Antidepressant Effects of High and Low Frequency Repetitive Transcranial Magnetic Stimulation to the Dorsolateral Prefrontal Cortex
Repetitive TMS (rTMS) to a cortical area is capable of enhancing or decreasing cortical excitability of that area beyond the duration of the TMS train. Studies on the motor cortex have revealed that 1 Hz of stimulation has a largely suppressive effect while frequencies of 10 Hz or greater are largely excitatory. 2 , 3
These opposite effects of high and low frequency rTMS have been confirmed using single photon emission computed tomography (SPECT) and positron emission tomography (PET) functional imaging techniques in studies using rTMS to target the prefrontal cortex in patients with depression. 4 , 5
Patients with major depressive disorder often have low levels of activity in the left prefrontal cortex. 6 – 11 Various studies have reported antidepressant effects of high frequency (≥10 Hz) rTMS to the left dorsolateral prefrontal cortex (DLPFC). 12 – 16 Other studies have found antidepressant effects using low frequency (≤1 Hz) rTMS, 17 which might be expected to decrease cortical excitability, applied to the right DLPFC.
Despite the growing body of evidence that rTMS can have antidepressant effects, there remains some confusion as to the most beneficial stimulation site and parameters. Fitzgerald et al. 18 have suggested that both high frequency left-sided DLPFC and low frequency right-sided DLPFC stimulation have equivalent antidepressant effects, while other permutations are less helpful. In the present study, we set up to test this hypothesis further and provide confirming evidence supporting the conclusions of Fitzgerald et al.
METHOD
The study was a parallel group, sham-controlled, double-blind trial. Forty-five patients with unipolar major depressive disorder (SCID and DSM-IV) were randomized to four groups.
Group 1. High frequency left-sided DLPFC rTMS (N=10)
Group 2. Low frequency left-sided DLPFC rTMS (N=10)
Group 3. Low frequency right-sided DLPFC rTMS (N=10)
Group 4. Sham rTMS (N=15)
Group 4. (Sham rTMS) was subdivided into three further groups corresponding to the sites of real stimulation:
Group 4a. High frequency left-sided DLPFC sham rTMS (N=5)
Group 4b. Low frequency left-sided DLPFC sham rTMS (N=5)
Group 4c. Low frequency right-sided DLPFC sham rTMS (N=5)
High frequency right-sided DLPFC rTMS was not included in this study, given the negative results of this intervention in a previous study. 15
The patients in our study had all been referred for ECT having failed an adequate course of antidepressant medication.
The patient characteristics are summarized in Table 1. The number of patients with a history of hospitalization, ECT, or suicide attempts is relatively high compared with the general population of patients with major depressive disorder, suggesting that these patients are at the sicker end of the spectrum.
 |
All patients were right-handed (Oldfield questionnaire) and between the ages of 21 and 80. Patients were interviewed by a psychiatrist who was able to consult with their treating psychiatrist, and they met DSM-IV criteria for a major depressive episode with a score ≥20 on the 21-item Hamilton Depression Rating Scale (HAM-D).
They had no psychotic features and no other Axis I disorders. All patients were naïve to TMS, and none had participated in previous research studies on TMS and depression. All patients were treated as outpatients. The study was approved by the Institutional Review Board. Written consent was obtained from all participants. Patients then underwent a 14-day washout of all psychotropic medication, and the reinstatement of this medication was not permitted until the protocol was completed. PRN Lorazepam (maximum of 2 mg per day) was allowed during the first 7 days of washout. Patients unable to tolerate the medication withdrawal were excluded.
Exclusion criteria included a history of any psychotic disorder, including schizophrenia or schizoaffective disorder; bipolar disorder; obsessive compulsive disorder; personality disorder; substance abuse (except nicotine) within past year; current acute or chronic medical condition requiring treatment with psychoactive medication; a history of epilepsy or unprovoked seizures or other neurological disorder; abnormal neurological examination; family history of medication-resistant epilepsy; prior brain surgery; metal in the head; an implanted medical device; or pregnancy.
rTMS sessions were conducted at a laboratory staffed by personnel certified in basic life support and trained in the prompt recognition and treatment of seizures and other medical emergencies. A physician was always present during the treatments. Emergency equipment such as oxygen, IV access tools, and emergency medication was available.
We used a Dantec Magpro magnetic stimulator (Dantec Medical Inc, Denmark) and a Magstim Super-Rapid Magnetic Stimulator (Magstim Corporation, UK). Both used an identical 8-shaped focal stimulation coil. These machines were used randomly between patients, with each patient receiving stimulation from only one machine. Treatment parameters were based on motor threshold and were thus independent of any intermachine variability. Sham TMS was delivered by orienting the coil perpendicularly to the patient’s scalp, while in the treatment conditions the coil was held tangentially to the scalp. During each treatment, the patient’s head was held with a head support and coil position was fixed using a coil holder.
Motor threshold was determined on the first day of treatment in accordance with the recommendations of the International Federation of Clinical Neurophysiology. 19
Surface EMG electrodes were used to record from the belly of the right abductor pollucis brevis (APB) muscle. Using suprathreshold stimulation, the stimulation site producing the maximal EMG response was identified. A descending staircase technique was used to determine the threshold for APB activation. The threshold was defined as the lowest stimulation intensity to produce MEPs of at least 50uV amplitude (peak to peak) in at least five out of 10 trials.
As in previous studies, 15 stimulation was applied to an area 5 cm anterior of and in the same parasagittal plane as the site producing the maximal EMG response in the contralateral APB muscle. This is presumed to have targeted the middle third of the frontal gyrus, approximately the border of Broca’s areas 46 and 9. Fitzgerald et al. 18 used the same landmarks in their study.
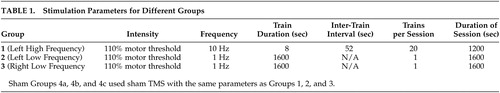
The stimulation parameters for the different groups are shown in Table 1.
In compliance with current safety guidelines, 20 patients and TMS technicians wore earplugs to prevent possible auditory threshold shifts. All sessions, including sham, were conducted under continuous video monitoring to allow for detailed evaluation of any unexpected complication. Patients completed a side effect checklist before and after each TMS application. The parameters for Group 1 ( Table 1 ) were slightly above the recommended safety guidelines, which recommend a maximum intensity of 80% motor threshold. However, our growing body of experience 1 suggests that these parameters are safe. Patients were made aware of the limited availability of safety data during the process of informed consent.
A psychiatrist blinded to group assignment conducted all assessments of patients’ symptoms. He was able to discuss the cases with the patients’ treating psychiatrists but remained blinded to group assignment. Patients were evaluated following the 14-day medication withdrawal period and weekly thereafter using the 21-item HAM-D. 21 In accordance with many other studies on depression, a clinically significant response was defined as a HAM-D reduction ≥50% relative to pretreatment baseline. Remission was defined as a HAM-D score ≤10. All subjects had a baseline score of ≥20 on the HAM-D (21 item); therefore all patients fulfilling the criteria for remission also fulfilled the criteria for clinical response.
RESULTS
Demographics
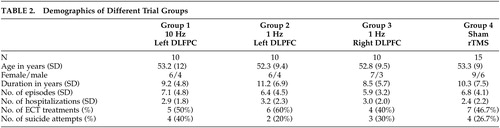
Baseline patient characteristics of the different study groups were compared using a one-way analysis of variance (ANOVA) which confirmed comparable study populations. Table 2 summarizes the patient characteristics of the four different groups. There were no significant differences in age, gender, handedness (Oldfield Inventory Scores), duration of major depressive disorder, number of depressive episodes, number of hospitalizations for depressive episodes, or suicide attempts or prior ECT.
 |
There was no significant difference between groups in baseline HAM-D score (F [3, 41]=0.02, p>0.05) although there was some variability between individual subjects. To minimize this, results were analyzed using percentage decrease from baseline HAM-D score in each subject.
HAM-D Scores
None of the patients in Group 2 (left-sided, low frequency rTMS) or Group 4 (sham rTMS) met the criteria for a clinical response. However, at the end of the 10 days of stimulation, 60% of the patients in Group 1 (left-sided, high frequency rTMS) and 60% in Group 3 (right-sided, low frequency rTMS) showed a clinical response. Similarly, while none of the patients in Group 2 or Group 4 met the criteria for remission, 33.3% of the patients in Group 1 and 10% of the patients in Group 3 showed this level of improvement ( Table 3 ).
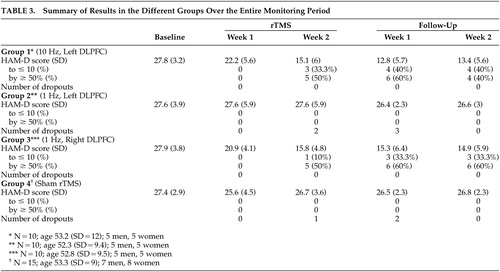 |
All patients were followed up for 2 weeks after the treatments ended. The number of patients in remission in both Group 1 and Group 3 increased slightly in the week following treatment (from five to six). In Group 1, the number of patients in remission had fallen to four by Week 2 of follow-up, representing an increase in HAM-D score above the threshold for remission for two patients. The difference between Group 1 and Group 3 at this stage was not statistically significant. The patients in Group 1 and Group 3 had their HAM-D scores reevaluated 4 weeks after treatment. Since only the active groups were followed up, this must be regarded as an unblinded follow-up. Four out of 10 patients in Group 1 and two out of 10 patients in Group 3 still met the criteria for a clinical response. The average decrease in HAM-D score between baseline and 4 weeks posttreatment was 40% in both groups.
Statistical Analysis
A mixed design factorial analysis was performed between the four groups over the four time points. Significant changes were found between both the different groups (10 Hz left, 1 Hz left, 1 Hz right, and Sham: F [3]=25.70, p<0.0005) and the different time points (rTMS–1, rTMS–2, Week 1, Week 2: F [3]=14.72, p<0.0005).
Part A: Analysis of Differences Within Each Group Over Time
Group 1 HAM-D scores differed significantly over time (F [3, 9]=47.22, p<0.0005). A post hoc modified Bonferroni analysis for all possible comparisons yielded significant differences (p<0.01) in HAM-D change scores between rTMS–Week 2, Follow-up Week 1, and Follow-up Week 2, when compared to rTMS–Week 1.
Group 2 HAM-D scores did not differ significantly (p>0.05) over time when all time points were compared.
Group 3 HAM-D scores differed significantly over time (F [3, 9]=21.49, p<0.0005), like Group 1. Here, a post hoc modified Bonferroni analysis for all possible comparisons also yielded significant differences (p<0.05) in HAM-D change scores between rTMS–Week 2, Follow-up Week 1, and Follow-up Week 2, when compared with rTMS–Week 1.
Group 4 HAM-D scores did not differ significantly (p>0.05) over time when all time points were compared.
Part B: Analysis of Differences Between Groups Over Time
HAM-D percent change scores were significantly different between the groups at all time points after baseline (rTMS–Week 1, p=0.018; rTMS–Week 2, p=0.0001; Follow-up Week 1, p=0.0001; Follow-up Week 2, p=0.0001).
These results were broken down using a post hoc modified Bonferroni analysis. Group 1 differed significantly from both Group 2 and Group 4 at time points rTMS–Week 2, Follow-up Week 1, and Follow-up Week 2 (all p<0.0005). We found similar results for Group 3, with significant differences compared to Group 2 and Group 4 found at time points rTMS–Week 2 , Follow-up Week 1 and Follow-up Week 2 (all p<0.0005). There were no differences between Group 2 and Group 4 (sham) at any time point. Also, there were no differences between Group 1 and Group 3 at any time point.
Finally, we found no correlation between baseline HAM-D scores, gender, age, or prior history of hospitalizations or ECT and subsequent improvement.
Withdrawals and Adverse Effects
A total of eight patients withdrew from the study due to adverse effects. These patients were from Group 2 (five patients) and Group 4 (three patients). No patients withdrew from Group 1 or Group 3, which were the groups showing a significant antidepressant effect. All subjects tolerated the procedure without any major complication; specifically, none of the patients experienced a seizure.
One patient complained of severe headaches on four occasions during the 10 days of rTMS and was prescribed analgesics (acetaminophen or aspirin). This patient requested release from the study at the end of the second week of rTMS. This patient was in Group 4a, receiving sham, left-sided high frequency rTMS.
While no other patients required analgesia, nine of the 45 patients reported headaches which they rated subjectively as “severe” on at least one of the days of rTMS. These headaches always subsided without treatment within a few hours of rTMS. There was no correlation between headaches and eventual antidepressant effects.
Optimal Stimulation Parameters for rTMS Treatment of Depression
The findings of this study confirm the results of previous sham-controlled trials of rTMS in depression 14 , 15 in finding antidepressant effects of rTMS in patients with major depressive disorder. Both high frequency left-sided rTMS and low frequency right-sided rTMS led to a clinically significant antidepressant effect (≥50% reduction in the HAM-D score) in 60% of patients. The magnitude of this effect is similar to the results in our previous trial 15 and greater than some other published reports. 22 This difference in degree might be related to differences in the rTMS parameters. In our studies, we have used both a higher stimulation intensity (110% in the present study) and a larger number of stimuli per session (1,600 in the present study) than most other reported studies. These parameters are now widely considered safe. 1
The main result of the present study is that low frequency rTMS to the right DLPFC has similar antidepressant effects to high frequency rTMS to the left DLPFC. These results confirm the findings of Fitzgerald et al. 18 In our previous sham-controlled trial of rTMS in depression, 15 right DLPFC rTMS at high frequency was found to lack antidepressant effects (and for this reason, this was not included as a treatment arm of the current study). In the present study, low frequency rTMS to the left DLFPC did not show antidepressant activity.
Though our study was not designed to assess the duration of the antidepressant effect of rTMS, it is worth noting that our unblinded follow-up at 4 weeks appeared to show an equal duration of antidepressant effect for both high frequency left-sided rTMS and low frequency right-sided stimulation.
If it is accepted that high frequency left-sided rTMS and low frequency right-sided stimulation are equally effective in the treatment of depression, factors other than efficacy must be taken into account when selecting a treatment modality. The most serious potential side effect of rTMS is seizure, and a growing body of evidence suggests that low frequency rTMS may be protective against seizures. 23 Therefore, low frequency rTMS should be the treatment of choice for patients with risk factors for epilepsy. On the other hand, high frequency treatment is better researched at present and may remain the first-line modality for some time.
Ultimately, it remains unclear whether some patients respond better to high freqeuncy left-sided rTMS and others to low frequency right-sided rTMS. Analysis of our data fails to reveal any obvious differences between the patients responding to one or another rTMS regimen. It is possible that by increasing activity on the left side, one may transcallosally suppress activity on the right and vice versa. Therefore, the physiological effects of high frequency left-sided and low frequency right-sided rTMS may, in fact, be equivalent. Alternatively, some characteristics may predispose patients to respond to one or the other modality. Our study did not address this issue. Fitzgerald et al. 18 attempted to investigate this with a crossover design in their study. Nonresponders to either high or low frequency treatments from the first leg of their study were given the alternate treatment. The patients were unblinded during their second phase of treatment, and some of the improvements measured might have had a placebo effect or a delayed response to the first phase of treatment. Of 17 patients crossed over, only three responded to the alternate treatment. It is not possible to come to a conclusion on this issue without more data.
Another hypothesis that remains to be adequately tested is that left-sided high frequency treatment and right-sided low frequency treatment might have an additive effect. Fitzgerald et al. 24 showed that this approach has efficacy in the treatment of major depressive disorder, but they compared it with placebo rather than with unilateral treatment, making comparison difficult.
The Mechanism of rTMS in the Treatment of Depression
Our results show that right and left hemispheric rTMS appear to lead to similar antidepressant effects only if disparate stimulation parameters are used. This finding is striking in the context of the results of unilateral ECT, which appears to have equivalent therapeutic value when applied to the right or left hemisphere. 25 , 26 One interpretation of these findings is that rTMS and ECT might have different mechanisms of action.
We believe the differing effects of high and low frequency stimulation represent differing neurophysiological responses. Applied to the motor cortex, high frequency rTMS results in an enhancement of excitability in most subjects, while low frequency rTMS leads to a transient cortical inhibition (or dysfacilitation). 3 Evidence from functional imaging supports the inference that the same differential effect of frequency occurs in the prefrontal cortex. Furthermore, these studies show that high and low frequency rTMS lead to completely different patterns of distal excitability and inhibition, affecting cortical and subcortical structures. 4 , 27 , 28
Though the evidence linking high and low frequency TMS with excitability and suppression, respectively, is strong, it is not the case that this mechanism has been conclusively proven to be responsible for the antidepressant effect of TMS. For example, some studies have associated antidepressant TMS with an increase in brain derived neurotrophic factors (BDNF), 29 although other studies demonstrate contradictory findings. 30
Study Limitations
Our study was relatively small (N=45), although the results were statistically significant.
There is no perfect control condition for rTMS. Both sham coils and real coils held at noneffective angles have limitations. However, we have data showing that both are effective controls in subjects who are naïve to TMS, as our patients were (Pascual-Leone, unpublished).
Finally, we now believe that 10 days of stimulation is suboptimal. The antidepressant effects appear to continue to grow for up to 20 days. 31 Nonetheless, the effect size in this particular population of patients is quite large. However, it is important to note that there is substantial variability in this regard. For review, see Mitchell and Loo. 22
CONCLUSIONS
This study demonstrates that high frequency rTMS to the left DLPFC and low frequency rTMS to the right DLPFC are both effective in the treatment of depression, while sham TMS and low frequency rTMS to the left DLPFC are ineffective.
1. Machii K, Cohen D, Ramos-Estebanez C, et al: Safety of rTMS to nonmotor cortical areas in healthy participants and patients. Clin Neurophysiol 2006; 117:455–471Google Scholar
2. Chen R, Classen J, Gerloff C, et al: Depression of motor cortex excitability by low-frequency transcranial magnetic stimulation. Neurology 1997; 48:1398–1403Google Scholar
3. Pascual-Leone A, Tormos JM, Keenan J, et al: Study and modulation of human cortical excitability with transcranial magnetic stimulation. J Clin Neurophysiol 1998; 15:333–343Google Scholar
4. Loo CK, Sachdev PS, Haindl W, et al: High (15Hz) and low (1Hz) frequency transcranial magnetic stimulation have different acute effects on regional cerebral blood flow in depressed patients. Psychol Med 2003; 33:997–1006Google Scholar
5. Speer AM, Kimbrell TA, Wassermann EM, et al: Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biol Psychiatry 2000; 48:1133–1141Google Scholar
6. Baxter LR Jr, Schwartz JM, Phelps ME, et al: Reduction in left prefrontal cortex glucose metabolism common to three types of depression. Arch Gen Psychiatry 1989; 46:243–250Google Scholar
7. Buchsbaum MS, Wu J, DeLisi LE, et al: Frontal cortex and basal ganglia rates assessed by positron emission tomography with (fluorine-18) 2-deoxyglucose in affective illness. J Affect Dis 1986; 10:137–152Google Scholar
8. Drevets WC, Price JL, Simpson JR Jr, et al: Subgenual prefrontal cortex abnormalities in mood disorders. Nature 1997; 386:824–827Google Scholar
9. Drevets WC, Videen TO, Preskorn SH, et al: A functional neuroanatomical study of unipolar depression. J Neurosci 1992; 12:3628–3641Google Scholar
10. George MS, Ketter TA, Post RM: Prefrontal cortex dysfunction in clinical depression. Depression 1994; 2:59–72Google Scholar
11. Martinot JL, Hardy P, Feline A, et al: Left prefrontal glucose hypometabolism in the depressed state: a confirmation. Am J Psychiatry 1990; 147:1313–1317Google Scholar
12. Avery DH, Holtzheimer PE III, Fawaz W, et al: A controlled study of repetitive transcranial stimulation in medication-resistant major depression. Biol Psychiatry 2006; 59:187–194Google Scholar
13. George MS, Wassermann EM, Williams WA, et al: Daily repetitive transcranial magnetic stimulation (rTMS) improves mood in depression. Neuroreport 1995; 6:1853–1856Google Scholar
14. George MS, Wassermann EM, Kimbrell TA, et al: Mood improvement following daily left prefrontal repetitive transcranial magnetic stimulation in patients with depression: a placebo controlled crossover trial. Am J Psychiatry 1997; 154:1752–1756Google Scholar
15. Pascual-Leone A, Rubio B, Pallardó F, et al: Rapid-rate transcranial magnetic stimulation of left dorsolateral prefrontal cortex in drug-resistant depression. Lancet 1996; 348:233–237Google Scholar
16. Rossini D, Lucca A, Zanardi R, et al: Transcranial magnetic stimulation in treatment-resistant depressed patients: a double-blind, placebo controlled trial. Psychiatry Res 2005; 137:1–10Google Scholar
17. Kauffmann CD, Cheema MA, Miller BE: Slow right prefrontal transcranial magnetic stimulation as a treatment for medication-resistant depression: a double-blind, placebo-controlled study. Depress Anxiety 2004; 19:159–162Google Scholar
18. Fitzgerald PB, Brown TL, Marston NA, et al: Transcranial magnetic stimulation in the treatment of depression: a double-blind, placebo-controlled trial. Arch Gen Psychiatry 2003; 60:1002–1008Google Scholar
19. Rossini PM, Berardelli A, Deuschl G, et al: Applications of magnetic cortical stimulation: The International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol 1999; 52:171–185Google Scholar
20. Wassermann EM: Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5–7, 1996. Electroencephalogr Clin Neurophysiol 1998; 108:1–16Google Scholar
21. Hamilton M: Development of a rating scale for primary depressive illness. Br J Soc Clin Psychology 1967; 6:278–296Google Scholar
22. Mitchell PB, Loo CK: Transcranial magnetic stimulation for depression. Aust N Z J Psychiatry 2006; 40:406–413Google Scholar
23. Theodore WH, Hunter K, Chen R, et al: Transcranial magnetic stimulation for the treatment of seizures: a controlled study. Neurology 2002; 59:560–562Google Scholar
24. Fitzgerald PB, Benitez J, de Castella A, et al: A randomized, controlled trial of sequential bilateral repetitive transcranial magnetic stimulation for treatment-resistant depression. Am J Psychiatry 2006; 163:88–94Google Scholar
25. Abrams R: Electroconvulsive Therapy, 3rd ed. New York, Oxford University Press, 1997Google Scholar
26. Abrams R, Swartz CM, Vedak C: Antidepressant effects of right versus left unilateral ECT and the lateralization theory of ECT action. Am J Psychiatry 1989; 146:1190–1192Google Scholar
27. Speer AM, Kimbrell TA, Wassermann EM, et al: Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biol Psychiatry 2000; 48:1133–1141Google Scholar
28. Wassermann EM, Grafman J, Paus T: Combining transcranial magnetic stimulation and neuroimaging to map the brain. Trends Cogn Neurosci 1997; 1:199–201Google Scholar
29. Yukimasa T, Yoshimura R, Tamagawa A, et al: High frequency repetitive transcranial magnetic stimulation improves refractory depression by influencing catecholamine and brain-derived neurotrophic factors. Pharmacopsychiatry 2006; 39:52–59Google Scholar
30. Lang UE, Bajbouj M, Gallinat J: Brain-derived neurotrophic factor serum concentrations in depressive patients during vagus nerve stimulation and repetitive transcranial magnetic stimulation. Psychopharmacology 2006; 187:56–59Google Scholar
31. Gershon AA, Dannon PN, Grunhaus L: Transcranial magnetic stimulation in the treatment of depression. Am J Psychiatry 2003; 160: 835–845Google Scholar



