Apathy in Dementia: An Examination of the Psychometric Properties of the Apathy Evaluation Scale
Marin et al. 2 , 10 reported that all versions of the AES differentiated between dementia groups according to levels of apathy. 2 , 10 For the most part, the scale was found to be a single factor scale with apathy accounting for 32% to 53% of the variance. 2 Interest (5% to 10% of the variance) and insight/concern (7% to 8% of the variance) factors were also identified. 2 Together, the three factors accounted for 50% to 65% of the total variance. 2 The scale reportedly has good interrater (Cronbach's alpha (α)= 0.86–0.94) and test-retest reliability (α= 0.76–0.94). Marin et al. 2 , 10 reported a cutoff score of 37.5 for the AES-C, which was two standard deviations above the score for normal healthy elderly persons, but the sensitivity and specificity were not indicated.
Other studies have provided support for the scale’s ability to differentiate between apathetic and nonapathetic individuals 2 , 5 , 10 , 11 and between dementia groups 2 , 5 , 6 , 10 with the AES-C. However, there is a lack of studies that reassess the factor structure and psychometric properties of the scale. Our recent critical appraisal of the psychometric properties of the AES-C (submitted) called for a more analytical assessment of the measurement properties of the scale. We suggested that with sufficient sample size, the properties of the scale should be reassessed in diagnostic and age groups that are different from those who were originally tested.
This article reexamines the factor structure of the three versions of the AES and identifies cutoff scores for apathy. The study also examines the psychometric properties of the three versions of the AES, including sensitivity and specificity, using the identified cutoff scores, and reliability and validity. It is hoped that information from this study will inform future use of the scale in the assessment of apathy in dementia and ultimately enhance treatment regime.
METHOD
Participants were drawn from the Behavioral Neurology Clinic at Baycrest Centre for Geriatric Care in Toronto, Canada. This is an outpatient multidisciplinary clinic headed by Behavioral Neurology. The team comprised clinicians in neurology, psychiatry, neuropsychology, communication disorders, occupational therapy, and social work. The clinic provides thorough diagnostic assessments and management to patients with cognitive disorders. The referral sources were primary care physicians and specialists.
The study sample represents individuals in whom the presence of dementia was strongly suspected and who were referred to psychiatry (RvR) for assessment and/or management between January 1997 and December 1998. This represented 121 of the 170 participants seen by the behavioral neurologist (MF) during the 2-year period. The sample consisted of community-dwelling individuals still living in their own homes and a few nursing home residents (4.2%). All were able to attend outpatient assessments.
The Psychiatric Assessment
The psychiatric assessments consisted of two components: first, participants and their caregivers were seen by the clinical research assistants who administered a battery of tests to assess for presence of apathy and other neurobehavioral conditions, such as depression, psychosis, and agitation. Participant and caregiver/relative interviews were conducted separately by different clinical research assistants who collected information on age, sex, marital status, level of education, and living situation. A summary of the results was compiled and presented to the psychiatrist (RvR) and his resident, who incorporated this information (as is appropriate for this clinical data) into the psychiatric assessment.
Next, the psychiatrist and his resident then completed their own (but unblinded) clinical assessment for apathy, depression, psychosis, and other behavioral changes. The psychiatrist's diagnostic conclusions for apathy, which were based on criteria proposed by Marin, 1 , 9 were taken from the consultation note and used as the gold standard in the study. The psychiatrist (RvR) is a fellow of the Royal College of Physicians and Surgeons in Canada (equivalent to board certification in the United States) and has worked extensively with this patient population in his clinical practice.
Apathy, in the month prior to the interview, was measured using the three versions of the AES. The apathy subscale of the Neuropsychiatric Inventory (NPI) 12 , 13 was also used to assess for the presence of apathy to enable the examination of the convergent validity of the three versions of the AES (in contrast to the method of Marin et al., 2 in which the correlations between the three versions of the AES were used as the only support for this important property of the scale). The NPI is an informant-based interviewer-administered scale developed by Cummings et al. 12 , 13 to measure a range of behavioral disturbances, including delusions, hallucinations, agitation, depression, anxiety, elation, apathy, disinhibition, irritability, aberrant motor behavior, sleep behavior and appetite behavior, in individuals with dementia.
The other subscales of the NPI enabled the examination of the discriminant validity of the AES scales. For example, it was expected that apathy should not be highly correlated with the subscales if the scales had good discriminant validity, representing different constructs. The NPI is administered to a knowledgeable informant and inquires into the presence of the behavioral disturbances, and the frequency and severity of each disturbance. 12 , 13 Severity is ranked on a three-point scale (1 to 3; mild, moderate, severe) and frequency on a four-point scale (1 to 4; occasionally, often, frequently, and very frequently). 12 , 13 The NPI reportedly has good validity and reliability. 12 – 14 The depression portion of the Structured Clinical Interview for DSM-IV (SCID) 15 was also used to assess for the presence of depression to further assess the discriminant validity of the AES. The SCID is a widely used semistructured interview for DSM diagnoses. 15
Following the assessment of each participant by the behavioral neurologist, the psychiatrist, and neuropsychologist, as well as cerebral imaging that was ordered (i.e., computed tomography [CT], magnetic resonance imaging [MRI], and single photon emission computed tomography [SPECT] scans), the participant’s chart was reviewed to determine whether the individual met NINCDS/ADRDA criteria for possible or probable Alzheimer’s disease, 16 the Consortium on Dementia with Lewy Bodies criteria for dementia with lewy bodies, 17 the Lund and Manchester criteria for frontotemporal dementia 18 and/or the Hachinski criteria for vascular dementia. 19 Participants who met multiple diagnostic criteria received a diagnosis of mixed dementia.
Data Analysis
We conducted descriptive analyses to characterize the study sample, and exploratory factor analyses with principal axes factoring and varimax rotation methods to examine the factor structure of the AES. Sample size issues restricted the ability to conduct confirmatory factor analyses. Cronbach’s alpha was calculated to determine the internal consistency of each identified factor. Receiver operating characteristic (ROC) analyses were employed, using the psychiatrist’s diagnosis of apathy as the gold standard, to identify the cutoff scores for the three versions of the scales. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of each version of the AES were calculated. Correlational analyses were also conducted to investigate the convergent and discriminant validity of the AES. All analyses were performed using SPSS for Windows version 12.0. 20
RESULTS
Characteristics of the Participants Referred for Psychiatric Assessment
The sample consisted of 52.9% women. The mean age was 73.7 (SD=9.4) years. Most reported being married (79.3%) and living with a spouse (73.7%). Forty-four percent of the group had partial to complete high school education. Research diagnoses were ascertained for 105 of the 121 participants. The frequencies of diagnosis were as follows: 55.2% Alzheimer's disease; 14.3% mixed dementia, which included possible Alzheimer’s disease and possible dementia with lewy bodies; 9.5% dementia with lewy bodies; 5.7% vascular dementia, 5.7% mixed dementia, which included Alzheimer’s disease and vascular dementia; 4.8% frontotemporal dementia; and 4.8% other dementia.
Assessment of the Psychometric Properties of the Apathy Evaluation Scale
Table 1 presents the results of the factor analysis for the three versions of the AES. For the clinician and informant versions of the scale, two factors were identified which accounted for 51.1% and 54.4% of the variance, respectively. The two factors identified for both versions of the scale were apathy and interest. Examples of some of the items that loaded onto the apathy factor included, “S/he has initiative,” “S/he has motivation,” and “S/he gets things done during the day.” Some of the items that loaded on the interest factor were as follows: “S/he is interested in things,” “S/he is interested in having new experiences,” and “S/he is interested in learning new things.” For the AES-C, the apathy and interest factors accounted for 42.4% and 8.7% of the variance, respectively. However, the interest factor accounted for the majority of the variance for the AES-I (45.1%) compared with the apathy factor (9.3%). The AES-S also had two factors, with the major factor being apathy, which accounted for 36.4% of the variance. The second factor for AES-S, identified herein as “other,” accounted for 6.9% of the variance. The items that loaded onto this factor included, “Do you get things done during the day?” “Do you put little effort into anything?” and “Are you less concerned about your problems than you should be?”
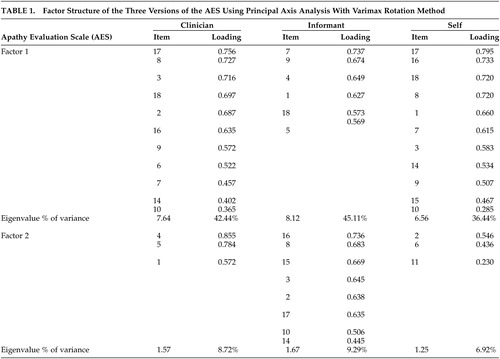 |
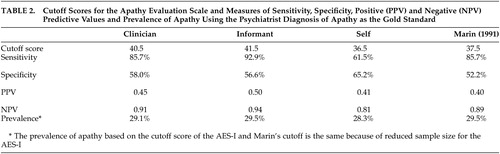
Figure 1 and 2 present the ROC curve for the AES-I and AES-C, respectively (a similar figure for the AES-S is available upon request). The area under the curve for the AES-C, AES-I and AES-S was 0.72, 0.82 and 0.65, respectively. Table 2 presents the results of ROC analyses, including the cutoff scores, sensitivity, specificity, positive predictive value, negative predictive value and the prevalence per the AES-C, AES-I and AES-S. Using the psychiatrists’ unblinded diagnoses of apathy as the gold standard, cutoff scores of 40.5, 41.5, and 36.5 were identified for the AES-C, AES-I, and AES-S, respectively. Optimal psychometric performance appeared to be with the AES-I, with sensitivity of 92.9%, specificity of 56.6%, prevalence of 29.5%, positive predictive value of 0.50, and negative predictive value of 0.94. The AES-S gave relatively weaker results across the board, and the AES-C was stronger than the AES-I only in terms of specificity, with a minimally higher result of 58%.
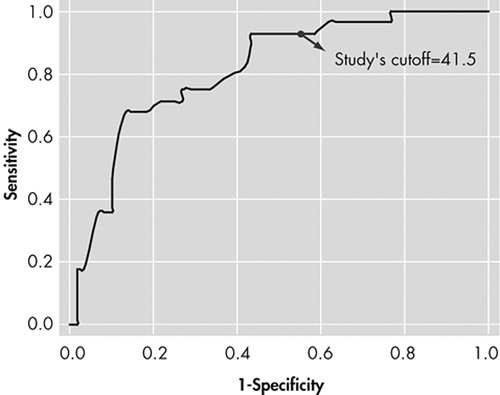
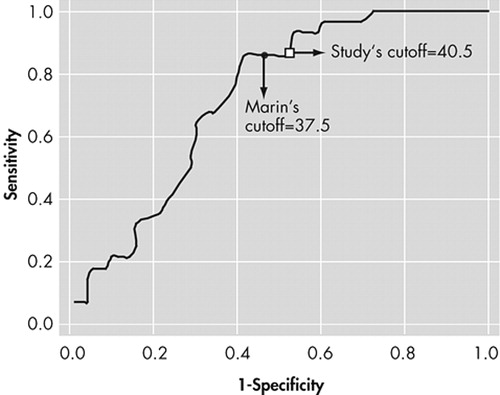
 |
Internal consistencies of the factors identified for the three versions of the 18-item scale were measured by Cronbach’s alpha coefficient ( Table 3 ). The internal consistencies of the apathy and interest factors for the AES-C were 0.90 and 0.86, respectively. Similarly, high standardized Cronbach’s alpha coefficients were found for the apathy and interest factors of the AES-I (i.e., 0.90 and 0.88, respectively). For each factor, the removal of any of the loaded items did little to improve the standardized alpha coefficient. The internal consistencies of the identified factors for the AES-S were 0.90 for apathy and 0.41 for the factor identified as “other.”
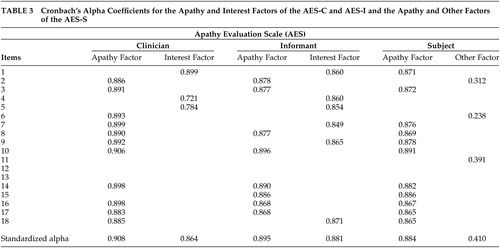 |
Table 4 presents the results of the correlational analyses examining the discriminant and convergent validity of the AES. The total scores and the scores for the apathy factor of AES-C, AES-I, and AES-S were significantly correlated with the frequency x severity score of the apathy subscale of the NPI, but the strength of the relationships was not very high. These findings indicate better convergent validity for the AES-I (r=0.5, p<0.001) compared with the AES-C (r=0.3, p<0.01) and the AES-S (r=0.2, p<0.05). Given that the NPI-apathy was informant-rated, it was not unexpected that the correlation of this score with the informant version of the AES would be higher.
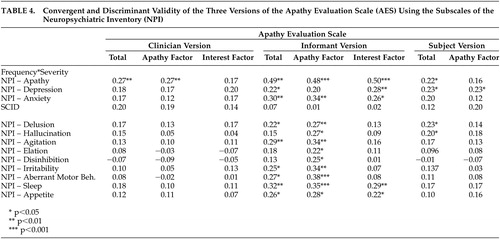 |
Unlike the AES-C, the total scores of both the AES-I and AES-S, as well as the interest factor of the AES-I and the apathy factor of the AES-S, had statistically significant correlations with the depression subscale of the NPI. However, the levels of correlation were not very high. These results indicate fair discriminant validity of the informant and self-rated versions of the AES and good discriminant validity of the clinician version of the scale. The AES-C, AES-I, and AES-S had statistically nonsignificant relationships with the clinician-rated Structured Clinical Interview for DSM-IV (SCID), providing further support for their fair to good discriminant validity. With regards to the delusion, hallucination, agitation, elation, disinhibition, irritability, aberrant motor behavior, sleep disturbance, and appetite disturbance, the AES-I, particularly the apathy factor, was significantly correlated with all subscales, while the AES-C and AES-S scales and their factors generally did not correlate well with these NPI subscales.
DISCUSSION
The main findings of this study relate to the factors identified as well as the optimal psychometric performance of the AES-I compared with both the AES-C and AES-S. However, it is important to note that this clinical investigation was prone to limitations as follows. There was a lengthy waiting list for the Behavioral Neurology Clinic, which might have led to a referral bias (e.g., there may have been a selection bias toward more diagnostically challenging or more difficult-to-manage cases being seen). We were also unable to maintain blindness of the psychiatrist to the results of the AES, and other neurobehavioral measures, as these were clinical data. These results might have influenced the psychiatrist’s diagnosis of apathy. As such, there is a need for a better gold standard for apathy in future studies that either examine the psychometric properties of the three versions of the AES or aim to develop new apathy scales. The AES-C and SCID were administered by the same clinical research assistant during the same interview session for each subject and results from one inventory may have influenced results from the others. Despite these limitations, this research has provided support for the internal consistency and the validity of the AES, particularly the informant and clinician versions. Another limitation to the study relates to the lack of information on ethnicity. Ethnicity has been found to be associated with apathy 21 , 22 and therefore the lack of information on this variable possibly affected the results obtained.
Using the rule of a minimum of three items per factor, two factors were identified for each of the AES scales in this sample. These included factors of apathy and interest for the AES-C and AES-I, and apathy and “other” for the subject version of the scale. These results differed from those of Marin et al. 2 who identified three factors for the AES-C, two factors for the AES-S and one factor for the AES-I. However, the findings were also similar to the original study 2 in the identification of apathy and interest factors. For the AES-C, the items that loaded onto the apathy and interest factors were quite similar to the item loading shown in Marin et al.’s original study. 2 The items that loaded onto the apathy factor for the AES-C, AES-I, and AES-S were quite similar in this study, but three of the six items that loaded onto the interest factor of the AES-I were items that loaded onto the apathy factors of the AES-C and AES-S. These items were as follows: “S/he approaches life with intensity,” “S/he spends time doing things that interest her/him,” and “S/he has motivation.” At face value, the items appear to be related to apathy more so than interest. The validity of the second factor for the AES-S is questionable in that, at face value and theoretically, the items do not appear to be related, except for the fact that two of the three are the negatively worded items included in the scale.
Cronbach’s alpha coefficients greater than or equal to 0.70 are said to be indicative of good internal consistency of a scale. 23 The observed Cronbach’s alpha coefficients of 0.91, 0.86, and 0.90, 0.88 and 0.88 for the apathy and interest factors of the AES-C and AES-I, respectively, and the apathy factor of the AES-S indicated very good internal consistencies. However, the 0.41 Cronbach’s alpha coefficient for the “other” factor of the AES-S indicated poor internal consistency. As such, it can be concluded that two reliable factors were identified for the AES-C and AES-I and one for the AES-S.
As with Marin et al., 2 the AES-C was found to have fairly good psychometric properties. However, optimal psychometric performance was observed with the informant version of the AES. The cutoff score of 40.5 for the AES-C was higher than the score of 37.5 observed by Marin et al., 2 and that of 38 observed by Pluck and Brown, 22 and is possibly a function of the differences in the makeup of the samples studied. Our cutoff score performed slightly better than that of Marin et al. with the same sensitivity (85.7) but slightly higher specificity (58.0 versus 52.2), positive predictive value (0.45 versus 0.40) and negative predictive value (0.91 versus 89.2). Marin et al. 2 had strict criteria for inclusion and exclusion for their study sample. This study, however, included a clinical population of patients who were all diagnosed with dementia and therefore were more likely to be impaired cognitively and functionally. As such, the cutoff score might appropriately be higher than that found using a “healthier” population. Pluck and Brown included only individuals with Parkinson’s disease who may or may not have had dementia. 24 This is the only study to date to provide a cutoff score for the informant version of the AES, which was one point higher than that of the clinician version.
The clinician version of the AES showed fair convergent validity by its statistically significant correlation with the apathy subscale of the NPI. The convergent validity of the AES-I appeared to be better than that of the AES-C and AES-S, but this could be due to the fact that both the AES-I and the apathy subscale of the NPI were informant-based and likely completed by the same informant. In contrast, the clinician version of the AES showed good discriminant validity by failing to have statistically significant correlations with the SCID depression, as well as the depression, anxiety, and other subscales of the NPI.
From a diagnostic point of view, the AES-I provided the greatest sensitivity as well as the strongest positive and negative predictive values. At a prevalence rate of 29.5% (based on the psychiatrist’s assessments), the combination of a high NPV and low PPV (0.5) suggests that the AES-I may be used clinically as a screening tool to rule out the presence of apathy when results are less than the cutoff score, and to encourage a clinician assessment when results are above the cutoff score. The AES-C and the AES-S do not appear to add diagnostically to the AES-I, and hence are probably unnecessary for clinical use.
It is important to note that the assessors who administered the clinician version of the AES had bachelor’s-level training in health-related fields with 1 to 5 years of experience working with dementia patients and more than 4 to 6 hours of experience with the scale, a criterion that Marin stated would be sufficient for reliable rating. 2
However, it is possible that this level of training was not sufficient for reliable rating and might account for the less than optimal performance of the AES-C, a point raised in our critical appraisal of the AES-C. This “level of training” hypothesis could be investigated by comparing the rating of apathy with the AES-C across raters with different levels of training and experiences with the dementia population (i.e., interrater reliability), but this was not done in this current study. An alternate explanation for the less than optimal performance of the AES-C might be that the interviewer or rater needed to be someone who knew the patients well, or at least had time to observe the individuals’ behaviors in performing tasks that required initiative and self-motivation. This point was supported by the better performance of the AES-I. Therefore, in research settings where the research personnel or assessors have only bachelor’s-level training and less than 5 years of experience with dementia patients, it might be more appropriate to use the AES-I instead of the AES-C.
1. Marin RS: Apathy: a neuropsychiatric syndrome. J Neuropsychiatry Clin Neurosci 1991; 3:243–254Google Scholar
2. Marin RS, Biedrzycki RC, Firingiogullari S: Reliability and validity of the Apathy Evaluation Scale. Psychiat Res 1991; 38:143–162Google Scholar
3. Cummings J: Frontal-subcortical circuits and human behaviors. Arch Neurol 1993; 50:873–880Google Scholar
4. Gray JM, Shepherd M, McKinley WW: Negative symptoms in the traumatically brain-injured during the first year postdischarge, and their effect on rehabilitation status, work status and family burden. Clin Rehabil 1994; 8:188–197.Google Scholar
5. Resnick B, Zimmerman SI, Magaziner J, Adelman A: Use of the Apathy Evaluation Scale as a measure of motivation in elderly people. Rehabil Nurs 1998; 23:141–147Google Scholar
6. Andersson S, Krogstad JM, Finset A: Apathy and depressed mood in acquired brain damage: Relationship to lesion localization and psychophysiological reactivity. Psychol Med 1999; 29:447–456Google Scholar
7. Andersson S, Gundersen PM, Finset A: Emotional activation during therapeutic interaction in traumatic brain injury: effect of apathy, self-awareness and implications of rehabilitation. Brain Inj 1999; 13:393–404Google Scholar
8. van Reekum R, Stuss DT, Ostrander L: Apathy: why care? J Neuropsychiatry Clin Neurosci 2005;17: 7–19Google Scholar
9. Marin RS: Differential diagnosis and classification of apathy. Am J Psychiatry 1990; 147:22–30Google Scholar
10. Marin RS, Firinciogullari S, Biedrzycki RC: The sources of convergence between measures of apathy and depression. J Affect Disord 1993; 28:117–124Google Scholar
11. Lampe IK, Kahn RS, Heeren TJ: Apathy, anhedonia, and psychomotor retardation in elderly psychiatric patients and healthy elderly individuals. J Geriatr Psychiatry Neurol 2001; 14:11–16Google Scholar
12. Cummings JL, Mega M, Gray K, et al: The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 1994; 44:2308–2314Google Scholar
13. Cummings JL: The neuropsychiatric inventory: assessing psychopathology in dementia patients. Neurology 1997; 48(suppl 6): 10–16Google Scholar
14. Mega M, Cummings JL, Fiorello T, et al: The spectrum of behavioral changes in Alzheimer’s disease. Neurology 1996; 46:130–135Google Scholar
15. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis I Disorders – Nonpatient Edition (SCID-I/NP, Version 2.0). New York, Biometrics Research Department, 1996Google Scholar
16. McKahn G, Drachman D, Folstein M, et al: Clinical diagnosis of Alzheimer’s’s disease: Report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology 1984; 34:939–944Google Scholar
17. McKeith IG, Galasko D, Kosaka K, et al: Consensus guidelines for the clinical and pathological diagnosis of dementia with lewy bodies: report of the consortium on DLB international workshop. Neurology 1996; 47:1113–1124Google Scholar
18. The Lund and Manchester Groups: Clinical and neuropathological criteria for frontotemporal dementia. J Neurol Neurosurg Psychiatry 1994; 57:416–418Google Scholar
19. Hachinski VC, Iliff LD, Zilhka E, et al: Cerebral blood flow in dementia. Arch Neurol 1975; 32:632–637Google Scholar
20. SPSS statistical Software for Windows, Version 12.0Google Scholar
21. Binetti G, Mega MS, Magni E, et al: Behavioral disorders in Alzheimer’s disease: a transcultural perspective. Arch Neurol 1998; 55:539–544Google Scholar
22. Hargrave R, Stoeklin M, Haan M, et al: Clinical aspects of dementia in African-American, Hispanics and white patients. J Nat Med Assoc 2000; 92:15–21Google Scholar
23. Nunnelly JC: Psychometric Theory, 2nd ed. New York, Mcgraw Hill, 1978, pp 225–255Google Scholar
24. Pluck GC, Brown RG: Apathy in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2002; 73:636–642Google Scholar



