Psychosensory Symptoms in Combat Veterans With Posttraumatic Stress Disorder
Abstract
Psychosensory symptoms have relevance to the study of chronic posttraumatic stress disorder (PTSD), given that their presence is associated with limbic system dysfunction and that several features of chronic PTSD suggest that it, too, may be associated with limbic dysfunction. The Iowa Interview for Partial Seizure-like Symptoms (IIPSS), a measure of psychosensory symptoms, was administered to a PTSD group and a comparison group. The PTSD group generated significantly higher IIPSS scores than did the other group. Within the PTSD group, higher IIPSS scores were associated with significantly more severe PTSD symptoms, dissociative symptoms, aggression, and overall psychopathology.
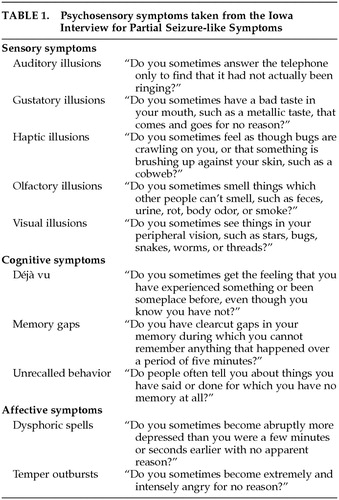
Psychosensory symptoms are of interest to mental health professionals because these symptoms have been noted to be present in a variety of psychiatric disorders, including affective disorders1 and chronic psychotic disorders.2 Although much of the pathophysiology of these symptoms is unclear, evidence suggests they are associated with limbic system dysfunction.3 Given this association, psychosensory symptoms (listed in Table 1) may have relevance to the study of chronic posttraumatic stress disorder (PTSD), since a number of features of chronic PTSD, including frequent complaints of rapid shifts in mood, aggressive impulses,4–6 dissociative phenomena,7–10 and memory disturbance,11,12 indicate that it may be associated with limbic dysfunction as well.
Beyond some clinical similarities in symptom profiles between PTSD patients and patients with documented limbic dysfunction, findings from various different avenues of research suggest a relationship between limbic dysfunction and chronic PTSD. Anatomic studies of limbic structures, in particular the hippocampal structures, have suggested that patients with chronic PTSD have altered limbic system anatomy compared with control populations.13–15 Pharmacotherapeutic (open clinical) trials of two agents often used to block seizures in patients with limbic dysfunction, carbamazepine and valproate, have found them to be effective in treating symptoms of PTSD.16–18 Lastly, studies of psychosensory symptoms in patients with early childhood abuse19 have shown that subjects with histories of childhood physical and sexual abuse have elevated scores on the Limbic System Checklist-33 (LSCL-33), an instrument that measures levels of self-reported psychosensory symptoms.
Given that psychosensory symptoms and chronic PTSD have been associated with limbic system dysfunction, we sought to measure to what degree psychosensory symptoms were present in a sample with chronic, combat-related PTSD. Because nearly 80% of veterans receiving inpatient PTSD services from this facility have had prior substance abuse–related diagnoses, a comparison group, patients without PTSD but with a history of alcohol or substance abuse, was examined as well. Correlations between psychosensory symptoms, PTSD symptoms, dissociative symptoms, aggression, and other psychopathologic symptoms were examined. PTSD patients with higher and lower levels of psychosensory symptoms were compared as well.
METHODS
Subjects
Sixty patients admitted to the North Little Rock, AR, PTSD rehabilitation program and 18 substance-abusing control subjects admitted to a domiciliary program for substance abuse recovery and work retraining were interviewed and completed a variety of psychological measures. Neither the PTSD nor the domiciliary program excluded veterans because of cognitive deficits or psychiatric histories. Study recruitment occurred at the time of admission to their prospective programs. All veterans who completed an informed consent form were entered in the study; no veterans were excluded from consideration.
All patients referred to the PTSD program carried a prior diagnosis of PTSD, and this diagnosis was validated with the Clinician-Administered PTSD Scale (CAPS). The patients also provided proof of military service (form DD-214) as a part of the application process to the PTSD rehabilitation unit. All PTSD patients completed a number of clinician-administered and self-report evaluations as a portion of their program assessment; a complete psychiatric interview was conducted as well.
The Structured Clinical Interview for DSM-IV (SCID-I) was administered to all control subjects to ensure that they met the diagnostic criteria for a drug-related diagnosis. They were further evaluated with the CAPS; none of the substance-abusing control subjects met the CAPS criteria for a diagnosis of PTSD and so were not given the PTSD-Interview (described below). Both groups completed all other measures.
Measures
Psychosensory symptoms were measured with the 35-question version of the Iowa Interview for Partial Seizure-like Symptoms (IIPSS).20 As recommended by its authors, no mention of epilepsy or brain disease was made to the subjects. Rather, the questionnaire was presented as the “Iowa Interview.” IIPSS scores were separated into highest and lowest quartiles and classified as “high” (the H-group) and “low” (the L-group), respectively. The H-group (n=21) were those veterans who generated an IIPSS score of 91 or more; the L-group (n=7) produced a score of 28 or less.
Intellectual functioning was assessed by using an abbreviated form of the Wechsler Adult Intelligence Scale–Revised.21 Prior research has demonstrated that IQ scores generated from this short form are as reliable as those produced from the entire scale.22 A measure of memory function was obtained by using the Wechsler Memory Scale-III Verbal Memory Index (VMI), a measure of immediate verbal memory.23
In addition, several scales evaluating the extent of psychopathology and general level of functioning were administered.
The Brief Symptom Inventory (BSI) is an abbreviated form of the Symptom Checklist-90-Revised (SCL-90-R).24 This 53-item self-report symptom inventory provides a score for nine primary symptom dimensions as well as an overall measure of symptom severity, the Global Severity Index (GSI). The Dissociative Experiences Scale (DES) is a 28-question self-report of dissociative symptoms, perhaps the most commonly used instrument to measure dissociation.25 As in other studies with PTSD samples, the fixed-response format was used in place of the traditional visual analogue format.26,27 The PTSD-Interview (PTSD-I) is a 17-item scale developed from the PTSD symptom criteria found in the DSM-III-R.28 The Hostility Scale,29 the Aggression Questionnaire,30 and the Combat Exposure Scale31 were given as well. Lastly, in order to compare the PTSD and Substance Abuse groups' drug and alcohol histories, the Michigan Alcoholism Screening Test (MAST)32 and the Drug Abuse Screening Test (DAST)33 were administered.
RESULTS
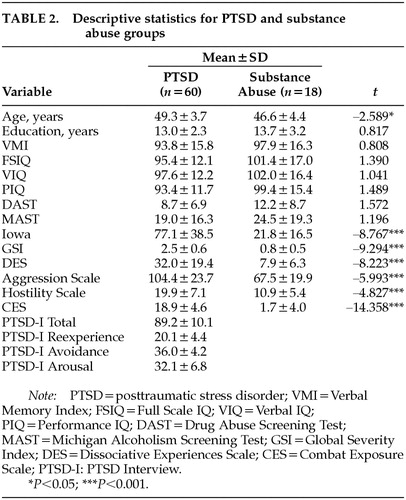
Descriptive statistics for the PTSD and substance abuse groups are reported in Table 2. The two groups differed in age, the PTSD group being significantly older than the comparison group. There were no group differences on educational level or on the memory and intelligence scores. Moreover, these two groups did not differ in the alcohol and drug histories they reported. Significant differences were generated for every measure of psychopathology (see Table 2).
Within the PTSD sample, the IIPSS score was significantly correlated with the following measures of psychopathology: SCL-90-R GSI (r=0.684, P<0.001), DES (r=0.705, P<0.001), PTSD-I Total (r=0.512, P=0.001), PTSD-I Re-experience (r=0.478, P=0.003), Aggression Scale (r=0.361, P=0.005), and Hostility Scale (r=0.479, P<0.001). The IIPSS scores were not significantly correlated with any of the IQ scores, age, or educational level, nor did they correlate with the Combat Exposure Scale (r=–0.013, P=0.925), PTSD-I Avoidance (r=0.226, P=0.178), or PTSD-I Arousal (r=0.293, P=0.079). Within the Substance Abuse sample, the only measures significantly correlated with the IIPSS score were the DES (r=0.713, P<0.001) and the Hostility Scale (r=0.727, P<0.001).
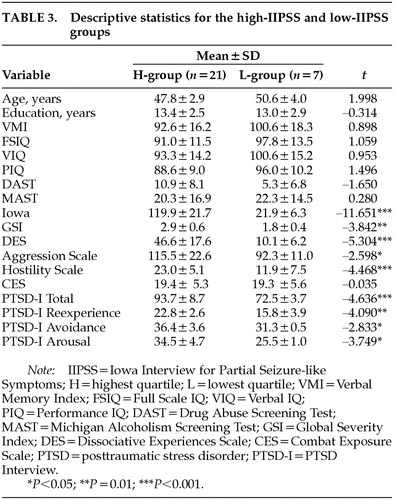
Within the PTSD sample, the H- and L-groups did not significantly differ on any of the demographic or performance measures. To determine whether the H-group (IIPSS top quartile scores) and L-group (IIPSS bottom quartile scores) veterans differed in their reported PTSD symptoms, dissociative experiences, exposure to combat, reported aggression, level of hostility, and overall psychopathology, a series of t-tests was conducted (Table 3). Significant differences were found for all but one variable, the Combat Exposure Scale (t=–0.035, df=58, P=0.972).
DISCUSSION
The present data show that the PTSD group experienced significantly more psychosensory symptoms, as measured by the IIPSS, than did the comparison group. Given the similar MAST and DAST scores produced by these two groups, it appears that the PTSD sample's drug and alcohol histories did not significantly differ from those of veterans with current substance abuse–related diagnoses. Consequently, the IIPSS scores within the PTSD group clearly show that the elevated psychosensory symptoms are not likely to be due to alcohol or drug histories. Certainly a shortcoming is that the effect of other variables, such as the presence of non–substance abuse psychiatric diagnoses, current medication regimens, or head injury histories, was not accounted for in this pilot study. Given the preliminary data, however, a more extensive project appears warranted.
Limitations notwithstanding, within the PTSD sample, the high-IIPSS (H) group generated significantly higher mean DES scores than did the low-IIPSS (L) group, 46.6 and 10.1, respectively. Likewise, when compared with the L-group, the H-group produced significantly higher PTSD scores, more so within the reexperiencing than the avoidance and arousal symptom clusters. These associations were not unexpected, given that both the IIPSS and DES are said to measure behaviors associated with temporolimbic disruption3,34–37 and that PTSD symptomatology is mediated in part through these brain structures.13–15
In the present study, patients with chronic, combat-related PTSD showed elevated levels of psychosensory symptoms when compared with a population of patients having similar substance abuse histories. Moreover, in the PTSD group, higher psychosensory symptoms were associated with higher PTSD, dissociative, and hostility scores. Perhaps identifying veterans with this PTSD symptom profile may assist clinicians in developing more efficacious treatment paths. Increasingly there is evidence that anticonvulsants are effective as a primary psychopharmacologic treatment for reducing PTSD symptomatology.16–18,38,39 Anticonvulsants are thought to be effective because they reverse the lowering of the discharge threshold in kindled limbic structures.40,41 To date, anticonvulsant trials have shown varied results in patients with chronic, combat-related PTSD. Future research may examine whether veterans with chronic, combat-related PTSD who also have elevated psychosensory and dissociative symptoms are more likely to benefit from this psychopharmacologic intervention.
 |
 |
 |
1 Ali S, Denicoff K, Ketter T, et al: Psychosensory symptoms in bipolar disorder. Neuropsychiatry Neuropsychol Behav Neurol 1997; 10:223-231Medline, Google Scholar
2 Atre-Vaidya N, Taylor M: Differences in the prevalence of psychosensory features among schizophrenic, schizoaffective, and manic patients. Compr Psychiatry 1997; 38:88-92Crossref, Medline, Google Scholar
3 Stevens J, Livermore A: Kindling in the mesolimbic system: an animal model of psychosis. Neurology 1978; 28:36-46Crossref, Medline, Google Scholar
4 McFall M, Fontana A, Raskind M, et al: Analysis of violent behavior in Vietnam combat veteran psychiatric inpatients with posttraumatic stress disorder. J Trauma Stress 1999; 12:501-517Crossref, Medline, Google Scholar
5 Yehuda R: Managing anger and aggression in patients with posttraumatic stress disorder. J Clin Psychiatry 1999; 60:33-37Crossref, Medline, Google Scholar
6 Lasko N, Gurvits TV, Kuhne AA, et al: Aggression and its correlates in Vietnam veterans with and without chronic posttraumatic stress disorder. Compr Psychiatry 1994; 35:373-381Crossref, Medline, Google Scholar
7 Tampke AK, Irwin HJ: Dissociative processes and symptoms of posttraumatic stress in Vietnam veterans. J Trauma Stress 1999; 12:725-738Crossref, Medline, Google Scholar
8 Bremner JD, Brett E: Trauma-related dissociative states and long-term psychopathology in posttraumatic stress disorder. J Trauma Stress 1997; 10:37-49Medline, Google Scholar
9 Marmar CR, Weiss DS, Schlenger WE, et al: Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry 1994; 151:902-907Crossref, Medline, Google Scholar
10 Hyer LA, Albrecht JW, Boudewyns PA, et al: Dissociative experiences of Vietnam veterans with chronic posttraumatic stress disorder. Psychol Rep 1993; 73:519-530Crossref, Medline, Google Scholar
11 Bremner JD: Does stress damage the brain? Biol Psychiatry 1999; 45:797-805Crossref, Medline, Google Scholar
12 Vasterling JJ, Brailey K, Constans JI, et al: Attention and memory dysfunction in posttraumatic stress disorder. Neuropsychology 1998; 12:125-133Crossref, Medline, Google Scholar
13 Bremner JD, Staib LH, Kaloupek D, et al: Neural correlates of exposure to traumatic pictures and sound in combat veterans with and without posttraumatic stress disorder: a positron emission tomography study. Biol Psychiatry 1999; 45:806-816Crossref, Medline, Google Scholar
14 Stein MB, Koverola C, Hanna C, et al: Hippocampal volume in women victimized by childhood sexual abuse. Psychol Med 1997; 27:951-959Crossref, Medline, Google Scholar
15 Bremner JD, Randall PS, Tammy M, et al: MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am J Psychiatry 1995; 152:973-981Crossref, Medline, Google Scholar
16 Davidson JR: Biological therapies for posttraumatic stress disorder: an overview. J Clin Psychiatry 1997; 58:29-32Medline, Google Scholar
17 Ford N: The use of anticonvulsants in posttraumatic stress disorder: case study and overview. J Trauma Stress 1996; 9:857-863Crossref, Medline, Google Scholar
18 Lipper S, Davidson JRT, Grady TA, et al: Preliminary study of carbamazepine in post-traumatic stress disorder. Psychosomatics 1986; 27:849-854Crossref, Medline, Google Scholar
19 Teicher MH, Glod CA, Surrey J, et al: Early childhood abuse and limbic system ratings in adult psychiatric outpatients. J Neuropsychiatry Clin Neurosci 1993; 5:301-306Link, Google Scholar
20 Roberts RJ: Epilepsy spectrum disorder in the context of mild traumatic brain injury, in The Evaluation and Treatment of Mild Traumatic Brain Injury, edited by Varney NR, Roberts RJ. Hillsdale, NJ, Lawrence Erlbaum, 1999, pp 209-247Google Scholar
21 Ward C: Prediction of verbal, performance, and full scale IQs from seven subtests of the WAIS-R. J Clin Psychology 1990; 46:436-440Crossref, Medline, Google Scholar
22 Schretlen D, Benedict R, Bobholz J: Composite reliability and standard errors of measurement for a seven-subtest short form of the Wechsler Adult Intelligence Scale-Revised. Psychol Assess 1994; 6:188-190Crossref, Google Scholar
23 Wechsler D: Manual for the Wechsler Memory Scale, Third Edition. New York, The Psychological Corporation, 1997Google Scholar
24 Derogatis LR, Melisaratos N: The Brief Symptom Inventory: an introductory report. Psychol Med 1993; 13:595-605Crossref, Google Scholar
25 Bernstein E, Putnam F: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727-735Crossref, Medline, Google Scholar
26 Frueh B, Johnson D, Smith D, et al: A potential problem with the response format of the dissociative experiences scale: a significant correlation with intelligence among combat veterans with PTSD. J Trauma Stress 1996; 9:651-656Crossref, Medline, Google Scholar
27 Smith D, Frueh B: Compensation seeking, comorbidity, and apparent exaggeration of PTSD symptoms among Vietnam combat veterans. Psychol Assess 1996; 8:3-6Crossref, Google Scholar
28 Watson CG, Juba MP, Manifold V, et al: The PTSD interview: rationale, description, reliability, and concurrent validity of a DSM-III-based technique. J Clin Psychology 1991; 47:179-188Crossref, Medline, Google Scholar
29 Blackburn R: The Development and Validation of Scales to Measure Hostility and Aggression. London, Special Hospitals Research Unit, 1974Google Scholar
30 Buss A, Perry M: The Aggression Questionnaire. J Pers Soc Psychol 1992; 63:452-459Crossref, Medline, Google Scholar
31 Keane TM, Caddell JM: Clinical evaluation of a measure to assess combat exposure. Psychol Assess 1989; 1:53-55Crossref, Google Scholar
32 Selzer ML: The Michigan Alcoholism Screening Test: the quest for a new diagnostic instrument. Am J Psychiatry 1971; 127:1653-1658Crossref, Medline, Google Scholar
33 Skinner HA: The Drug Abuse Screening Test. Addict Behav 1982; 7:363-371Crossref, Medline, Google Scholar
34 Chambers RA, Bremner JD, Moghaddam B, et al: Glutamate and post-traumatic stress disorder: toward a psychobiology of dissociation. Semin Clin Neuropsychiatry 1999; 4:274-281Medline, Google Scholar
35 Zahn T, Moraga R, Ray W: Psychophysiological assessment of dissociative disorders, in Handbook of Dissociation: Theoretical, Empirical, and Clinical Perspectives, edited by Michelson LK, Ray WJ. New York, Plenum, 1996, pp 269-287Google Scholar
36 Hines ME, Kubu CS, Roberts RJ, et al: Characteristics and mechanisms of epilepsy spectrum disorder: an explanatory model. Appl Neuropsychol 1995; 2:1-6Crossref, Medline, Google Scholar
37 Devinsky O, Putnam F, Grafman J, et al: Dissociative states and epilepsy. Neurology 1989; 39:835-840Crossref, Medline, Google Scholar
38 Hertzberg MA, Butterfield MI, Feldman ME, et al: A preliminary study of lamotrigine for the treatment of posttraumatic stress disorder. Biol Psychiatry 1995; 45:1226-1229Crossref, Google Scholar
39 Brannon N, Labbate LA, Huber M: Gabapentin treatment for posttraumatic stress disorder (letter). Can J Psychiatry 2000; 45:84Crossref, Medline, Google Scholar
40 Keck P, McElroy M, Friedman L: Valproate and carbamazepine in the treatment of panic and posttraumatic stress disorders, withdrawal states and behavioral dyscontrol syndromes. J Clin Psychopharmacol 1992; 12(suppl 1):36-41Google Scholar
41 Post R, Weiss S, Chung D: Mechanisms of action of anticonvulsants in affective disorders. J Clin Psychopharmacol 1992; 12(suppl 1):23-35Google Scholar