Clinical Features Characterizing Young-Onset and Intermediate-Onset Schizophrenia
Abstract
Late-onset schizophrenia has been noted to have distinct clinical characteristics. The authors compared symptom characteristics between early- and intermediate-onset patients (N=259) to determine whether clinical features distinguished differences within younger populations. On global measures of psychotic, disorganized, and negative symptoms, early-onset patients had greater disorganized and negative symptoms but did not differ in hallucinations and delusions. The dichotomy of early vs. late onset may extend to a younger population, reflecting a more continuous influence.
The issue of whether the neuropathology in schizophrenia differs among those with onset in childhood, adolescence, adulthood, and late life remains unresolved after a century of debate. Kraepelin's original descriptions of dementia praecox suggested only a small percentage of patients experienced the onset of symptoms after age 40.1 Among the small group that did have a late onset, the clinical features were observed by Kraepelin to be essentially the same as those in typical early-onset dementia praecox.
Kraepelin also recognized a separate “paraphrenic” syndrome, with an affectively intact, primarily delusional, less deteriorative course.1 At the time of its conceptualization, the term paraphrenia did not have specific age boundaries. It was used simply to represent a prognostically different syndrome that may occur regardless of age at onset. Ensuing observations that paraphrenic patients often had a later age at onset led Roth to coin the term late paraphrenia.2 This term was intended to identify patients with onset after the age of 60 who displayed the symptom features earlier ascribed to paraphrenia. The unique characteristics that often distinguished this group included less affective flattening, less formal thought disorder, and the presence of often plausible paranoid delusions in the absence of severe social deterioration.3–5
A somewhat complicating influence has been the designation by Manfred Bleuler in 1943 of late-onset schizophrenia. This term was simply intended to describe patients with onset between age 40 and 60 whose illness had essentially the same clinical features as the typical young-onset illness: the same incidence of social decline, disorganization, negative symptoms, and deteriorative course.6 The result of these efforts to describe the late-life syndromes has been confusion in terms and interpretations. It is of clinical importance to clarify these terms to better inform treatment studies and guide future research, particularly as there may exist unique neurobiologic mechanisms underlying the late-life syndromes. Furthermore, the influence of age-related neurodegenerative processes that may precipitate psychosis in the elder years (e.g., dementia) compounds the difficulty in achieving diagnostic certainty among older patients.
The first step in teasing apart these syndromes is to determine the appropriate age cutoff at which the “late” and “paraphrenic” features are most likely to occur. The age of 45 has been one consensus, as seen in DSM-III-R.7 We examined the issue of whether age at onset significantly affects clinical presentation in the absence of the influence of age-related brain changes. For this analysis, we examined this variable within the midlife range—that is, onset between ages 30 and 40. We postulated that the relationship seen between current late-onset and early-onset patients could also be found to exist among younger subjects. Specifically, it was our hypothesis that, compared with young-onset subjects, intermediate-onset patients (ages 30 to 45 years) will have fewer negative and disorganized symptoms.
METHODS
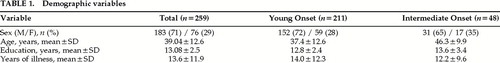
Our sample included 259 subjects, who were recruited for study by the Mental Health Clinical Research Center and gave written informed consent. All subjects had DSM-IV schizophrenia determined by a structured interview, the Comprehensive Assessment of Symptoms and History (CASH).8 Patients were excluded if there was a substantial history of substance abuse, head trauma, or other central nervous system pathology. Subjects within their first episode of psychosis were not included in this analysis. Subjects were assessed by use of the CASH, the Scale for the Assessment of Positive Symptoms (SAPS),9 and the Scale for the Assessment of Negative Symptoms (SANS).10 The measures used in this analysis were derived from the “current” symptom portion of the CASH instrument, reflecting the character of each subject's symptoms over the preceding month interval. The age at onset was defined as the age that the subject first experienced psychotic symptoms of sufficient number and severity to constitute a psychotic “syndrome.” The syndrome was defined as meeting criteria for DSM-IV schizophrenia without the 6-month duration criterion.
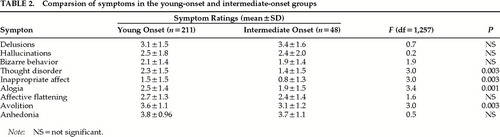
A psychotic symptom score was generated by the sum of the SAPS global ratings of hallucinations and delusions. Similarly, a disorganization score was created from the sum of SAPS global ratings of disorganized speech, positive formal thought disorder, and inappropriate affect; and a negative symptom score represented the sum of SANS global ratings of alogia, avolition, anhedonia, and affective flattening. Additionally, individual ratings for each symptom were examined in the two groups in relation to age-at-onset status.
Initially the subjects were dichotomized into “young” onset and “intermediate” onset groups, with ages at onset of 20–29 and 30–45 years, respectively. Adolescent-onset and childhood-onset subjects were excluded. The proportion of women and men in the young- and intermediate-onset groups did not differ significantly. There was no difference in the two groups in mean age at the time of assessment. A logistic regression analysis determined whether the two groups differed across the three major symptom dimensions (psychotic, negative, and disorganized), and individual t-tests (two-tailed) estimated differences between the groups in terms of individual symptoms. Demographic variables are shown in Table 1.
RESULTS
In the analysis of the three symptom dimensions, disorganized and negative symptoms were found to be significantly more severe among the young-onset patients compared with the intermediate-onset patients (F=12.7, df=1,257, P=0.0004; F=7.7, df=1,257, P=0.0061, respectively). In terms of individual symptoms, the disorganized symptoms of formal thought disorder and inappropriate affect were significantly more severe among young-onset subjects (F=3.01, df=1,257, P=0.003; F=3.0, df=1,257, P=0.003, respectively). The negative symptoms of alogia and avolition were also significantly more severe among the younger-onset group (F=3.4, df=1,257, P=0.0008; F=3.0, df=1,257, P=0.003, respectively). Symptom ratings of the positive symptoms of hallucinations and delusions did not differ between the subject groups (Table 2). These data suggest that the younger-onset individuals have characteristic features within the negative and disorganized symptom dimensions.
In a second analysis, the age at onset of symptoms was used as a continuous variable in a multiple regression procedure. This model examined the influence of age at onset on the three symptom dimensions. The model demonstrated that age at onset significantly influenced symptom presentation in the disorganized and negative dimensions (F=13.06, df=1,255, P=0.0004; F=4.89, df=1,255, P=0.028, respectively). This relationship was in the negative direction; that is, greater severity of disorganized and negative symptoms was associated with a younger age at onset.
The age at the time of evaluation was also examined as a continuous variable in a multiple regression model to determine its impact on symptom severity and whether it interacted with age at onset. This aspect of the analysis sought to determine whether perhaps there was a confounding influence of the age at the time the person was assessed. In this analysis, it was observed that older age at the time of assessment was significantly associated with less severe positive symptoms (F=19.2, df=1,255, P=0.0001). However, age at the time of assessment did not interact with the effect of age at onset on any symptom severity, nor did it have a main effect on negative and disorganized symptoms in this sample.
To try to determine whether the group differences could have been accounted for by a longer duration of illness in the early-onset group, a regression analysis was also performed using the total months' duration of illness as a dependent measure. A separate regression was performed for each of the three symptom dimensions. The outcome measure was symptom severity, with illness duration, age at onset, and the interaction term for duration and age at onset included in the model. This analysis demonstrated no significant interaction between illness duration and age at onset in predicting symptom severity in any of the three dimensions. The effect of age at onset continued to be significant for the disorganized and negative dimensions after controlling for illness duration (F=13.2, df=1,255, P=0.0003; F=6.12, df=1,255, P=0.014, respectively). Similarly to the age effects noted above, illness duration influenced psychotic symptoms in the negative direction (F=19.4, df=1,255, P<0.0001).
DISCUSSION
Traditionally, the features thought to characterize late-onset (after age 45 years) from early-onset schizophrenia have been the presence of less affective flattening, less disorganization, fewer negative symptoms, a greater likelihood of paranoid delusions, and overall a less severe course in terms of symptom severity and deterioration. There have been a number of different age criteria designated for “late life.” These have included age 40 to 60 for late-onset schizophrenia as coined by Manfred Bleuler, and age 60 as the starting point for “late paraphrenia” as designated by Roth. The apparent existence of differences with multiple starting points suggests that there may be a continuum of factors at work that may come into play earlier in life. In this study, the pattern of differences observed between the young and intermediate groups was similar to the pattern of differences that one would expect between the traditional early-onset versus late-onset subtypes—namely, less severity of negative and disorganized symptoms among the intermediate-onset patients.
The disorganized dimension perhaps warrants discussion. Previous studies have observed that disorganization is infrequent among late-onset patients. For example, Pearlson et al.11 reported the rate of thought disorder among late-onset patients to be only 6% compared with 52% among young-onset patients. Furthermore, when young-onset individuals were assessed in late life, the rate remained the same (55%), suggesting a stable trait associated with the early-onset illness. Similarly, in the present analysis, although we find that disorganization is significantly less likely to occur among the intermediate-onset subjects compared with earlier-onset patients, disorganization remained present for early-onset patients even when they were assessed in midlife.
There are several ways to conceptualize this “intermediate-onset” syndrome. These patients may represent a mix of individuals, of whom some could be considered to have the same illness symptomatically as typical early-onset patients, while others could have a syndrome that reflects the “paraphrenic” picture associated with the late-onset group of individuals. From another standpoint, this intermediate group could be viewed as patients who are experiencing the same pathologic processes that occur in young-onset schizophrenia, but because the processes are giving rise to symptoms at a later point in life, the individual is less severely impaired. The intermediate-onset patient would have the opportunity to undergo a longer period of normal neural development and maturation with a longer period of normal social function, which may not only confer a less severe course of functional impairment but also affect the nature of the symptoms themselves. For example, developmental factors may account for the greater affective component and the lesser severity of negative symptoms. One could also surmise that the onset of illness may have to occur at a certain juncture in brain development for the presence of formal thought disorder to occur.
One other interesting aspect of this analysis was that age at the time of intake did not influence the relationship between age at onset and clinical features. This finding may reflect a relative consistency within individual patients in symptom features across the course of illness. That is, early-onset patients displayed greater severity of negative and disorganized symptoms whether they were examined as younger adults or somewhat later in life—raising the possibility that age at onset predicts a characteristic symptom picture that is persistent with age. It could be argued that because later-onset individuals tend to have a shorter duration of illness at the time of evaluation, one might misinterpret differences that actually may be related to adverse effects of prolonged illness or medication exposure on the presentation of earlier-onset individuals. However, in our sample the groups did not differ substantially in duration of illness. Furthermore, when we examined the influence of age at onset on symptom severity while controlling for duration of illness, the findings remained the same.
The most clinically meaningful inference from this study is that it may be possible to identify distinct symptomatic and prognostic groups in young to mid-adulthood on the basis of age at onset. This notion further suggests that age at onset may factor into treatment recommendations as newer medications are increasingly examined in terms of differential effects on various symptoms clusters. That is, the observation that mid- to later-life syndromes are characterized by more frequent psychotic symptoms such as delusions, whereas early-onset syndromes require interventions for negative symptoms, may be meaningful in terms of selecting treatment with novel agents. Additionally, from a research standpoint, a better understanding of the “gray zone” (i.e., mid-life) in schizophrenia may be helpful in distinguishing how the probable neurodevelopmental pathology manifests through maturation and into age-related neurodegeneration.
 |
 |
1 Kraepelin E: Dementia Praecox and Paraphrenia (1919), translated by Barclay RM, edited by Robertson GM. New York, Robert E Krieger, 1971Google Scholar
2 Roth M: The natural history of mental disorders in old age. J Ment Sci 1955; 101:281–301Crossref, Medline, Google Scholar
3 Harris MJ, Jeste DV: Late-onset schizophrenia: an overview. Schizophr Bull 1988, 14:39–55Google Scholar
4 Jeste DV, Harris MJ, Krull A, et al: Clinical and neuropsychological characteristics of patients with late-onset schizophrenia. Am J Psychiatry 1995; 152:722–730Crossref, Medline, Google Scholar
5 Riecher-Rossler A, Rossler W, Forstl H, et al: Late-onset schizophrenia and late paraphrenia. Schizophr Bull 1995; 21:345–354Crossref, Medline, Google Scholar
6 Bleuler M: Late schizophrenic clinical pictures. Forschritte der Neurologie und Psychiatrie 1943; 15:259–290Google Scholar
7 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, revised. Washington, DC, American Psychiatric Association, 1987Google Scholar
8 Andreasen NC: The Scale for the Assessment of Negative Symptoms (SANS). Iowa City, IA, The University of Iowa, 1983Google Scholar
9 Andreasen NC: The Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, IA, The University of Iowa, 1984Google Scholar
10 Andreasen NC: Comprehensive Assessment of Symptoms and History (CASH). Iowa City, IA, The University of Iowa, 1985Google Scholar
11 Pearlson GD, Kreger L, Rabins PV, et al: A chart review study of late-onset and early-onset schizophrenia. Am J Psychiatry 1989; 146:1568–1574Google Scholar