Imaging Auditory Verbal Hallucinations During Their Occurrence
SIR: We report the case of a 26-year-old Caucasian right-handed male who came to our attention because of “hearing conversation.” The patient was born and raised in Iraq. He received a high school level of education and has no significant psychiatric, medical, or family history. At age 19, he was drafted into the army. After 3 years of noncombat service, he defected and escaped to Kuwait, where he was imprisoned and tortured. He was told, during torture, that he would be killed. The patient lost consciousness for an unknown period of time, and upon regaining consciousness he thought that he was dead. He was later sent to a refugee camp in Saudi Arabia, where he spent 3 years before immigrating to the United States.
Approximately 2 months afterward, he gradually started experiencing various symptoms: nightmares, disturbed sleep, fatigue, hypnagogic and hypnopompic auditory hallucinations, and auditory verbal hallucinations in full alertness during the daytime.
The auditory verbal hallucinations consisted of a replay of conversations that took place previously. They occurred spontaneously. The patient did not resist their occurrence and could also induce them by effortful concentration. They were not cued, and their content had no emotional significance and had no relation to torture, imprisonment, or war. He experienced the “voices” inside his head but emphasized their auditory quality, “like somebody talking to me.” These perceptions appeared when he was idle in an environment with a steady level of noise, and they dissipated when the constancy of external auditory stimuli or the patient's passivity was interrupted. They were not concomitant to normal auditory stimuli, and he had full insight into their abnormality. His mental status examination was normal otherwise.
Physical examinations, routine laboratory tests, and routine EEG were within normal limits. The MRI revealed no structural abnormalities but was compatible with arachnoid cysts in the middle cranial fossae.
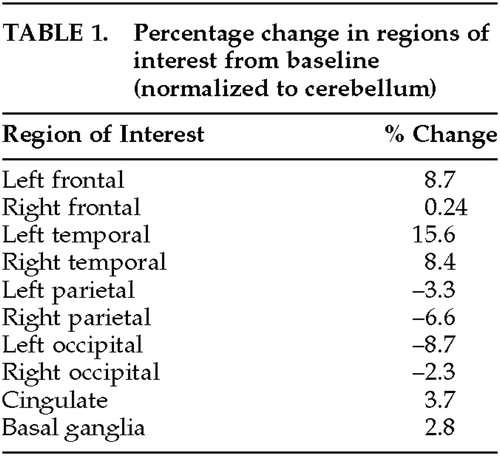
Two SPECT scans were performed using [99mTc]l,l-ethyl cysteinate dimer (ECD) with a 2-month interval between scans. Acquisition conditions were the same in both scans, and the patient's mental state differed only with regard to the presence of hallucination in the first one. ECD uptake coincided with hallucination in this scan.
Visual observation indicated that during the hallucinatory experience, regional cerebral blood flow (rCBF) was maximally increased in the left temporal region and to a lesser extent in the left frontal and right temporal regions. This visual impression was corroborated by region of interest (ROI) data obtained using previously described methods.1 ROI data were normalized to cerebellum and expressed as percentage change from baseline (Table 1). While the patient was experiencing hallucinations, only one region showed an increase in rCBF that was greater than 10% (left temporal, 15.6%).
Comment
Literature review of functional imaging studies shows that they yield inconsistent findings; however, the activation of the brain region encompassing Wernicke's area has been frequently correlated to hallucinations in different illnesses (M. Stephane, N.N. Bourous, submitted for publication). This relationship could indicate that activation of Wernicke's area constitutes the final common pathway for the expression of the hallucinatory process, the latter involving a distributed neural network.2
 |
1 Matthew E, Hill TC: Brain mapping studies with single photon emission CT. Radiology 1998; 206:483–489Crossref, Medline, Google Scholar
2 Andreasen NC, O'Leary DS, Flaum M, et al: Hypofrontality in schizophrenia: distributed dysfunctional circuits in neuroleptic naive patients. Lancet 1997; 349(9067):1730–1734Google Scholar