Discriminant Validity of the Wender Utah Rating Scale for Attention-Deficit/Hyperactivity Disorder in Adults
Abstract
The authors examined the factor structure and discriminant validity of the Wender Utah Rating Scale (WURS) in adults seeking evaluation for attention-deficit/hyperactivity disorder (ADHD). Three factors (Dysthymia, Oppositional/Defiant Behavior, and School Problems) accounted for 59.4% of the variance. In a stepwise discriminant function analysis, age and childhood school problems emerged as significant variables. The classification procedure correctly classified 64.5% of patients. Among those who did not have ADHD, only 57.5% were correctly classified compared with 72.1% among those with ADHD. The WURS is sensitive in detecting ADHD, but it misclassifies approximately half of those who do not have ADHD.
Attention-deficit/hyperactivity disorder (ADHD) affects approximately 8% of children.1 Follow-up studies of children with some form of ADHD suggest that from 30% to 60% will continue to exhibit impairment associated with ADHD symptoms into adulthood.2 Thus it is estimated that approximately 4% of the adult population exhibits ADHD,3 consistent with recent field surveys in the adult population.1
The diagnosis of ADHD in adults is challenging because symptoms of inattentiveness and/or hyperactivity and impulsivity must have been present and causing impairment before they were 7 years old.4 Although recent studies have suggested this age cutoff may be too stringent,5 childhood, prepubertal onset is probably still required for the diagnosis to be valid. Retrospective recall bias and elapsed time necessarily limit the accuracy of information on behavior prior to age 7.
This makes diagnosis in adults, who often were not evaluated or identified as having ADHD in childhood, quite difficult—a difficulty that is compounded by the lack of experience in childhood psychopathology of most adult clinicians who usually evaluate such patients. In this setting, the availability of rating scales to characterize and quantify relevant ADHD behaviors and symptoms is an important diagnostic aid.
Despite the explosion of interest, popular press publications, and scientific investigation in adult ADHD, little has been published on rating scales that might screen for or assist in diagnosing this condition in adults. The best-known scale for assessing adults with ADHD is still the Wender Utah Rating Scale, which retrospectively assesses ADHD-relevant childhood behaviors and symptoms in adults.6,7 This scale originally consisted of 61 items reflecting signs and symptoms of ADHD and was subsequently reduced to the 25 items that distinguished patients with ADHD from a nonpatient comparison group.6 The 25-item Wender Utah Rating Scale has been shown to distinguish ADHD patients from patients with unipolar depression; to differentiate responders from nonresponders to methylphenidate in a controlled treatment study;6,8 and to be moderately correlated with a rating scale completed by parents.6
Although two subsequent studies9,10 have replicated the adequate internal consistency of the scale, established good temporal stability with one-month test-retest reliability, and explored the scale's factor structure with respect to gender,9 no published study has reexamined the scale's discriminant validity with respect to other psychiatric populations. Furthermore, in the original study Ward and colleagues preselected their comparison populations, so that the discriminant validity of the scale in a sample of adults presenting for ADHD evaluation is unknown.6 Such a sample is likely to have a more heterogeneous group of psychiatric diagnoses than the homogenous comparison sample of unipolar depressed patients used by Ward et al.6
Use of this scale as a measure of current, as well as childhood, behavior has been shown to distinguish ADHD and non-ADHD patients in a preliminary analysis11 and to change with medication treatment in an outpatient ADHD sample.12 However, the internal consistency and factor structure of the scale when used in this manner are unknown.
Here we report on the factor structure, internal consistency, and discriminant validity of the 25-item Wender Utah Rating Scale, used both in its traditional retrospective way, to characterize childhood behavior and symptoms (WURS-C), and to rate adult behavior and symptoms in 141 adults seeking evaluation for ADHD in a specialty clinic (WURS-A). Unlike the previous report,11 which divided this group three ways to include an intermediate group (patients with ADHD symptoms who either lacked a childhood history of ADHD or had current psychiatric comorbidity that complicated interpretation of current symptoms), we have dichotomized the sample so that those with absent childhood histories are classified as not having ADHD and those with complicating comorbidity but clear-cut childhood histories are classified as having ADHD.
METHODS
Participants
One-hundred forty-three adults referred to an adult ADHD specialty clinic were administered the 25-item version of the WURS-C and WURS-A as part of a comprehensive intake assessment battery. Detailed methods of the assessment are reported elsewhere.11 Of the 143 adults evaluated in the adult ADHD specialty clinic, 46 were originally classified as definitely having ADHD; 51 showed symptoms consistent with ADHD, but complicating comorbidity or absence of childhood history made a definite DSM-IV diagnosis problematic; and 48 clearly did not have ADHD. Two patients were excluded from the present analyses because of missing data on the WURS-C and WURS-A.
Measures
Non-ADHD psychiatric diagnoses were assessed in both clinics by use of a semistructured diagnostic interview previously validated against the Structured Clinical Interview for DSM-III-R.13–15 Patients evaluated in the clinic were also evaluated for ADHD, using DSM-IV criteria and a structured interview provided by J. Biederman, M.D.
The 25-item Wender Utah Rating Scale6 was used to measure the presence of attention deficit disorder symptoms in childhood and adulthood. Patients were instructed to rate 25 items that completed the sentence stems “As a child I was or had…” and “In the last week I have been or had…”. Sample items include “not achieving up to potential” and “concentration problems, easily distracted.” Ratings were made on a 5-point scale ranging from 0 (“not at all or very slightly”) to 4 (“very much”). The range of possible scores is from 0 to 100. Items comprising the original 61-item version of the WURS7 and the 25-item version are shown in Table 1.
Written evaluations of the 51 patients originally classified as “probable” ADHD cases were reviewed by a board-certified psychiatrist (P.R.B.) and a senior psychologist (B.S.M.), both of whom have extensive experience in making the diagnosis of ADHD in adults. The following criteria were used in the reclassification: 1) complicating comorbidity in adulthood did not rule out a diagnosis of ADHD; 2) the maximum age at onset was raised to 13 years;16 and 3) evidence of functional impairment was required unless there was clear evidence that a spouse or business surrogate was compensating for the patient's deficits.
Statistical Analyses
We analyzed demographic differences between groups, using chi-square tests for categorical variables and t-tests for continuous variables.
A principal components analysis using varimax rotation was performed on the 25 test items. The number of factors retained was determined by examination of the scree plot and use of the Kaiser-Guttman rule (i.e., eigenvalues greater than 1.0). Cronbach's alpha was calculated as a measure of internal consistency on all 25 items and on the subscales resulting from the factor analysis.
Discriminant validity was determined by a stepwise discriminant function analysis in which the subscale scores resulting from the factor analyses of the WURS-C and WURS-A were entered into the function. The resulting function was applied to each case, using a jackknifed classification.
RESULTS
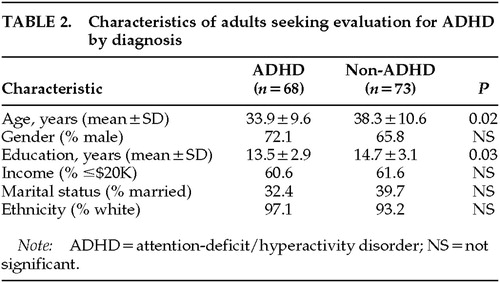
Table 2 presents characteristics of patients presenting for evaluation as a function of ADHD status. Patients diagnosed with ADHD were younger than patients who did not have this diagnosis, and they completed fewer years of education. These variables were included in the discriminant function analysis.
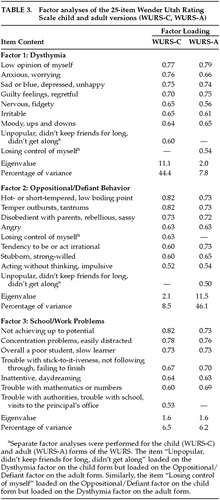
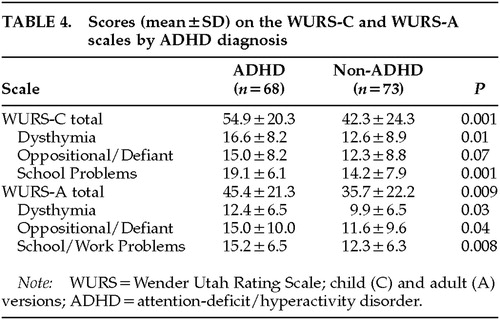
For the WURS-C, the principal components factor analysis resulted in a three-factor solution that accounted for 59.4% of the variance (Table 3). The three factors were labeled Dysthymia, Oppositional/Defiant Behavior, and School Problems. Two items did not load at the specified 0.50 cutoff level on the WURS-C: “tendency to be immature,” and “trouble seeing things from someone else's point of view.” Alpha coefficients were WURS-C Total=0.95, Dysthymia=0.91, Oppositional/Defiant Behavior=0.90, and School Problems=0.87. For the WURS-A, the principal components factor analysis also resulted in a three-factor solution, which accounted for 60.1% of the variance (Table 3). Similar factors emerged, with adequate alpha reliabilities: Oppositional/Defiant Behavior (α=0.90), Dysthymia (α=0.89), and School/Work Problems (α=0.88). The alpha coefficient for the WURS-A total scale was 0.95. Patients diagnosed with ADHD attained higher scores than non-ADHD patients on WURS-A and WURS-C total scales and all subscales, except the Oppositional/Defiant Behavior subscale on the WURS-C (Table 4).
In the discriminant function analysis, age, education, and all three factors from both the WURS-C and WURS-L were entered in stepwise fashion. Two variables entered into the analysis: School Problems from the WURS-C, and age (χ2=19.2, P<0.001). The classification procedure correctly classified 64.5% of patients. Among those who did not have a diagnosis of ADHD, the correct classification rate was low, with only 57.5% correctly classified. Among those receiving a diagnosis of ADHD, the classification rate was better, with 72.1% correctly classified.
DISCUSSION
This study used a clinically referred sample of adults seeking evaluation for ADHD to study the underlying factor structure of the Wender Utah Rating Scale and to determine characteristics of the scale that distinguish those who receive a clinical diagnosis of ADHD from those who do not have ADHD. Results of this study suggest that three factors characterize the Wender Utah Rating Scale: Dysthymia, Oppositional/Defiant Behavior, and School (Work) Problems. These three factors are found in both the retrospective childhood and the adult forms of the instrument. Only one factor, School Problems in childhood, distinguished ADHD from non-ADHD patients. This factor correctly identifies 72% of patients with a clinical diagnosis of ADHD but does little better than chance in correctly identifying adults who do not have ADHD. Thus, the School Problems factor from the WURS-C has reasonable sensitivity, but poor specificity.
These findings provide only limited support for the use of the 25-item WURS as a diagnostic aid in adults who present for ADHD evaluation. In addition to its poor specificity, the underlying factor structure suggests that the WURS measures depression and conduct problems, which are not specific to the DSM-IV ADHD classification. Other studies of symptom clusters in children support two factors: inattention and hyperactivity-impulsivity.17–19
Another possible reason for the low specificity of the WURS may be a response bias on the part of patients evaluated in an ADHD specialty clinic; this is more probable in adult patients, who are unlikely to have parents available as informants regarding childhood behavior.11 To the extent that patients seeking evaluation specifically for ADHD may have a preconceived notion that this diagnosis applies to them, they may be inclined to endorse items that they feel would support such a diagnosis. This tendency may represent yet another limitation of a self-report measure when used to assess for symptoms (both retrospective and current) of ADHD.
The factor structure obtained in the current study differs somewhat from the factor structure previously identified in parents of children referred for evaluation of ADHD.9 The previous factor analysis used all of the 61 original Wender Utah Rating Scale items and analyzed the data separately for males and females. The resulting factor structures were similar, and in both genders they included conduct problems, attention problems, learning problems, poor social skills/unpopularity, and poor stress tolerance/dysphoria. Our use of the 25 items identified previously as distinguishing patients with ADHD from nonpatients6 appeared to collapse these categories by combining learning and attentional problems (School Problems) and combining poor stress tolerance, dysthymia, and poor social skills/acceptability (Dysthymia).
Our findings are important for several reasons. First, the use of the WURS-C as a diagnostic screen in adult psychiatric patients presenting for ADHD evaluation could be misleading. For example, in a patient with equivocal evidence of ADHD by diagnostic interview, a high WURS-C score might sway a clinician in favor of the ADHD diagnosis and a low score might do the opposite. Second, the finding that inattentive symptoms are the best discriminator in adults is consistent with the evolution of ADHD over the lifespan from mixed to more predominantly inattentive. This finding also highlights that the cognitive symptom domain is perhaps the most important to consider when evaluating a general psychiatric population for presence of ADHD.
 |
 |
 |
 |
1 Barkley RA: Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment, 2nd edition. New York, Guilford, 1998Google Scholar
2 Weiss G, Hechtman L: Hyperactive Children Grown Up: ADHD in Children, Adolescents, and Adults, 2nd edition. New York, Guilford, 1993Google Scholar
3 Spencer T, Biederman J, Wilens T, et al: Is attention-deficit hyperactivity disorder in adults a valid disorder? Harv Rev Psychiatry 1994; 1:326–335Google Scholar
4 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Washington, DC, American Psychiatric Association, 1994Google Scholar
5 Barkley RA, Biederman J: Toward a broader definition of the age-of-onset criterion for attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1997; 36:1204–1210Google Scholar
6 Ward MF, Wender PH, Reimherr FW: The Wender Utah Rating Scale: an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry 1993; 150:885–890Crossref, Medline, Google Scholar
7 Wender PH: Wender AQCC (Adult Questionnaire–Childhood Characteristics) scale. Psychopharmacol Bull 1985; 21:927–928Google Scholar
8 Wender PH, Wood DR, Reimherr FW, et al: A controlled study of methylphenidate in the treatment of attention deficit disorder, residual type, in adults. Am J Psychiatry 1985; 142:547–552Crossref, Medline, Google Scholar
9 Stein MA, Sandoval R, Szumoski E, et al: Psychometric characteristics of the Wender Utah Rating Scale (WURS): reliability and factor structure for men and women. Psychopharmacol Bull 1995; 31:425–433Medline, Google Scholar
10 Rossini ED, O'Connor MA: Retrospective self-reported symptoms of attention-deficit hyperactivity disorder: reliability of the Wender Utah Rating Scale. Psychol Rep 1995; 77:751–754Crossref, Medline, Google Scholar
11 Roy-Byrne P, Scheele L, Brinkley J, et al: Adult attention-deficit hyperactivity disorder: assessment guidelines based on clinical presentation to a specialty clinic. Compr Psychiatry 1997; 38:1–9Crossref, Google Scholar
12 Adler LA, Resnick S, Kunz M, et al: Open-label trial of venlafaxine in adults with attention deficit disorder. Psychopharmacol Bull 1995; 31:785–788Medline, Google Scholar
13 Dunner DL, Tay LK: Diagnostic reliability of the history of hypomania in bipolar II patients and patients with major depression. Compr Psychiatry 1993; 34:303–307Crossref, Medline, Google Scholar
14 Flick SN, Roy-Byrne P, Cowley D, et al: DSM-III-R personality disorders in a mood and anxiety disorders clinic: prevalence, comorbidity, and clinical correlates. J Affect Disord 1993; 27:71–79Crossref, Medline, Google Scholar
15 Spitzer RL, Williams JB, Gibbon M, et al: Structured Clinical Interview for DSM-III-R–Non-Patient Edition (SCID-NP) Version 1.0. Washington, DC, American Psychiatric Press, 1990Google Scholar
16 Applegate B, Lahey BB, Hart EL, et al: Validity of the age-of-onset criterion for ADHD: a report from the DSM-IV field trials. J Am Acad Child Adolesc Psychiatry 1997; 36:1211–1221Google Scholar
17 Bauermeister JJ, Alegria M, Bird HR, et al: Are attentional-hyperactivity deficits unidimensional or multidimensional syndromes? Empirical findings from a community survey. J Am Acad Child Adolesc Psychiatry 1992; 31:423–431Crossref, Medline, Google Scholar
18 Halperin JM, Matier K, Bedi G, et al: Specificity of inattention, impulsivity, and hyperactivity to the diagnosis of attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1992; 31:190–196Crossref, Medline, Google Scholar
19 Pelham WE, Gnagy EM, Greenslade KE, et al: Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 1992; 31:210–218Crossref, Medline, Google Scholar