The Use of DSM-IV and ICD-10 Criteria and Diagnostic Scales for Delirium Among Cardiac Surgery Patients: Results From the IPDACS Study
In clinical trials a diagnosis of delirium is made on the basis of DSM-IV, 8 DSM-III-R, 9 and ICD-10 10 or different psychometric scales such as the Confusion Assessment Method, the Memorial Delirium Assessment Scale (MDAS), or the Delirium Index. 11 – 14
Although delirium prevalence varies in number depending on the diagnostic tools and criteria administered, the sensitivity and specificity of DSM-IV and ICD-10 criteria for delirium were previously evaluated in only 1 study of a population of elderly hospitalized patients. 15 In another study, Laurila et al. 16 , 17 assessed the impact of different diagnostic criteria on the prevalence rates and prognosis of delirium diagnosed among elderly inpatients and nursing home residents.
However, diagnostic accuracy of different diagnostic systems in estimating the incidence of delirium among surgery patients has not been investigated to date.
The MDAS—one of the diagnostic instruments used in the present study—is a clinician-rated scale reflecting the diagnostic criteria for delirium in DSM-IV as well as DSM-III-R and ICD-9. 12 Although the MDAS was initially designed to measure the severity of delirium, the validation study by Breitbart et al. 12 in a group of 33 mixed cancer and AIDS patients established a diagnostic cutoff score to be 13. Nonetheless, the accuracy of the MDAS in evaluating the incidence of delirium among patients after cardiac surgery was not previously assessed.
The Delirium Index was adopted from the Confusion Assessment Method and intended as a measure of the severity of delirium for use in delirium research. 13 However, the optimal diagnostic cutoff value of this measure was not investigated in any previous studies.
Therefore, we would like to present the analysis of data collected in the Incidence and Predictors of Delirium After Cardiac Surgery Study (IPDACS Study). One of the objectives of this research was to establish the frequency of delirium diagnosed on the basis of DSM-IV and ICD-10 criteria. Moreover, the optimal cutoff scores of the MDAS and Delirium Index in estimating the incidence of delirium after cardiac surgery have been investigated. Furthermore, present results have been compared to the findings of our preliminary study conducted in a less considerable group of participants (n=260). 18 – 20
METHODS
Patient Population
After the Ethics Committee of the Medical University of Lodz approval had been obtained, 846 patients consecutively admitted to the Department of Cardiac Surgery in Lodz for a heart operation with cardiopulmonary bypass between November 2004 and April 2007 were asked to join the study. We excluded from the study 283 patients for the following reasons: 152 individuals declined to participate, 55 underwent urgent surgery, 53 were in poor general condition that precluded the participation (e.g., severe circulatory failure, cardiogenic shock), 12 died during the first 6 days after surgery (period of postoperative assessment), 10 had preoperatively diagnosed dementia, and one was illiterate. Individuals with dementia were excluded from the study since one of the study objectives (not presented in the current analysis) was to determine whether cognitive impairment other than dementia independently predisposes to postoperative delirium. The other 563 subjects gave their informed consent and were enrolled and completed the study.
Preoperative Assessment
The studied population was examined the day prior to the scheduled operation with the use of the Mini-Mental State Examination (MMSE) to screen for possible cognitive impairment (MMSE score ≤24) by two psychiatrists (JK, MK). 21 For individuals with dementia diagnosed or suspected on the basis of data from the patients’ history, the MMSE assessment and a regular psychiatric examination were excluded from the study (n=10). None of the participants had preoperative delirium while being assessed according to DSM-IV criteria.
Postoperative Assessment
Following surgical intervention, DSM-IV and ICD-10 criteria, as well as the MDAS (cutoff point ≥13), were used to diagnose delirium. All the patients were also evaluated with the use of the Delirium Index. The assessment of each individual was done once a day postoperatively with the use of all above diagnostic criteria and tools, within 2 to 6 days after surgery, by one of the two psychiatrists involved in the study. Each instrument was administered independently of another during the single evaluation. First, the assessment with the use of the scales was performed without counting the total score achieved by the patients. Next, the diagnostic criteria were used to establish delirium diagnosis. Participants were also screened for delirium twice a day, within 2–6 days after surgery, with the use of the MDAS by one of the three physicians (MB, PO, AB) involved in their daily care. Individuals who scored 8 or more points on the MDAS were additionally interviewed by a psychiatrist.
The psychiatrists and other physicians were equally trained by the senior author (TS) in applying the scales and criteria used in this research. The interobserver reliability of investigators, calculated in the random sample of 40 paired assessments, was κ=1.0 for DSM-IV criteria, 0.98 for ICD-10 criteria, and 0.96 for the MDAS.
Measures
The MDAS is a 10-item, four-point clinician-rated scale (possible range: 0–30) initially designed to measure the severity of delirium in medically ill patients. 12 However, a validation study by Breitbart et al. 12 in a group of 33 mixed cancer and AIDS patients established a diagnostic cutoff score of this measure to be 13. The MDAS reflects the diagnostic criteria for delirium in DSM-IV, as well as symptoms of delirium from earlier classification systems (DSM-III, DSM-III-R, ICD-9). Unlike existing measures of delirium, the MDAS can be administered repeatedly within the same day and monitors changes in delirium severity.
The Delirium Index is a seven-item, four-point clinician-rated scale (possible range: 0–21) intended as a measure of the severity of delirium for use in delirium research. 13 The Delirium Index was adopted from the Confusion Assessment Method and is based on the observation of the patient without additional information from the family members, nursing staff, or the patient’s medical chart.
Statistical Analysis
Central tendency and dispersion measures of variables and their subsets were assessed using descriptive statistics depending on distribution. Continuous variables are shown as means, standard deviations (SD) and ranges or medians and interquartile ranges (IQR). In order to establish the agreement in classification of patients according to DSM-IV and ICD-10 criteria, an “interscale” analysis was performed. A McNemar’s test was used to contrast the number of patients with delirium diagnosis according to different measures. A receiver operating characteristic (ROC) curve was plotted to show the sensitivity and specificity for various scores of the MDAS and Delirium Index in comparison with DSM-IV criteria of delirium. Statistical analysis was performed using the STATISTICA package (StatSoft, Tulsa, Oklahoma).
RESULTS
Of the 563 patients, 395 (70%) were men. Their mean age was 62 years old (range=25–81 [SD=9.0]). Significant differences of mean age were observed between delirious and nondelirious patients (mean=68.5 [SD=7.6] compared with mean=61.0 [SD=8.9] years, respectively; p<0.001).
For all participants, the incidence of delirium diagnosed in accordance with DSM-IV, ICD-10 criteria, and the MDAS was 16.3% (95% confidence interval [CI]=13.5%–19.6%), 14.2% (95% CI=11.4%–17.2%), and 11.7% (95% CI=9.5%–14.8%), respectively.
The onset of delirium was most frequently diagnosed on the fourth postoperative day (IQR=3–5), both with the use of DSM-IV and ICD-10 criteria and with the MDAS. The mean score of the MDAS was 15 points (IQR=12–20) for individuals with delirium established on the basis of DSM-IV criteria and 5 points (IQR=3–7) for patients without delirium (p<0.001). The mean score of the Delirium Index was 12 points (IQR=8–15) for individuals with delirium and 3 points (IQR=2–5) for patients without delirium (p<0.001).
The “interscale” agreement kappa statistic between DSM-IV and ICD-10 criteria equaled 0.91 (95% CI=0.86–0.96), with a standard error (SE) of 0.025, which is regarded as a very good agreement between the two. However, chi-square McNemar testing showed that ICD-10 criteria produced a greater number of delirium diagnoses than MDAS (χ 2 =4.65, df=1, p=0.03), whereas DSM-IV criteria yielded more diagnoses of delirium than ICD-10 (χ 2 =11.08, df=1, p=0.0009) and the MDAS (χ 2 =23.0, df=1, p<0.0001).
The exact number of patients classified according to both classification systems is shown in Table 1 . The symptoms observed among patients with DSM-IV-diagnosed delirium who did not meet ICD-10 criteria (n=13) are listed in Table 2 .
 |
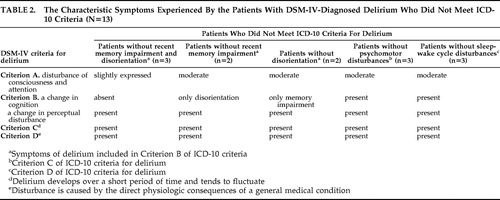 |
The specificity and sensitivity for various values of the MDAS and Delirium Index in comparison with DSM-IV delirium criteria are presented in Figure 1 and Figure 2 . Areas under the curves were 0.997 (95% CI=0.987–0.999 [SE=0.004]) for the MDAS and 0.985 (95% CI=0.972–0.994 [SE=0.009]) for the Delirium Index. The cutoff values were established at a level of 10 or more points on the MDAS and 7 or more on the Delirium Index.
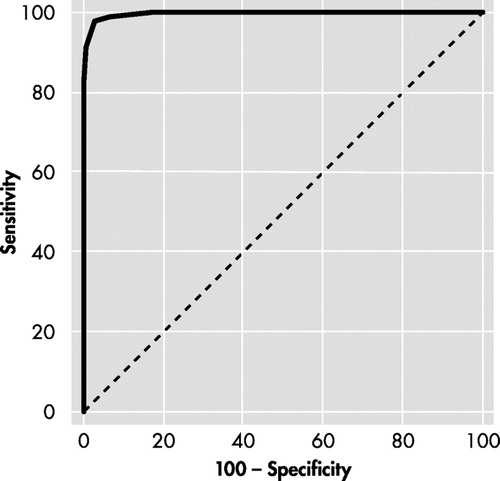
Cutoff value was established at >9 points with sensitivity of 97.8% and specificity of 97.0%.
MDAS=Memorial Delirium Assessment Scale; ROC=receiver operating characteristic
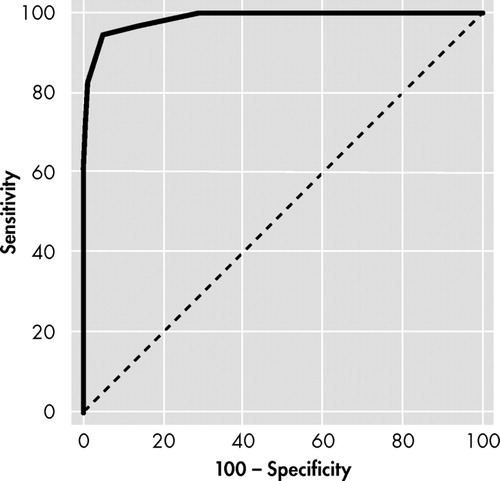
Cutoff value was established at >6 points with sensitivity of 94.6% and specificity of 94.9%.
ROC=receiver operating characteristic
DISCUSSION
According to the results of the present study, there are differences in the incidence of postoperative delirium depending on the measures used by the researcher. Although the “interscale” correlation of 0.91 suggested good agreement between DSM-IV and ICD-10 diagnostic systems, DSM-IV criteria for delirium were found to be more inclusive than those of ICD-10. Moreover, a diagnostic score of 10 on the MDAS and 7 on the Delirium Index were established to be optimal in diagnosing delirium among cardiac surgery patients, which is consistent with our preliminary findings. 20
The differences in delirium estimates revealed in the current study were due to more restrictive criteria used in ICD-10. Namely, ICD-10 criteria require all symptoms of delirium to be present in each of the five areas (disturbance of consciousness and attention, cognition, psychomotor, emotional, and sleep-wake cycle disturbances). DSM-IV criteria are less restrictive; thus, subjects who did not meet ICD-10 criteria for delirium could fulfill criteria included in DSM-IV ( Table 2 ).
Cole et al. 15 and Laurila et al. 17 also showed a discrepancy in the incidence of delirium depending on the kind of criteria used (ICD-10, DSM-III, DSM-III-R, DSM-IV). 15 , 17 The study by Cole et al. 15 revealed that for elderly patients with or without dementia, DSM-IV criteria for delirium were the most inclusive followed by DSM-III and ICD-10, respectively. The other study among geriatric hospital patients and nursing home residents confirmed this observation. 17
It is interesting, however, that in the present research the differences in delirium incidence were not only due to patients without psychomotor or sleep-wake cycle disturbances who were diagnosed as delirious according to DSM-IV criteria ( Table 2 ). There was also another group of participants with only partly expressed change in cognition who were diagnosed as delirious according to DSM-IV but not ICD-10 criteria. This new finding is a consequence of the different design of Criterion B in DSM-IV and ICD-10 criteria. According to the DSM-IV classification system, one of the two diagnostic features (change in cognition or perceptual disturbances) is sufficient to fulfill Criterion B for delirium. However, in ICD-10 criteria, change in cognition is always required for delirium diagnosis.
The Confusion Assessment Method is a diagnostic scale that has been most frequently used in delirium research to date. 11 However, this instrument consists of diagnostic criteria from DSM-III-R. As it is known from available studies, problems have emerged with DSM-III-R since some criteria were found to be difficult to interpret. 22 Thus, one of the aims of the present study was to evaluate a diagnostic cutoff value of the MDAS—a measure which reflects both DSM-IV and DSM-III-R criteria for delirium.
In our present study the MDAS diagnostic cutoff score of 10 produced optimal results in relation to the presence or absence of delirium (with sensitivity of 97.8% and specificity of 97.0% in comparison to DSM-IV criteria). Breitbart et al. 12 revealed the optimal diagnostic cutoff value to be 13 with high sensitivity (93.7%), though markedly lower specificity (70.6%). In their study, the MDAS with such a diagnostic cutoff value appropriately classified patients with moderate and severe delirium; however, a diagnosis of mild delirium was inaccurate. On the other hand, Lawlor et al. 23 suggested an optimum MDAS diagnostic score of 7 in the comparable population of AIDS and cancer patients, whereas in the other MDAS validation study in a population of hospitalized patients, the cutoff score of 10 was established to be optimal. 23 , 24
In our study, the individuals with delirium symptoms noticed during a psychiatric interview whose score in the MDAS was slightly below 13 had a full-blown, though usually less severely symptomatic, delirium. The explanation for this, apart from the low specificity of the cutoff value, may be the specific character of the intensive care unit, the cardiac surgery department, and the surgical procedures themselves which create several limitations, previously noticed by Liptzin et al. 22 The individuals were examined during the first 6 days after a painful and physically exhausting surgical procedure; hence, their psychomotor activity was problematic to rate. Additionally, disorganized thinking and insomnia were difficult to judge as the patients spoke very little, were intubated, and were given hypnotic drugs to help them sleep or their sleep could have been disrupted by other patients, trouble breathing, or nursing interventions. An inappropriate assessment of the severity of those symptoms could lower the total MDAS score and result in a misdiagnosis of mild delirium.
This is also the first study investigating the cutoff values of the Delirium Index in establishing the diagnosis of delirium. In available studies the above scale has been used only as a measure of the severity of delirium. However, the Delirium Index with diagnostic scores evaluated in this series may be used in future studies and clinical practice as a tool for simple and quick assessment of delirium incidence and severity.
The strength of the present study is its prospective design, the employment of qualified physicians, consistent methodology, and the considerable total number of participants and the number of patients with a diagnosis of delirium who were enrolled.
A potential limitation of this study is the use of the simple MMSE questionnaire to assess cognitive function. However, it would not be feasible to use a wider test battery because the patients were often unstable, anxious, or immobilized; therefore, a prolonged interview was not advisable.
The other potential drawback of this research is, as mentioned above, the psychiatric assessment of individuals whose medical condition could mimic or mask delirium. Therefore, some manifestations could be falsely classified or unrecognized as symptoms of delirium. Nevertheless, we believe that the involvement of qualified and experienced physicians reduced the risk of potential misdiagnoses.
CONCLUSION
The present study revealed DSM-IV criteria as more inclusive, while ICD-10 criteria are more restrictive, in establishing a diagnosis of delirium after cardiac surgery. Thus, the use of DSM-IV criteria in clinical practice can result in a lower prevalence of false negative results but could also lead to diagnosing as delirious patients with vague and unspecified symptoms.
The two diagnostic features of DSM-IV criteria are responsible for their more inclusive character. First, DSM-IV includes subjects who do not show psychomotor and sleep-wake cycle disturbances. Second, the patients without change in cognition are classified as delirious if perceptual disturbances are present. Furthermore, the cutoff scores of 10 on the MDAS and 7 on the Delirium Index are suggested to be optimal in diagnosing delirium in the population of cardiac surgery patients.
1. Detroyer E, Dobbels F, Verfaillie E, et al: Is preoperative anxiety and depression associated with onset of delirium after cardiac surgery in older patients? A prospective cohort study. J Am Geriatr Soc 2008; 56:2278–2284Google Scholar
2. Bucerius J, Gummert JF, Borger MA, et al: Predictors of delirium after cardiac surgery delirium: effect of beating-heart (off-pump) surgery. J Thorac Cardiovasc Surg 2004; 127:57–64Google Scholar
3. Marcantonio ER, Kiely DK, Simon SE, et al: Outcomes of older people admitted to postacute facilities with delirium. J Am Geriatr Soc 2005; 53:963–969Google Scholar
4. van der Mast RC, Roest FH: Delirium after cardiac surgery: a critical review. J Psychosom Res 1996; 41:13–30Google Scholar
5. Norkiene I, Ringaitiene D, Misiuriene I, et al: Incidence and precipitating factors of delirium after coronary artery bypass grafting. Scand Cardiovasc J 2007; 41:180–185Google Scholar
6. Rudolph JL, Jones RN, Grande LJ, et al: Impaired executive function is associated with delirium after coronary artery bypass graft surgery. J Am Geriatr Soc 2006; 54:937–941Google Scholar
7. Tan MC, Felde A, Kuskowski M: Incidence and predictors of postcardiotomy delirium. Am J Geriatr Psychiatry 2008; 16:575–583Google Scholar
8. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1997Google Scholar
9. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, revised. Washington, DC, American Psychiatric Association, 1980Google Scholar
10. WHO: International Statistical Classification of Diseases and Health Related Problems—Tenth Revision. Geneva, World Health Organization, 1993Google Scholar
11. Inouye SK, van Dyck CH, Allesi CA, et al: Clarifying confusion: the Confusion Assessment Method: a new method for detection of delirium. Ann Inter Med 1990; 113:941–948Google Scholar
12. Breitbart W, Rosenfeld B, Roth A, et al: The Memorial Delirium Assessment Scale. J Pain Symptom Manage 1997; 13:128–137Google Scholar
13. McCusker J, Cole MG, Dendukuri N, et al: The Delirium Index, a measure of the severity of delirium: new findings on reliability, validity, and responsiveness. J Am Geriatr Soc 2004; 52:1744–1749Google Scholar
14. Kamierski J, Sobów T, Kłoszewska I: Delirium after cardiac surgery. Kardiol Pol 2007; 65:583–587 (Polish)Google Scholar
15. Cole MG, Dendukuri N, McCusker J, et al: An empirical study of different diagnostic criteria for delirium among elderly medical inpatients. J Neuropsychiatry Clin Neurosci 2003; 15:200–207Google Scholar
16. Laurila JV, Pitkala KH, Strandberg TE, et al: Impact of different diagnostic criteria on prognosis of delirium: a prospective study. Dement Geriatr Cogn Disord 2004; 18:240–244Google Scholar
17. Laurila JV, Pitkala KH, Strandberg TE, et al: The impact of different diagnostic criteria on prevalence rates for delirium. Dement Geriatr Cogn Disord 2003; 16:156–162Google Scholar
18. Kazmierski J, Kowman M, Banach M, et al: Preoperative predictors of delirium after cardiac surgery: a preliminary study. Gen Hosp Psychiatry 2006; 28:536–538Google Scholar
19. Banach M, Kazmierski J, Kowman M, et al: Atrial fibrillation as a nonpsychiatric predictor of delirium after cardiac surgery: a pilot study. Med Sci Monit 2008; 14:CR286–291Google Scholar
20. Kazmierski J, Kowman M, Banach M, et al: Clinical utility and use of DSM-IV and ICD-10 criteria, and the Memorial Delirium Assessment Scale in establishing diagnosis of delirium after cardiac surgery. Psychosomatics 2008; 49:73–76Google Scholar
21. Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for clinician. J Psychiatr Res 1975; 12:189–198Google Scholar
22. Liptzin B, Levkoff SE, Cleary PD, et al: An empirical study of diagnostic criteria for delirium. Am J Psychiatry 1991; 148:454–457Google Scholar
23. Lawlor PG, Nekolaichuk C, Gargnon B, et al: Clinical utility, factor analysis, and further validation study of the Memorial Delirium Assessment Scale in patients with advanced cancer: assessing delirium in advanced cancer. Cancer 2000; 88:2859–2867Google Scholar
24. Shyamsundar G, Raghuthaman G, Rajkumar AP, et al: Validation of Memorial Delirium Assessment Scale. J Crit Care 2009; 24:530–534Google Scholar



