Neuropsychological Evidence of Impaired Cognitive Empathy in Euthymic Bipolar Disorder
Another ability related to empathy is “Theory of Mind,” which can be defined as the ability to understand the feelings, intentions, and motivations of others. 7 Currently there is a lack of a clear distinction between empathy and the theory of mind concept, leading some researchers to use these terms interchangeably. 6 , 8 It appears that theory of mind is roughly equivalent to cognitive empathy, but not to “affective empathy.”
Recent findings indicate that an impaired theory of mind may account for the aberrant social behaviors exhibited by bipolar disorder. 9 , 10 Kerr et al. 11 reported impairment in performance on first- and second-order theory of mind tasks in bipolar depressive and bipolar manic patients, but not in remitted patients. However, more recently, Bora et al. 12 proposed that even euthymic bipolar disorder patients may be impaired in advanced theory of mind tasks.
We have recently suggested that, similar to empathy, theory of mind could also be divided into cognitive and affective components. 13 It was assumed that while “cognitive theory of mind” refers to our ability to make inferences regarding other people’s beliefs, “affective theory of mind” refers to the inferences one makes regarding others’ emotions. While “cognitive theory of mind” is very similar to “cognitive empathy,” “affective theory of mind” may be related to both cognitive and affective empathy. It appears that the centrality of emotion distinguishes between the affective and cognitive aspects of empathy and theory of mind.
Cognitive empathy has been shown to depend on intact ventromedial prefrontal cortical functioning. 14 Interestingly, ventromedial prefrontal cortical dysfunction has been reported in bipolar disorder. 15 Furthermore, recent research indicates that many of the core features of bipolar disorder overlap with those known to characterize frontal lobe syndrome. 16 Additionally, it has been suggested that bipolar disorder patients show impairment in frontal neurocognitive tasks that involve cognitive flexibility. 17 On the other hand, the neuroanatomical basis of affective empathy is largely unknown and could relate to more limbic structure function such as the amygdala. 18 Thus, we hypothesized that euthymic bipolar disorder patients would show impaired cognitive empathy while showing preserved affective empathy.
To date, there have been no studies looking at the relationship between either cognitive or affective empathy and cognitive and affective theory of mind, leaving unsettled whether these terms are equivalent or not. Therefore, to more fully understand the nature of empathy in bipolar disorder, the relationship between empathy and theory of mind was also examined. Additionally it was hypothesized that impaired cognitive empathy in bipolar disorder would be related to performance on cognitive flexibility tasks that assess prefrontal cortical functioning.
METHODS
Participants
Nineteen patients (10 males, 9 females) diagnosed with bipolar disorder were recruited from new admissions to the affective disorder program in the Shalvata Mental Health Center. Remission criteria for bipolar disorder patients (euthymia) were defined as a rating of ≤9 on the Hamilton Depression Rating Scale (HAM-D); ≤7 on the Young Mania Rating Scale (YMRS); and a self-report by the patient and confirmation by at least one family member that the patient was in remission (Table 1) .
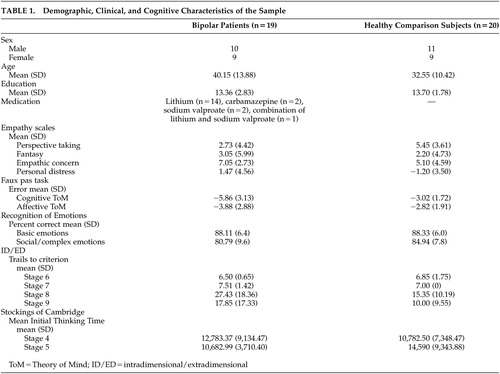 |
The inclusion criteria for patients were ages between 18 and 60 years; stable medication intake during the preceding month (as confirmed by the clinical staff and/or a family member); DSM-IV diagnosis of bipolar disorder, and monitoring of blood levels of mood stabilizers. The exclusion criteria were any acute, unstable, significant, or untreated medical illness, neurological disorders, mental retardation, and current drug abuse. Bipolar disorder patients were excluded if they had been diagnosed as having a psychotic episode or other axis I diagnosis of mental disorder for the index episode. Two bipolar disorder patients had a comorbid personality disorder: one an adjustment disorder and the other a borderline personality disorder. Only patients with bipolar I disorder and with no history of psychosis were included. All bipolar disorder patients were receiving psychiatric medication, mainly mood stabilizers (nine patients taking lithium, six patients taking carbamazepine, four patients taking sodium valproate). The blood levels of the mood stabilizers for all patients were within the therapeutic range: lithium 0.5–1.2 nmol/liter, carbamazepine 6–10 mg/liter, and sodium valproate 60–100 mg/liter. Only outpatients were included in the sample.
Twenty age- and gender-matched healthy comparison volunteers (11 men, 9 women) were recruited by advertisement. The healthy comparison subjects had no known psychiatric or current drug/alcohol problem (according to the Structured Clinical Interview for DSM-IV-TR). They also denied having any first-degree relatives with a psychiatric history (self-report).
The study was conducted in accordance with the local institutional review board committee. Study candidates were given a detailed description of the study and signed a written informed consent. One patient refused to complete the theory of mind task.
Measures
Assessment of Empathic Abilities
The cognitive and affective aspects of empathic abilities were assessed using the Interpersonal Reactive Index. 3 The Interpersonal Reactive Index includes four seven-item subscales, each tapping a different aspect of empathy 3 : (a) the perspective taking subscale, which measures the reported tendency to adopt spontaneously the psychological point of view of others; (b) the fantasy subscale, measuring the tendency to imaginatively transpose oneself into fictional situations; (c) the empathic concern scale, measuring the tendency to experience feelings of sympathy and compassion for others; and (d) the personal distress scale assesses the tendency to experience distress and discomfort in response to others’ observed distress. The scales have previously been adapted to Hebrew and validated with Hebrew speaking Israeli population. Scoring ranged from −2 to +2 for each item.
It has been suggested that while the perspective-taking subscale of the Interpersonal Reactive Index clearly assesses cognitive empathy, the personal distress scale taps prominently affective empathy. Reliability analysis (split-half reliability), in the present study, of the scales yielded high reliability coefficients for both the cognitive scale (α=0.79) and for the affective empathy scale (α=0.82).
Assessment of Cognitive and Affective Theory of Mind
Understanding “Faux Pas”
A faux pas occurs when a speaker says something without considering that the listener might not want to hear it or may be hurt by what has been said. Detection of a faux pas requires both an understanding that there might be a difference between a speaker’s knowledge state (cognitive theory of mind) and that of the listener, and an appreciation of the emotional impact of a statement on the listener (affective theory of mind).
To evaluate the ability of participants to recognize a social faux pas, we used a Hebrew version of a task designed by Baron-Cohen et al. 19 consisting of 20 stories presented in random order. A faux pas occurred in 10 of them, while the remaining 10 served as control stories. Participants were then asked theory of mind questions and control questions (tapping story comprehension).
The score for every item (error score) was divided into two components. Each error received a −1 score. The “Recognition of Faux Pas” component consisted of the score of the first two questions (“Did someone say something he should not have said?” “Who said it?”). The reliability (split-half reliability) of this component was high (α=0.96). In the 10 control stories, the correct answer to the first question was “no” and no further questions were asked if answered correctly. If participant answered “yes,” this item would be scored as “false alarm” and get error scores for each wrong answer. The second, “Understanding of Faux Pas” (reliability, α=0.86), referred to the subject’s ability to understand exactly what went wrong in the story by answering two other questions: an affective theory of mind question (“What was wrong with what that person said?”) and cognitive theory of mind question (“Why did she say it?”). In both components, the scores were calculated based on the number of errors that subjects had on both test and control items. The control items were not included in the final scoring and were only used as distracters and for exclusions of subjects with major cognitive disabilities. No subject in the sample was excluded due to impaired performance in these control items.
Recognition of Basic versus Social Eye Expressions
This computerized task was designed to assess the ability to recognize basic emotions versus social emotions. The test consists of 52 photographs of eyes showing six basic emotions taken from Ekman and Friesen 20 : happy, sad, afraid, surprised, distressed, disgusted, and angry (reliability of this classification was good, α=0.61). The reliability (split-half reliability) of this component was high (α=0.96). The test also showed seven “social emotions” (reliability α=0.49) based on Baron-Cohen et al. 21 : interested, worried, confident, fantasizing, preoccupied, friendly, and suspicious. Two words were printed at the bottom of each picture stimulus, with one word describing the correct emotion expressed in the eyes and the other a distracter. Correct and incorrect responses were scored as 1 and 0, respectively. A total mean score for the basic and social emotions scores was calculated.
Neurocognitive Assessment of Prefrontal Cortical Functioning
Participants were administered subsets from the Cambridge Neuropsychological Test Automated Battery (CANTAB), a computer-administered nonverbal battery of tasks designed to examine specific aspects of cognition, associated particularly with prefrontal cortical functioning. 22
Cognitive Flexibility: The ID/ED Shifting Task
This task assesses subject’s ability to attend to the specific attributes of compound stimuli (rule acquisition) and to shift that attention when required. Two artificial dimensions and two stimuli are displayed, initially each of only one dimension. These shifts are initially intradimensional, then later extradimensional (ID/ED). The task involves simple shifts as well as reversal. This test was associated to the prefrontal cortex. Specifically, dorsolateral prefrontal cortical was related to extradimensional shifts stages (stage 8) 23 while reversal stages (stage 7-simple reversal and stage 9 extradimensional reversal) were associated with the orbitofrontal/ventromedial prefrontal region. 24 Using the method administered by Ozonoff et al., 25 when participants failed to achieve criterion (six consecutive correct responses) at a given stage, the test was failed and the maximum number of errors (25) and trials (50) was recorded for all subsequent stages not administered (reliability of the stages was 0.552).
Planning: The Stockings of Cambridge Task
A spatial planning test based upon the Tower of London test. The subject is shown two displays containing three colored balls. In each trial, the subject must move the balls in the lower display to copy the pattern shown in the upper. A later motor control task, in which the subject simply copies earlier moves, allows planning time to be calculated (reliability, α=0.788). Among other regions, this test is strongly associated with the dorsolateral prefrontal cortex. 26
RESULTS
The bipolar disorder and the healthy comparison groups did not differ in age (t =−1.94, df=37, n.s.) or years of education (t=0.44, df=37, n.s.).
Cognitive and Affective Empathy
Bipolar disorder patients had significantly lower scores on the cognitive empathy subscale (perspective-taking), (t=2.102, df=37, p=0.042). However, patients scored significantly higher than controls on the affective empathy subscale (personal distress) (t=−2.059, df=37, p=0.047). No significant differences were observed in the empathic concern (t=−1.561, df=37, n.s.) and fantasy scale (t=−0.494, df=37, n.s).
To examine the interaction between group (bipolar disorder patients, comparison subjects) and empathy subtype (cognitive, affective), a repeated measures analysis of variance (ANOVA) (empathy subtype, with group as between-subjects factor) was conducted with the cognitive (perspective-taking) and affective (fantasy scale) scales. As observed in Figure 1 , this analysis revealed a significant type effect (F =15.460, df=1, 37, p=0.0001), a significant group-by-type interaction effect (F=7.164, df= 1, 37, p=0.011), and a nonsignificant group effect (F=0.001, df=1, 37, n.s.). This suggested that the pattern of performance in the cognitive and affective empathy scores was significantly different between the two groups: whereas cognitive empathy was higher in healthy comparison subjects, bipolar patients showed a trend toward higher emotional empathy.
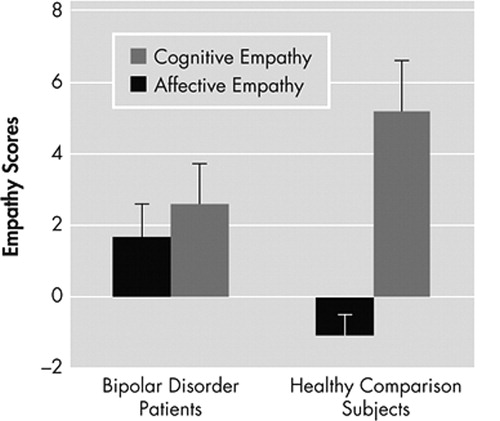
A significant group by type (interaction) effect (F=7.164, df=1, 37, p=0.011) indicated that the pattern of performance in the cognitive and affective empathy scores was significantly different between the two groups. Follow-up independent T-test indicated that bipolar disorder patients had significantly lower scores in the cognitive empathy subscale (perspective-taking) (t=2.102, df=37, p=0.042). However, patients scored significantly higher than comparison subjects on the affective empathy subscale (personal distress) (t=−2.059, df=37, p=0.047).
To rule out the possibility that different medication type affected the results, we divided the patient group into three groups according to their medications (nine patients taking lithium, six patients taking carbamazepine, four patients taking sodium valproate). One-way ANOVA indicated that the subgroups of patients did not differ in their cognitive (F=3.131, df=2, 16, n.s.) or affective empathy (F=0.690, df=2, 16, n.s.).
Cognitive and Affective Faux Pas
In order to compare the cognitive and affective theory of mind scores of patients and comparison subjects, independent sample t tests were conducted for recognition of faux pas, as well as cognitive and affective understanding of faux pas. Significant differences were evident in the cognitive faux pas variable (t=−3.502, df=36, p=0.001), with better performance of the healthy comparison subjects than the bipolar disorder group. Interestingly, no significant differences between the healthy comparison subjects and the bipolar patients were found in the affective faux pas scores (t=1.531, df=36, n.s.) in the “false alarm” scores (t=1.531, df=36, n.s.) or in the recognition of faux pas (t=1.676, df=36, n.s.).
A repeated measures ANOVA was conducted, with type (affective versus cognitive theory of mind) as the within-subjects factor and group as the between-subjects factor. As observed in Figure 2 , this analysis revealed a significant group effect (F=6.649, df=1, 36, p=0.014) and a significant type effect (F=17.805, df=1, 36, p=0.0001), indicating significant differences in performance between groups and between types (cognitive, affective) of theory of mind. A significant group-by-type interaction effect (F=11.910, df=1, 36, p=0.001) was found, indicating that the pattern of performance reflected in the cognitive and affective theory of mind scores was significantly different between the two groups.
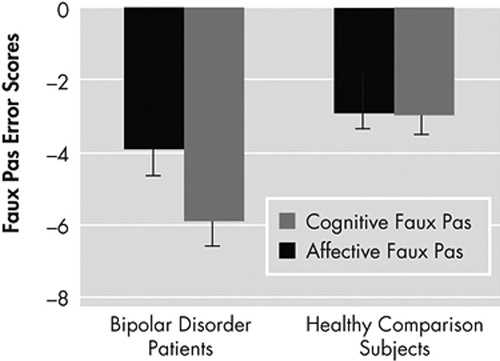
A significant group effect (F=6.649, df=1, 36, p=0.014), a significant type effect (F=17.805, df=1, 36, p=0.0001), and a significant group by type (interaction) effect (F=11.910, df=1, 36, p=0.001) were found. Follow-up independent T-tests indicated that significant differences were evident in the cognitive faux pas variable (t=−3.502, df=36, p=0.001), but not in the affective faux pas scores (t=1.531, df=36, n.s.).
One way ANOVA of the three medication subgroups indicated that the subgroups of patients did not differ in their cognitive (F=0.368, df=2, 16, n.s.) or affective theory of mind (F=0.993, df=2, 16, n.s.) abilities.
The Relationship between Cognitive and Affective Empathy and Theory of Mind
To assess the associations between measures of cognitive empathy, affective empathy, and theory of mind (affective and cognitive), we evaluated the correlations between the cognitive (perspective-taking) and the affective (personal distress) scales of the Interpersonal Reactive Index and the affective and cognitive faux pas in the entire sample and in each group separately. Correlational analysis between variables on the entire sample indicated that the cognitive empathy scale correlated significantly with the cognitive theory of mind scale (r=0.366, p=0.024) as well as the affective theory of mind scale (r=0.357, p=0.028). On the other hand the affective empathy scale did not correlate with the cognitive theory of mind (r=−0.017, n.s.) nor with the affective theory of mind scale (r=0.083 n.s.).
In the bipolar disorder patients, cognitive empathy scale correlated significantly with the affective theory of mind scale (r=0.475, p=0.046) but not with the cognitive theory of mind scale (r=0.285, n.s.). The affective empathy scale did not correlate with the cognitive theory of mind (r=−0.341, n.s.) nor with the affective theory of mind scale (r=0.291 n.s.).
In the healthy comparison group, cognitive empathy scale did not correlate significantly with the cognitive theory of mind scale (r=0.191, n.s.) nor with the affective theory of mind scale (r=0.037, n.s.). The affective empathy scale did not correlate with the cognitive theory of mind scale (r=−0.162, n.s.) nor with the affective theory of mind scale (r=−0.053 n.s.).
Recognition of Basic Emotions and Mentalizing Emotions (Reading the Mind in The Eyes)
Independent samples t tests revealed no significant differences between groups in the measure of basic emotions (t=0.111, df=35, n.s.) or mentalizing/social emotions (t=1.428, df=35, n.s.), indicating that bipolar disorder patients are not impaired in recognizing basic and complex emotions.
Neurocognitive Assessment of Prefrontal Cortical Functioning
Cognitive Flexibility: Intradimensional/Extradimensional Task
The primary variables of interest were the number of trials taken to reach criterion at stages 6 (intradimensional shift), 7 (reversal of the intradimensional shift), 8 (extradimensional shift), and 9 (reversal of the extradimensional shift) of the task. In order to obtain a measure of the trends over the different stages, a repeated measures analysis of variance (ANOVA) was conducted, with stage as the within subjects factor and group as the between-subjects factor. As evident in Figure 3 , analysis was carried out for the trials to criterion variable for stages 6–9. This analysis revealed a significant group effect (F=5.951, df=1, 37, p=0.020), a significant stage effect (F=13.349, df=3, 35, p=0.0001) and a significant (marginal) group by stage effect (F=2.761, df=3, 35, p=0.057).
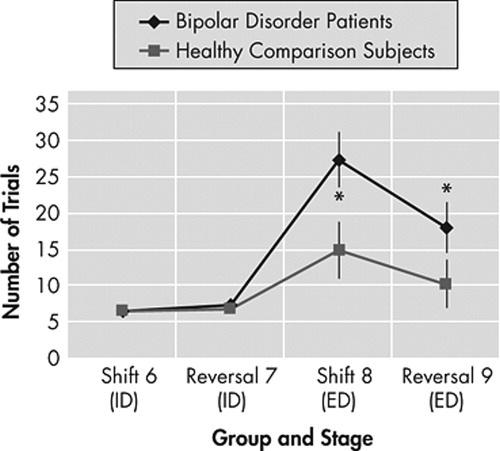
The primary variables of interest were the number of trials taken to reach criterion at stages 6 (intradimensional shift), 7 (reversal of the intradimensional shift), 8 (extradimensional shift), and 9 (reversal of the extradimensional shift) of the task. Rrepeated measures ANOVA revealed a significant group effect (F=5.951, df=1, 37, p=0.020), a significant stage effect (F=13.349, df=3, 35, p=0.0001) and a significant (marginal) group by stage effect (F=2.761, df=3, 35, p=0.057).
Follow-up t-tests showed that that the two groups did not differ significantly in the number of trials made on stage 6, but did differ in stages 8 (t=2.558, df=37, p=0.018) and marginally in stage 9 (t=1.764, df=37, p=0.08)
Follow-up t tests showed that that the two groups did not differ significantly in the number of trials made on stages 6 (t=−0.808, df=37, n.s.) and 5 (t=1.610, df=37, n.s.). However, the bipolar disorder group made significantly more trials until reaching criterion in stages 8 (t=2.558, df=37, p=0.018) and marginally in stage 9 (t=1.764, df=37, p=0.08).
Planning: Stocking of Cambridge Task
An independent sample t test revealed the bipolar disorder group did not need more time (Mean Initial Thinking Time) to solve each of the four (t=−0.748, df=36, n.s.), and five-move problem (t=1.617, df=36, n.s.), than the comparison group, as measured by the “Mean Moves” variables.
The Relationship between Empathy and Executive Functions in Bipolar Disorder
A correlation analysis was done in order to explore the relation between scores on the empathy scales and performance on the intradimensional/extradimensional and Stocking of Cambridge tasks. In the patient group, this analysis revealed significant negative correlations only between cognitive empathy and intradimensional/extradimensional reversal scores (tapping on orbitofrontal performance) in stage 7 (r=−0.432, p=0.037) but not with the shifting scores (tapping dorsolateral performance) or in stage 9. The lower participants’ cognitive empathy scores were, the more trials they needed to reach the reversal criterion. Empathy scores did not significantly correlate with the Stocking of Cambridge task.
DISCUSSION
The current study assessed the empathic and theory of mind abilities as well as executive functions of bipolar patients relative to healthy comparison subjects. As we hypothesized, bipolar patients showed impaired cognitive empathy and theory of mind. Impaired theory of mind has previously been reported in euthymic bipolar patients. 10 , 12 However, a selective deficit in cognitive theory of mind and empathy has never before been reported in bipolar disorder. Using the Interpersonal Reactive Index, a multidimensional measure of empathy, we demonstrated that although individuals with bipolar disorder scored lower than healthy comparison subjects on measures of cognitive empathy (perspective-taking), they scored higher than healthy comparison subjects on the personal distress scale, which is an affective scale. To the best of our knowledge, this is the first time that affective empathy has been measured at the same time as cognitive empathy in a group of patients with bipolar disorder.
Deficits in attentional control and executive functioning 27 in this population are consistent with dysfunction in frontal and striatal brain network. 28 Furthermore, in accordance with previous reports, 17 bipolar disorder patients were impaired in the intradimensional/extradimensional task of cognitive flexibility, a cognitive ability that is usually associated with cognitive empathy. 29 Patients did not show impaired planning ability. Furthermore, their impaired cognitive empathy was related with the reversal stages (only stage 7) rather than other measures of executive functions. It has been suggested that damage to the orbitofrontal cortex can impair the learning and reversal of stimulus-reinforcement associations, and thus the correction of behavioral responses. 30 Interestingly, impaired cognitive empathy has also previously been reported in patients with ventromedial prefrontal damage. 14 Thus, additional corroboration for the concept of impaired cognitive empathy in bipolar disorder arises from the comparable neuroanatomical foundations of social cognition dysfunction and bipolar disorder.
According to Davis, 4 the cognitive Interpersonal Reactive Index scales evaluate the likelihood that someone will engage in the process of attempting to reflect on the viewpoint of others. The present study results suggest that these processes are impaired in bipolar disorder. On the second affective scale, personal distress, the bipolar disorder group actually scored significantly higher than healthy comparison subjects (the empathic concern scores were also higher, but not significantly). This indicates a greater tendency to have self-oriented feelings of anxiety and discomfort in response to tense interpersonal settings. Although this could be interpreted as a demonstration of greater empathy, it should be noted that individuals with bipolar disorder have been reported to have higher levels of anxiety in general, 31 which may have increased personal distress scores.
Furthermore, these findings support recent studies on emotion perception in bipolar disorder, showing impairments in the capacity to inhibit emotional response. 32 Indeed, it has been suggested that these patients tend to overactivate limbic regions during the appraisal of emotional material, 33 which may evoke the generation of extreme emotional responses that are difficult to regulate. 34 It may be speculated that this lack of regulation of emotion and hyperactivation of the amygdala may account for the “hyper empathy,” which could be expressed in a dysfunctional empathic emotional overreaction. Thus, this exaggerated emotional response to others may be expressed in a dysfunctional empathic emotional overreaction (or “hyper empathy”).
This notion is consistent with the “simulation” theory, 35 according to which individuals impersonate others’ emotional mental states, using their own mental state. Thus, it may be hypothesized that bipolar disorder patients tend to engage in the “oversimulation” of others’ emotions, as reflected in high affective empathy, and as a result, they tend to misinterpret others’ mental states, which is reflected in impaired cognitive empathy and theory of mind.
Contrary to the findings of Bora et al., 12 patients in the present study were not impaired in recognizing complex social emotions. It may be speculated that since the eye stimuli used in the present study had only one distracter, rather than three as described in Bora et al., 12 this task was easier. However, these results are consistent with the general tendency of bipolar patients in the present study to perform better in emotional tasks than in cognitive empathy tasks.
The results of the present study also contradict those of Kerr et al., 11 who reported impaired theory of mind only in patients with currently symptomatic bipolar mania or depression. In line with Bora et al., 12 it may be concluded that cognitive empathy deficits in bipolar disorder may be regarded as a trait - rather than a state -dependent characteristic. This notion corroborates previous reports regarding theory of mind impairments in remitted patients with affective disorders. 36
Several limitations of the study need to be acknowledged. First, the small number of patients and lack of comprehensive IQ assessment limit the statistical power of the results. Additionally, although the majority of empathy studies to date have used questionnaires that evaluate empathic abilities, the use of self-rating scales may be problematic in patients. Surprisingly, while in the entire sample the cognitive empathy scale correlated with both cognitive and affective theory of mind, in the bipolar disorder group the cognitive empathy scale correlated only with affective theory of mind. While this lack of consistency between cognitive theory of mind and cognitive empathy may question the division of cognitive and affective theory of mind and empathy, we have recently suggested that affective theory of mind is actually an integral part of the cognitive empathic system. Thus, it appears that although the simulation perspective may explain emotional empathic processing, theory of mind processes may underlie cognitive empathy. 37
In addition, although it has been suggested that, at least in schizophrenia, an association of social cognition and medication is unlikely, 38 there are considerable variations in the medications given to bipolar disorder patients, differently affecting their brains and influencing their symptom level. In the present study we found that medication type did not have a differential effect on levels of empathy and theory of mind. Furthermore, the finding that bipolar patients show selective cognitive empathic and theory of mind deficits further identifies their empathic impairments as a core trait related to this disorder.
1 . Altshuler LL, Ventura J, Van Gorp WG, et al: Neurocognitive function in clinically stable men with bipolar I disorder or schizophrenia and normal control subjects. Biol Psychiatry. 56 2004; 8:560–569Google Scholar
2 . Goswami U, Sharma A, Khastigir U, et al: Neuropsychological dysfunction, soft neurological signs and social disability in euthymic patients with bipolar disorder. Br J Psychiatry 2006; 188:366–373Google Scholar
3 . Davis MH: Measuring individual differences in empathy: evidence for a multidimensional approach. J Pers Soc Psychol 1980; 44:113–126Google Scholar
4 . Davis MH: Empathy: A Social Psychological Approach. Dubuque, Iowa, Wm. C. Brown Communications, 1994Google Scholar
5 . Shamay-Tsoory SG, Shur S, Harari H, et al: Neurocognitive basis of impaired empathy in schizophrenia. Neuropsychology 2007; 21:431–438Google Scholar
6 . Baron-Cohen S, Wheelwright S, Hill J, et al: The “Reading the Mind in the Eyes” Test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. J Child Psychol Psychiatry 2001; 42:241–251Google Scholar
7 . Premack D, Woodruff G: Does the chimpanzee have a “theory-of-mind”? Behav Brain Sci 1978; 4:515–526Google Scholar
8 . Kaland N, Moller-Nielsen A, Callesen K, et al: A new “advanced” test of theory of mind: evidence from children and adolescents with Asperger syndrome. J Child Psychol Psychiatry 2002; 43:517–528Google Scholar
9 . Doody GA, Gotz M, Johnstone EC, et al: Theory of mind and psychoses. Psychol Med 28:397, 1998Google Scholar
10 . Olley AL, Malhi GS, Bachelor J, et al: Executive functioning and theory of mind in euthymic bipolar disorder. Bipolar Disord 2005; 5:43–52Google Scholar
11 . Kerr N, Dunbar RI, Bentall RP: Theory of mind deficits in bipolar affective disorder. J Affect Disord 2003; 3:253–259Google Scholar
12 . Bora E, Vahip S, Gonul AS, et al: Evidence for theory of mind deficits in euthymic patients with bipolar disorder. Acta Psychiatr Scand 2005; 2:110–116Google Scholar
13 . Shamay-Tsoory SG, Aharon-Peretz J: Dissociable prefrontal networks for cognitive and affective theory of mind: a lesion study. Neuropsychologia 2007; 45:3054–3067Google Scholar
14 . Shamay-Tsoory SG, Tomer R, Berger BD, et al: Characterization of empathy deficits following prefrontal brain damage: the role of the right ventromedial prefrontal cortex. J Cogn Neurosci 2003; 3:324–337Google Scholar
15 . Blumberg HP, Stern E, Martinez D, et al: Increased anterior cingulate and caudate activity in bipolar mania. Biol Psychiatry 2000; 48:1045–1052Google Scholar
16 . DeMay MG, Palvic D, Miller BL: Bipolar disorder and the frontal lobes, in The Human Frontal Lobes: Functions and Disorders. Edited by Miller BL, Cummings JL. New York, Guilford Press, 2007, pp 614–620Google Scholar
17 . Borkowska A, Rybakowski JK: Neuropsychological frontal lobe tests indicate that bipolar depressed patients are more impaired than unipolar. Bipolar Disord 2001; 2:88–94Google Scholar
18 . Vollm BA, Taylor AN, Richardson P, et al: Neuronal correlates of theory of mind and empathy: a functional magnetic resonance imaging study in a nonverbal task. Neuroimage 2006; 1:90–98Google Scholar
19 . Baron-Cohen S, O’Riordan M, Stone V, et al: Recognition of faux pas by normally developing children and children with Asperger syndrome or high-functioning autism. J Autism Dev Disord 1999; 29:407–418Google Scholar
20 . Ekman P, Friesen WV: Pictures of Facial Affect. Palo Alto, Calif, Consulting Psychologists Press, 1976Google Scholar
21 . Baron-Cohen S, Jolliffe T, Mortimore C, et al: Another advanced test of theory of mind: evidence from very high functioning adults with autism or Asperger syndrome. J Child Psychol Psychiatry 1997; 38:813–822Google Scholar
22 . Robbins TW, James M, Owen AM, et al: Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia 1994 5:266–281Google Scholar
23 . Rogers RD, Andrews TC, Grasby PM, et al: Contrasting cortical and subcortical activations produced by attentional-set shifting and reversal learning in humans. J Cogn Neurosci 2000; 12:142–146Google Scholar
24 . Kringelbach ML, Rolls ET: Neural correlates of rapid reversal learning in a simple model of human social interaction. NeuroImage 2003; 20:1371–1383Google Scholar
25 . Ozonoff S, Cook I, Coon H, et al: Performance on Cambridge neuropsychological test automated battery subtests sensitive to frontal lobe function in people with autistic disorder: evidence from the collaborative programs of excellence in autism network. J Autism Dev Disord 2004; 34:139–150Google Scholar
26 . Owen AM, Doyon J, Petrides M, et al: Planning and spatial working memory: a positron emission tomography study in humans. Eur J Neurosci 1996; 2:353–364Google Scholar
27 . Larson ER, Shear PK, Krikorian R, et al: Working memory and inhibitory control among manic and euthymic patients with bipolar disorder. J Int Neuropsychol Soc 2005; 2:163–172Google Scholar
28 . Strakowski SM, Delbello MP, Adler CM: The functional neuroanatomy of bipolar disorder: a review of neuroimaging findings. Mol Psychiatry 2005; 1:105–116Google Scholar
29 . Eslinger PJ: Neurological and neuropsychological bases of empathy. Eur Neurol 1998; 39:193–199Google Scholar
30 . Rolls ET: The orbitofrontal cortex. Philos Trans R Soc Lond B Biol Sci 1996; 351:1433–1444Google Scholar
31 . Taylor CT, Hirshfeld-Becker DR, Ostacher MJ, et al: Anxiety is associated with impulsivity in bipolar disorder. J Anxiety Disord 2008; 22:868-876Google Scholar
32 . Murphy FC, Sahakian BJ, Rubinsztein JS, et al: Emotional bias and inhibitory control processes in mania and depression. Psychol Med 1999; 6:1307–1321Google Scholar
33 . Chen CH, Lennox B, Jacob R, et al: Explicit and implicit facial affect recognition in manic and depressed states of bipolar disorder: a functional magnetic resonance imaging study. Biol Psychiatry 2006; 1:31–39Google Scholar
34 . Green MJ, Cahill CM, Malhi GS: The cognitive and neurophysiological basis of emotion dysregulation in bipolar disorder. J Affect Disord 2007; 103:29-42Google Scholar
35 . Gallese V, Goldman A: Mirror neurons and the simulation theory of mind-reading. Trends Cogn Sci 1999; 12:493–501Google Scholar
36 . Inoue Y, Tonooka Y, Yamada K, et al: Deficiency of theory of mind in patients with remitted mood disorder. J Affect Disord 2004; 3:403–409Google Scholar
37 . Shamay-Tsoory SG: Empathic processing: its cognitive and affective dimensions and neuroanatomical basis, in The Social Neuroscience of Empathy. Edited by Decety J, Ickes W. Cambridge, Mass, MIT Press 2008Google Scholar
38 . Sarfati Y, Hardy-Bayle MC, Nadel J, et al: Attribution of mental states to others by schizophrenic patients. Cogn Neuropsychiatry 1997; 2:1–17Google Scholar



