disease will ultimately develop has long been of interest. We have developed the Cognitive Testing Battery (CTB) for use in individuals at risk for HD as well as for individuals with symptoms. It was designed to be specifically sensitive to subtle cognitive changes in very early HD. Methods: Subjects included 98 individuals at risk for HD participating in presymptomatic genetic testing. As part of the protocol, each individual was administered psychiatric, neurological, and CTB examinations before genetic testing was performed. Spouses of at-risk persons served as further controls. Results: Presymptomatic individuals with positive gene test results showed significant and specific cognitive impairment on the CTB. In contrast, individuals with negative gene status performed the same as normal control subjects. Subtest sensitivity on the CTB highlighted frontal symptoms deficiencies consistent with early brain changes usually seen in HD. Conclusions: Patients at risk for HD, although asymptomatic, showed specific frontal symptoms deficits on cognitive testing. In contrast, normal control subjects and gene-negative patients performed normally. These findings suggest that even in clinically asymptomatic patients who show no behavioral changes, psychiatric features, or neurological signs, detection of subtle cognitive changes is possible in a carefully selected battery of cognitive tasks that allow for both qualitative and quantitative interpretation.
P119. Memory functions of the cerebellum displayed in oxygen-15 PET studiesSergio Paradiso, Nancy C. Andreasen, Daniel S. O'Leary (Department of Psychiatry, MHCRC University of Iowa, Iowa City, IA)
Background: Anatomical connectivity of the cerebellum suggests its possible implication in regulation of cognitive function (Schmahmann & Pandya, J Neurosci 1997; 17:438–458). We reviewed the results of investigations performed at our laboratory that were designed to map the circuits of human memory focusing on cerebellar activations. Methods: Five oxygen-15 PET studies in which experimental paradigms had comparable verbal output were reviewed. Areas of cerebellar activation were identified following co-registration of individual MRI and PET data (Woods et al., J Comp Assist Tomogr 1993; 17:536–546) and placement in standard coordinate space (Talairach & Tournoux; New York, Thieme, 1988). Areas of significant blood flow change were anatomically localized by using an atlas of the cerebellum (Duvenroy, 1995). Results: Study 1: Short- and long-term recognition memory of words compared with reading aloud showed increased activity in L superior and inferior semilunar lobules, L lobule simple, culmen, R superior semilunar lobule, multiple R dorsal frontal, and one L dorsal frontal region. Study 2: Novelly learned compared with well-practiced recall of words showed increased activity in the R superior semilunar lobule. Study 3: Practiced compared with novel recall of narratives showed increased activity in R superior and inferior semilunar lobule and L lobule simple, in the anterior cingulate, and in the L frontal operculum. Study 4: Recall of a personal event (episodic memory) compared with a familiar complex narrative showed increased activity in the R superior and inferior semilunar lobules and L deep cerebellar nuclei. Study 5: Comparison of facial recognition to gender categorization tasks showed increased cerebellar flow in L inferior semilunar lobule, R dorsal lateral frontal lobe, and cingulate gyrus. Conclusions: The cerebellum participates in verbal and nonverbal memory. Semantic and episodic recall predominantly activated the right cerebellar hemisphere; recognition predominantly activated the left cerebellar hemisphere. Frontal areas of increased activity are consistent with the frontal-cerebellar crossed anatomical connectivity.
P120. Multidomain cognitive impairment in depressed left temporal lobe epilepsy (TLE)Sergio Paradiso, Bruce P. Hermann, Dietrich Blumer, Robert G. Robinson (University of Iowa, Iowa City, IA)
Background: Depressed patients with left but not right hemisphere stroke show a range of cognitive difficulties (Bolla-Wilson et al., Am J Psychiatry 1989; 146:627–634). Methods: 70 consecutive surgery candidates for medication-resistant complex partial seizures of temporal lobe (TL) origin were assessed for psychiatric symptoms; intelligence; psychomotor, verbal, visual-spatial, and executive abilities; and visual and verbal memory. Unilateral TL origin was determined by closed circuit television/EEG monitoring with scalp, sphenoidal, and/or strip electrodes. Results: 24 patients (15 L, 9 R) reported depressed mood on a semistructured psychiatric interview, and 46 (32 L, 14 R) were nondepressed. Depressed patients showed higher Center for Epidemiological Studies Depression Inventory scores (mean±SD: 18.2±10 vs. 10.7±8), BDI scores (11.0±7 vs. 6±6), and MMPI D scale scores (72.4±14 vs. 61.3±14; all P<0.01). Depressed and nondepressed patients had comparable age (range 16–39 yr), sex, education, handedness, age at onset (0.5–37 yr), hippocampal sclerosis, and language dominance (sodium amobarbital test). In the L-TLE group, daily seizure frequency (DSF) was 1.65±4.4 in the depressed patients and 0.72±1.68 in the nondepressed patients (P>0.1). In the R-TLE group, DSF was 3.14±3.80 in the depressed patients and 0.23±0.25 in the nondepressed patients (P<0.05). 9 depressed patients were on phenytoin (PHE), 10 on carbamazepine (CBZ), and 2 on barbiturates. 12 nondepressed patients were on PHE, 20 on CBZ, and 1 on felbamate. 2 depressed and 8 nondepressed patients were on polytherapy. Overall, depressed patients showed lower intelligence and weaker naming, visual-spatial, and executive abilities and memory. Controlling for DSF, L-TLE depressed patients showed lower FSIQ (P=0.004), PIQ (P=0.004), and VIQ (P=0.015) and weaker performance on the Token Test (P<0.001), Naming (P=0.006), Judgment of Line Orientation (all P=0.03), Facial Recognition (all P=0.03), Trails B (P=0.03), Visual Reproduction (P=0.015), WCST categories (P<0.05), and perseverative responses (P=0.007) compared with L-TLE nondepressed control subjects. R-TLE depressed patients showed lower WMS Logical Memory percentage retained (P=0.015) and a trend for Visual lower Reproduction percentage retained (P=0.06) compared with R-TLE nondepressed control subjects. Conclusions: L-TLE depressed patients showed impairment of general intelligence, verbal, visual-spatial, and executive abilities. This confirms the association of depression, left hemisphere dysfunction, and impairment of several cognitive domains. Support from NARSAD.
P121. Persistent neuropsychological sequelae of neuroleptic malignant syndrome (NMS)James D. Petrick (ReMed Neurologic Rehabilitation, Pittsburgh, PA)
Background: Neuroleptic malignant syndrome is characterized by the sudden onset of motor rigidity, fever, autonomic instability, and altered consciousness. It is thought to result from a blockade of dopaminergic activity. Following discontinuation of the offending neuroleptic agent in conjunction with systemic supportive measures, the duration of NMS averages between 7 and 10 days. Residual brain damage is rare; however, several other important conditions that may resemble NMS must be ruled out. Methods and Results (case report): A 26-year-old African American female experienced what was believed to be an acute psychosis, treated with risperidone. She developed fever, rigidity, and headache, as well as elevated creatine phosphokinase (CPK) at 26,000, consistent with a diagnosis of NMS. She was treated with bromocriptine and dantrium. She subsequently underwent video monitor EEG and was felt to have a significant seizure disorder. She had experienced at least one episode of seizure activity, approximately 12 months prior to the onset of psychotic like symptoms, which was treated with phenytoin. Follow-up neuropsychological testing indicated profound neurocognitive impairment, persistent in nature. The clinical course of NMS is reviewed and neuropsychological data associated with this particular case are presented. The importance of careful organic/neuropsychological diagnostic assessment is discussed.
P122. Neuropsychological evaluation of bystander exposure to pesticidesRaymond M. Singer (independent practice, Santa Fe, NM, and New York, NY)
Background: There are reports in the literature of long-term neuropsychological dysfunction in persons with pesticide exposure. However, this report presents data on exposure to a person not occupationally exposed and with sudden onset of exposure. A home with open windows and a property were sprayed by helicopter with a mixture of chlorpyrifos and a carbamate (carbofuran). Three dogs on the property, fed from separate cans of food, were vomiting and listless and were diagnosed by their veterinarian with pesticide poisoning. The subject reported initial symptoms of anxiety, itching on the face which spread over her body, dizziness, and forgetfulness. She reported her sleep was frequently interrupted around 2:00 to 3:00 a.m. with symptoms of breathlessness, then numb hands and feet and a feeling of “blacking out.” She continued to reside in the home during the time when the pesticides were still potent. Her primary symptom at the time of this examination, 3 years later, was disabling chemical sensitivity, along with sleep apnea–like episodes and memory problems. She was in litigation. Methods: A physical examination that ruled out other causes of the symptoms, past medical record review, brain MRI, and neuropsychological testing were performed. Results: Brain MRI showed diffuse scattered foci of increased signal intensity in the subcortical and periventricular white matter tracts. Organophosphate pesticides are known to cause degeneration of the myelin. From normal or better functioning before exposure, declines in function included arithmetic (5th percentile), digit symbol and symbol search (9th percentile), visual memory (Benton Visual Retention Test, 11 errors), embedded figures (1st percentile), paired associates learning (1st percentile), and logical memory (1st percentile). Personality testing showed no personality disorder. Conclusions: Doctors need to be aware that pesticide exposure can lead to permanent neuropsychological deficits, even with a single exposure. Brain dysfunction from neurotoxicity can be revealed with appropriate neuropsychological testing.
P123. Observed hand preference, hand skills, and language disorders among childrenMaharaj Singh, Mandar Manjary (Ch. Charan Singh University, Meerut, UP, India)
Background: The link between handedness and learning disorders (reading and writing) has been described in terms of the slow development of the left cerebral hemisphere of the fetus. Such retardation occurs because of the high level of testosterone in utero. It has also been suggested that the slow rate of the development of left hemisphere predisposes to developmental language problems. However, others have claimed that there exists no link between handedness and language disorders. Methods: 517 elementary school children (400 normal and 117 with language disorders) were observed for 10 common hand preference activities (such as throwing a ball or using a knife). Along with the observed hand preference measures, the children of both the groups were also tested on two tasks of hand performance. In one task, the subjects were asked to fill the dots in 20 seconds using both preferred and nonpreferred hands one at a time. In the other, children were asked to move pegs as fast as possible using either hand one at a time. Results: The analysis showed that the incidence of left-handedness was 16.31% among the language-impaired children and 4.25% among the normal children. For hand skills, the language-impaired children performed poorly compared with their normal counterparts. Conclusions: The results indicate the strong possibility of the association between handedness (in terms of hand preference and hand skills) and language disorders. As suggested by the Geschwind and Galaburda (1987) model, such relationship may be mediated by the slow development of the left hemisphere. The results also indicate a lesser degree of lateralization of functions among language-impaired children. The results will be discussed in view of recent genetic and environmental theories of handedness.
P124. Neural mechanisms for relationships between emotion, memory, and decision makingDaniel Tranel, Matthew Ciorba, Daniel M. Jondle, Antoine Bechara (University of Iowa, Iowa City, IA)
Background: Emotions are known to improve memory (Cahill et al., Nature 1995; 377:295–296), and they also help guide the implementation of advantageous decisions (Damasio, Descarte's Error; New York, Grosset/Putnam, 1994). The amygdala has been shown to be a critical site for the modulation of both memory and decision making by emotion. On the other hand, the ventromedial prefrontal cortex (VM) has been shown to be a critical site for the influence of emotion on decision making, but its role in emotional memory has not been addressed. Methods: We tested normal (n=10) and VM-damaged (n=5) subjects on a memory task in which subjects were presented with a series of pictures and then tested for recall. A total of 16 pictures were presented in random order; 8 of the pictures were neutral in valance and arousal, and 8 were negative in valance and high in arousal. During learning, each picture appeared for 5 seconds on a computer screen. The stimuli were divided into four sets of four stimuli each; in each set, there were two neutral and two emotional pictures. The pictures in set 1 were presented once each; the pictures in set 2 were presented twice each; the pictures in set 3 were presented 4 times each; and the pictures in set 4 were presented 8 times each. Recall of picture content was calculated for each subject, as a function of repetition times (sets) and emotional content. Results: Normal control and VM subjects showed improvement of memory as a function of repetition, although the control subjects tended to have better overall memory scores than did the VM subjects. The most important finding, however, was that both groups were influenced by the manipulation of emotion, producing higher recall scores for pictures with emotional content. Conclusions: These results suggest that VM subjects are capable of using emotion to enhance declarative memory. Taking this together with previous findings that these subjects cannot utilize emotion to improve decisions, we suggest that the mechanism through which emotion modulates decision making is different from that through which emotion modulates declarative memory.Support from NINDS Grant P01 NS19632.
P125. Cognitive reserve and HIV-1 disease progression: the differential effects of neurologic versus psychosocial factorsSusan G. Silva, Eric D. Jackson, Kristi M. Lanning, Jane Leserman, Diana O. Perkins, Robert A. Stern, Robert N. Golden, Dwight L. Evans (University of North Carolina School of Medicine, Chapel Hill, NC)
Background: Neurologic, genetic, and experiential history can provide a cognitive reserve that influences the development and progression of symptoms in some neuropsychiatric disorders. This study examines the influence of cognitive reserve, measured by both neurologic and psychosocial history, on disease progression in HIV-1 infection. Methods: 92 initially asymptomatic HIV-seropositive gay men were studied over a 7-year period. Baseline neurologic reserve (NR) scores were derived by summing the ranks for estimated premorbid intellectual ability, degree of preexisting neurologic insult, and age. Baseline psychosocial reserve (PR) was calculated by summing the ranks for years of education, income level, and degree of social support. Disease progression was defined in three ways: as time to 1) neurocognitive decline, 2) clinical symptom advancement, and 3) immunologic decline. Results: Survival analyses, using Cox proportional hazards models, were conducted to evaluate the effects of NR and PR on disease progression. Covariates were CD4+ count, race, antiretroviral use, and depressive symptoms. Lower NR was related to more rapid progression of neurocognitive symptoms only (psychomotor slowing, P<0.05; attention deficits, P<0.05; and dexterity, P=0.04). Lower PR tended to be associated with more rapid progression of clinical symptoms (P=0.06) and immunocompromise (P=0.08). Conclusions: The results indicate that 1) neurologic history may have a greater influence on progression of neurocognitive symptoms and 2) psychosocial factors tend to influence other clinical symptoms and immunocompetence. These findings provide support for the role of cognitive reserve in protecting against or delaying the onset of HIV-related symptoms. Support from NIH Grants MH44618, MH33127, and RR00046.
P126. Neurocognitive symptoms in multiple chemical sensitivity (MCS)Susan G. Silva, Michael Hall, Kristi M. Lanning, Jane Leserman, Beth Ball, David Otto, Robert N. Golden, Howard R. Kehrl (University of North Carolina, Chapel Hill, NC)
Background: Multiple chemical sensitivity is a chronic condition in which a constellation of multiple somatic and neuropsychiatric symptoms develops in purported exposure to chemicals, usually volatile organic compounds. The purpose of this exploratory study was to characterize the nature of neurocognitive deficits observed in MCS patients. Methods: 13 individuals with MCS (11 women, 2 men) between 28 and 50 years of age were studied. Comprehensive medical, psychiatric, and neuropsychological evaluations were completed. Neuropsychological assessments included measures of attention, speed of information processing, learning/memory, and executive functioning. Participants were asymptomatic at the time of neurocognitive testing. Results: Mild to moderate attention disturbances were evident in 46% (6/13) of the patients. Selective attention and attention capacity were most affected. Executive dysfunction and memory problems were also observed in 15% of the group. When present, executive and memory dysfunction coexisted with attention deficits. All 13 participants had a history of affective disorder. Conclusions: The results indicate that MCS patients often experience significant attention problems. These findings suggest that patients with MCS may have alterations in brain circuitry involved in attention and affective processing.Support from NIH Grant MH33127 and U.S. EPA Cooperative Agreement CR817643. This abstract does not represent EPA policy.
Schizophrenia
P127. Influence of brain reserve on illness onset and remission in first-episode schizophreniaBrian Sheitman, Robert Bilder, Jose Alvir, Susan Silva, Robert Goldman, G. Reiter, Delbert Robinson, Miranda Chakos, Jeffrey Lieberman (University of North Carolina, Chapel Hill, NC)
Background: This study examined the influence of brain reserve (measured by intellectual ability) on age at illness onset and time to remission in first-episode and neuroleptic-naive schizophrenia and schizoaffective patients. Methods: 79 subjects, all without any comorbid neurological disorders, were treated by using a standardized antipsychotic medication algorithm. The Wechsler Adult Intelligence Scale–Revised was administered approximately 6 months after study entry when subjects were clinically stable. Results: Full Scale IQ scores and age at onset were not significantly related (r=0.08, P=0.50). Subgroup analyses indicated that higher FSIQ scores were associated with later age at onset in females (r=0.34, P=0.05, n=33), but not males (r=0.02, P=0.91). Survival analyses, using Cox regression models and adjusting for gender and illness duration, indicated that time to treatment response was significantly related to FSIQ (P=0.002) and Verbal IQ (P=0.001). The Vocabulary (P=0.003) and Similarities (P=0.009) subtest scores were the strongest predictors of response likelihood. Higher IQ scores predicted a more rapid treatment response. Covariate results revealed that females and patients with a shorter illness duration had a more rapid response (P<0.03). Conclusions: The concept of brain reserve appears applicable to schizophrenia. Since the relationship appears to be primarily with response to treatment, the findings suggest that the neurobiologic mechanisms underlying illness onset may differ from those responsible for treatment response. Support from NIH Grant MH33127.
P128. Perceptive organization dysfunction in schizophreniaStéphane Ertlé, Christine Rebourg (FORENAP, Rouffach, France)
Background: In this study we attempt to evaluate the quality of perceptive organization in schizophrenic patients. We analyze visual sweeping, presence or absence of a perceptive scheme (overall organization), coordination and purposeful action (overall metastructure), and capacity to recognize interactive effects between perceptual groups (overall visual information). Methods: Subjects were 30 schizophrenic patients according to DSM-IV criteria. All patients were under neuroleptic treatment. The tasks were also given to age- and sex-matched control subjects. Two tasks were used: 1) progressive enrichment of visual information and 2) image description from the Boston Diagnostic Aphasia Examination. Results: Statistically significant differences suggest an absence of perceptive strategy in these patients, as indicated by a disturbance of the overall metastructure, disorganized visual sweeping, the absence of causality linking, and the absence of a synthetic interactive and causal loop. Conclusions: Cognitive disturbances of schizophrenic patients occur within a general disturbance of action, including perceptive action, expressed in particular by disturbances of attention and of context processing. Disturbance of the organization or planning of action implies the intervention of a supervisor—a role given to the prefrontal cortex.Support from FORENAP: For Applied Neuroscience Research in Psychiatry.
P129. Do neurological abnormalities reflect brain structural indicators of risk for schizophrenia? A clinical and MRI studyGina Perez, Steve Spencer, Elizabeth Dick, Melissa Zeigler, Debra Montrose, Joe Pierri, Rick Sanders, Matcheri S. Keshavan (Pittsburgh, PA)
Background: A substantial body of literature points to both neurological examination abnormalities (NEA) and neuroimaging abnormalities in patients with schizophrenia. Studies of first-episode psychotic patients and offspring of schizophrenic patients allow investigation of NEA and brain morphology without the possible confounding effect of the illness and/or medications. The relatively few previous studies of NEA in recent-onset psychosis and offspring have involved small samples and/or have lacked adequate control groups. No studies to date have compared brain imaging and NEA. Methods: In this study, we evaluate both NEA and neuroimaging studies in first-episode psychotic patients and in offspring. The first-episode psychotic patients (SCZ; n=49) were matched with first-episode nonschizophrenic psychosis patients (NSCZ; n=25) and healthy, age-matched control subjects (HCN; n=34). The offspring of schizophrenic patients (n=16) were matched with healthy age-matched control subjects (n=20). All groups were evaluated with the Neurological Evaluation Scale (NES) and MRI studies. Results: Pairwise comparisons in the first-episode group revealed that SCZ patients scored higher than HCN in all NES parameters. The SCZ patients also scored higher than NSCZ in total NES and the motor coordination and “other signs” subscales. Total NES scores correlated with age in the SCZ and offspring groups but not in the control groups. The offspring showed significantly higher motor coordination deficits. An inverse relationship was seen between white matter volume and NEA in the SCZ group and the offspring group. Caudate volumes and NES were found to have an inverse relationship in the SCZ group. The control groups showed no correlation between NEA and brain morphology. Conclusions: Our findings suggest robust differences in NEA and brain imaging among recent psychotic patients and offspring at risk for schizophrenia. Neurological and neuroimaging abnormalities may be more severe in both schizophrenic patients and offspring of schizophrenic patients compared with control subjects. These abnormalities may reflect the primary pathophysiology of the illness and are unlikely to be simply a sequel to schizophrenia or its treatment.
P130. Neuropsychology of schizophrenia: cognitive evolutionLara Ruiz Socorro (Hospital San José, Popayán, Colombia)
Background: Schizophrenia implies a dysfunction in one or more of the principal areas of activity (interpersonal relations, work, studies, or self-care). Functioning is clearly inferior to the levels attained before the onset of symptoms (DSM-IV), and different cognitive deficits are observed in the distinct types of schizophrenia, for positive as well as negative symptoms. (Lara et al., Neuropsicología de la Esquizofrenia, 1995, 198–210). The study of the evolution of these cognitive deficits is a very important line of investigation in neuropsychiatry that contributes to determining whether or not cognitive deterioration will take place in this type of patient. Methods: A battery of neuropsychological tests was re-administered to 20 patients diagnosed with schizophrenia by DSM-IV criteria (10 paranoid and 10 residual), ages 20 to 50 years, who had been given the same tests 2 years previously. The tests evaluated attention, memory, language, praxis, gnosis, conceptual ability, and executive function. The performance of the two groups and comparison with the earlier results were analyzed according to standard methods. Results: After 2 years, the residual schizophrenic patients presented greater cognitive deterioration than the patients with paranoid schizophrenia. Conclusions: The diminished cognitive capacity in the residual patients involved all of the areas evaluated. In the paranoid patients, the decrease was observed mainly in the area of attention.[Translated, from the Spanish, by R. Rhodes.]
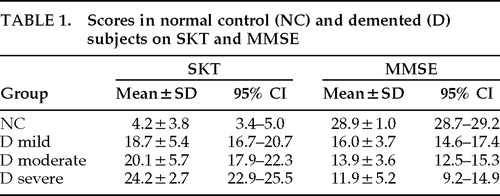 |