A Study of Herbal Remedies for Memory Complaints
Introduction
In 2007, over 40% of individuals between 50 and 70 years old reported using complementary and alternative medicine, of which the ingestion of herbal preparations is a major facet. 2 The comparable figure in the 70–85 age range was 32.1%.
Overall, 12% of American adults use herbal supplements, and more than half of these people do not tell their physicians because of concern about a “hostile attitude.” 3 Gingko biloba, long touted as a treatment for cognitive impairment, was the sixth most commonly sold “natural product” in 2007. 2 It is possible that people may be purchasing this product in an effort to treat perceived memory dysfunction and that the decision to do so is made without any medical consultation. To better understand the use of herbal supplements for real or perceived memory loss, we explored the availability of various substances and the marketing approach to people seeking this kind of treatment for cognitive complaints.
METHODS
Two of the authors (EL and CY) individually entered stores that sell herbal supplements posing as consumers seeking treatment for a grandmother with the following clinical profile. She is a 65-year-old woman with complaints of memory problems and a history of hypertension. For months she has been forgetting phone numbers, appointments, and names. She has not seen her primary physician for 6 months and is taking no medications. There are no allergies.
The proprietor was asked for recommendations for this care. Five things were then noted:
| 1. | What herbal preparation was recommended? | ||||
| 2. | Were there any questions about medical history? | ||||
| 3. | Were potential side effects mentioned? | ||||
| 4. | What are the specific ingredients of the recommended brand? | ||||
| 5. | What was the price of the recommended treatment? | ||||
The proprietor was specifically asked about potential side effects if they had not been mentioned.
Thirty stores in the New York City borough of Manhattan were sampled. Of these, there were four categories of merchants: large chains (group 1, n=9); large individual health food stores (group 2, n=9); small countercultural herbal shops (group 3, n=6); and ethnic herbal apothecaries in Chinatown (group 4, n=6).
RESULTS
Recommended Substances
The most commonly recommended herb was gingko biloba, either alone (46.7% of total) or in a combination with other substances (13.3%). Phosphatidylcholine and phosphatidylserine, generally combined, were the second most commonly endorsed treatments (20%). Brands containing multiple herbs were highly popular, being recommended 33% of the time and most had either gingko, phosphatidylcholine/phosphatidylserine, or both.
Medical History
Medical history was inquired about in a small minority of establishments: one of nine in group 1; zero of nine in group 2; two of six in group 3; and four of six in group 4. Thus, seven of 30 stores asked about any medical issues.
Potential Side Effects
This information was offered by one of nine in group 1; zero of nine in group 2; three of six in group 3; and zero of four in group 4 (two of the group 4 stores refused to address the issue of side effects without a direct evaluation of the patient first). Overall, four out of 28 (14.3%) retailers offered information about any potential side effects. When the salespeople were specifically asked about side effects, this did not increase the number of warnings. Some sample responses include: “Herbs do not have side effects”; “No, it actually increased blood flow to the brain”; and “No one has come back complaining of anything.”
Specific Ingredients and Costs
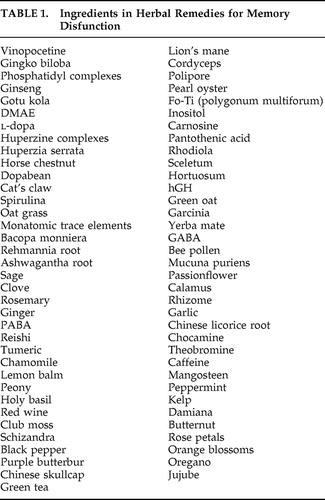
Table 1 lists all ingredients contained in the preparations recommended by the 30 sample stores. Monthly supplies of the supplements ranged from $4.99 to $199.
 |
DISCUSSION
This study documented which herbal remedies are most commonly recommended for the treatment of memory dysfunction and the degree of attention paid by merchants of these preparations to such medical issues as patient history and potential side-effect profiles.
The most highly recommended treatment, gingko biloba, has been found to be ineffective in large controlled studies of patients with cognitive impairment or as a preventive strategy in healthy elderly control subjects. 4 , 5 One study, in fact, suggested that gingko led to an excess number of hemorrhagic strokes. 4 Phosphatidylcholine showed no clinical benefit in 12 controlled trials in patients with dementia or subjective memory problems. 6 – 11 Likewise, results for phosphatidylserine have been disappointing, although scarcer. 12 – 14 The fact that one-third of recommended treatments contained multiple substances is of concern for a number of reasons. The array of chemicals included in these products ( Table 1 ) includes many obscure ones, the combinations do not appear to have clear underlying rationales, and the safety of the individual ingredients alone or in combination is unknown. The appeal of the combined remedies is fostered by the use of brand names that emphasize such concepts as “brain health” or “brain power” or suggest antiaging effects.
People who complain of memory deficits benefit from an assessment that includes a thorough history and elements of a medical evaluation (e.g., memory tests, labs, physical exam, and imaging). The fact that the preponderance of stores do not inquire about any aspect of symptoms or signs, or about intentions to see a doctor or get tested, suggests that many cases of significant pathology could be overlooked and/or allowed to progress significantly before medical evaluation and treatment are pursued. At the very least, herbals should not be recommended for memory complaints until the medical possibilities and options are made clear to the individual.
This study shows that warnings about potential side effects do not occur, perhaps because they are obfuscated or denied. As noted, gingko may produce hemorrhagic strokes. Known adverse effects of herbal medications also include hepatitis, gastrointestinal distress, hypertension, hypoglycemia, headache, serotonin syndrome, and dementia. 15 This is compounded by the fact that there is no requirement to gather data on side effects of these agents. There is also little information on potentially harmful drug interactions. Given the number of obscure herbs in the combination treatments, the need for vigilance is great.
One additional focus of the study was the cost of the herbal preparations that were recommended. It should be noted that the cost of many of these is equivalent to or greater than the price of FDA-approved drugs that are marketed for the treatment of memory disorders.
There are certain limitations of this study. The geographic restriction limits the generalizability of the findings. However, an effort was made to include stores that are representative of the national norm and to also broaden the cultural perspective by including Chinatown apothecaries. The sample size may be too small to draw some conclusions. It is also possible that the findings may have been different if the queries were made by elderly individuals rather than the “grandchildren” of the target individual. Nevertheless, the results of this study suggest that herbal remedies are often carelessly recommended without adequate consideration of the nature of the presenting problem and the potential effectiveness or toxicity of the agent(s) advocated. Greater regulation of these practices seems warranted.
1. Cavaliere C, Rea P, Lynch ME, et al: Herbal supplement sales experience slight increase in 2008. HerbalGram 2009; 82:58–61Google Scholar
2. Barnes PM, Bloom B, Nahin R: CDC National Health Statistics Report #12. Complementary and Alternative Medicine Use Among Adults and Children: United States, 2007. Dec 10, 2008. Available at http://nccam.nih.gov/news/2008/nhsr12.pdfGoogle Scholar
3. Robinson A, McGrail MR: Disclosure of CAM use to medical practitioners: a review of qualitative and quantitative studies. Complement Ther Med 2004; 12:90–98Google Scholar
4. DeKosky ST, Fitzpatrick A, Ives DG, et al: The Ginkgo Evaluation of Memory (GEM) study: design and baseline data of a randomized trial of ginkgo biloba extract in prevention of dementia. JAMA 2008; 300:2253–2262Google Scholar
5. Solomon PR, Adams F, Silver A, et al: Ginkgo for memory enhancement: a randomized controlled trial. JAMA 2002; 288:835–840Google Scholar
6. Etienne P, Dastoor D, Gauthier S, et al: Alzheimer disease: lack of effect of lecithin treatment for 3 months. Neurology 1981; 31:1552–1554Google Scholar
7. Brinkman SD, Pomara N, Goodnick PJ, et al: A dose-ranging study of lecithin in the treatment of primary degenerative dementia (Alzheimer disease). J Clin Psychopharmacol 1982; 2:281–285Google Scholar
8. Drachman DA, Glosser G, Fleming P, et al: Memory decline in the aged: treatment with lecithin and physostigmine. Neurology 1982; 32:944–950Google Scholar
9. Dysken MW, Fovall P, Harris CM, et al: Lecithin administration in Alzheimer dementia. Neurology 1982; 32:1203–1204Google Scholar
10. Weintraub S, Mesulan MM, Auty R, et al: Lecithin in the treatment of Alzheimer’s disease. Arch Neurol 1983; 40:527–528Google Scholar
11. Heyman A, Schmechel D, Wilkinson W, et al: Failure of long-term high-dose lecithin to retard progression of early-onset Alzheimer’s disease. J Neural Transm Suppl 1987; 24:279–286Google Scholar
12. Schreiber S, Kampf-Sherf O, Gorfine M, et al: An open trial of plant-source derived phosphatydilserine for treatment of age-related cognitive decline. J Psychiatry Relat Sci 2000; 37:302–307Google Scholar
13. Engel RR, Satzger W, Günther W, et al: Double-blind cross-over study of phosphatidylserine vs placebo in patients with early dementia of the Alzheimer type. Eur Neuropsychopharmacol 1992; 2:149–155Google Scholar
14. Delwaide PJ, Gyselynck-Mambourg AM, Hurlet A, et al: Double-blind randomized controlled study of phosphatidylserine in senile demented patients. Acta Neurol Scand 1986; 73:136–140Google Scholar
15. World Health Organization: WHO Monographs on Selected Medicinal Plants, Volume 1 and Volume 2. Geneva, Switzerland, World Health Organization, 1999Google Scholar



