A Critical Review of Memory Stimulation Programs in Alzheimer's Disease
Abstract
The authors describe the memory stimulation programs used in the treatment of Alzheimer's disease (AD) and review their efficacy. Visual imagery, errorless learning, dyadic approaches, spaced retrieval techniques, encoding specificity with cognitive support at retrieval, and external memory aids were the memory stimulation programs used alone or in combination in AD. Preliminary evidence suggests that the errorless learning, spaced retrieval, and vanishing cues techniques and the dyadic approach, used alone or in combination, are efficacious in stimulating memory in patients with AD.
Many reviews have been published on the effects of cognitive stimulation programs in populations suffering from traumatic brain injuries1–3 and strokes.4,5 However, few authors have examined the efficacy of these programs for patients with dementia. Much work has been done since publication in the early 1990s of reviews by Arkin6 and Bäckman,7 both of which found promise in this area. More recently, De Vreese et al.8 reviewed data from 1995 to 2000, although they presented only a few types of stimulation programs: the expanding rehearsal technique, vanishing cues, errorless learning, sensory motor skill stimulation, and external memory aids. No papers have been published in recent years that fully review and compare the efficacy of various cognitive stimulation programs in the treatment of Alzheimer's disease (AD).
Early and accurate clinical diagnosis of dementias as well as knowledge about the cognitive mechanisms involved, especially the memory systems, have greatly improved over the past 25 years.9 As Clare et al.10 have noted, the growing emphasis on early detection and diagnosis of dementia highlights the need for effective psychological interventions for people in the early stages of AD. Even in the mild phase of dementia, these individuals have significant episodic memory impairments: the encoding and retrieval capacities, as measured with the free and cued recall, as well as recognition paradigms, are the most impaired functions of episodic memory early in the AD course.11 The atrophy or alteration of the medial temporal lobe (limbic system) is usually responsible for the early impairments of episodic memory.12–16 However, motor skill learning, some implicit memory capacities,8,17–19 and the functioning of the articulatory loop of working memory20 are preserved in mild AD. Therefore, one can expect some potential for memory remediation or compensation at least in the early phases of AD. In this paper we review the efficacy of cognitive interventions for enhancing memory functions in the mild to moderate stages of AD.
The paper has two parts. In the first part, we present descriptions, as well as the theoretical basis, of the various stimulation strategies or programs that have been studied in patients with Alzheimer's disease. In the second part, we review the evidence on the efficacy of these programs with the AD population. We then conclude critical comments and recommendations for future programs and research.
METHOD
MEDLINE (1971–2001) and PsycINFO (1887–2001) were searched using the following terms: memory remediation; memory remediation and dementia; cognitive remediation; cognitive remediation and dementia; Wilson, Barbara; Sandman, Curt; Camp, Cameron; Quayhagen, Mary; vanishing cues; spaced retrieval; errorless learning; cue utilization and Alzheimer's disease; and visual imagery and Alzheimer's disease. For the first four items, the search was also performed using the terms “stimulation” and “rehabilitation” instead of “remediation.” In addition, we conducted a manual search of the references listed in the articles to identify other appropriate articles. Articles were included in our review only if they met the following criteria: the population studied was suffering only from Alzheimer's disease; a structured cognitive rehabilitation program was described and applied or external memory aids were used; the presented data were specific to the questions; cognitive rehabilitation was used as an intervention; and the article was written in English or in French. Articles were excluded if they used a reality orientation approach; if they included subjects with more than one type of dementia or with dementia and other neuropathological processes; or if they pooled results from various populations having different neuropathological processes. Two articles21,22 were rejected because the data on AD were not distinct from the data on other dementias (vascular dementia, multi-infarct dementia, and Parkinson's disease). Our approach was to conduct a qualitative review of the evidence. A meta-analysis would have been less appropriate and instructive than a qualitative analysis, because most of the studies (11 of 18) used very small samples (n≤11) as well as a patient-centered approach adapted to the needs of the individual patient.
PROGRAM DESCRIPTIONS
Several memory remediation or stimulation programs have been developed to compensate for the impairments associated with some necessary skills involved in the process of learning, such as the encoding and retrieval capacities. These capacities are typically altered in classical amnesic syndromes23–25 and in illnesses such as AD, causing severe memory problems and other cognitive deficits. The theoretical goal of the strategies reported in the literature is to improve or support damaged functions in order to facilitate new learning. These different strategies have not yet been used to strengthen or improve areas not damaged, but they can partially rely on these undamaged areas (such as implicit memory) to carry on the training and improve learning capacity. Some remediation strategies were conceptualized in order to facilitate the encoding process: the encoding specificity strategies with cognitive support in episodic remembering,26–28 the errorless learning approach,29,30 and the visual imagery techniques.31 Other strategies have been developed in order to enhance the retrieval capacities: the spaced retrieval technique, also called the expanding rehearsal method or the expanded retrieval practice,32–34 the vanishing cues technique,35,36 and various external memory aids such as memory books, prompts,37,38 computers, and NeuroPage, a radio paging system that sends reminders.39,40 Finally, the dyadic remediation program is a remote form of prosthetic memory aid, derived from a cognitive behavioral therapy approach,41 in which a caregiver or familiar partner becomes instrumental in carrying out different internal memory stimulation programs with the amnesic patient.42,43
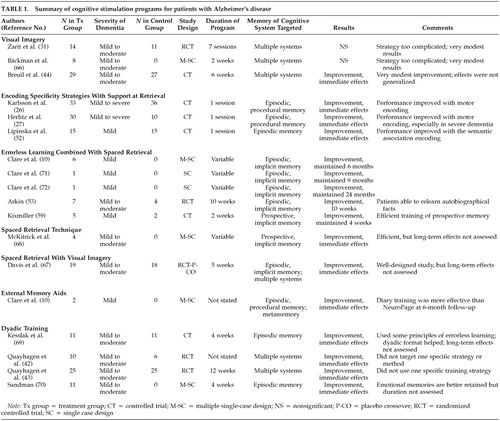
The memory training programs can be used individually or in combination. For this review, they are grouped in seven categories as found in the literature (Table 1): visual imagery techniques; encoding specificity strategies with cognitive support in episodic remembering; the errorless learning approach combined with the spaced retrieval technique; the spaced retrieval technique; the spaced retrieval technique with visual imagery; external memory aids; and patient-caregiver dyads for significant events, active memory recall and recognition exercises, interpersonal problem-solving situations, and targeted conversation exercises.
Visual Imagery
The use of visual imagery techniques is based on the concept that visual associations improve the encoding, consolidation, and recall capacities of verbal material because the memory system does not rely on the verbal semantic mode alone. According to Breuil et al.,44 even when several cognitive functions are compromised in AD, patients are still able to elaborate some cognitive strategies. Recall failures would occur because the retrieval strategies are not well applied. Thus, mental imagery is used to simultaneously stimulate visual and verbal semantic modes to facilitate the encoding, consolidation, and retrieval capacities in the everyday environment. Since many systems (mainly the visual and verbal semantic systems) are stimulated with visual imagery, generalization of learning from one environment to another or from one type of information to another has been hypothesized to occur.44 Examples of visual imagery include asking a subject to pay attention to specific visual details of the information being learned (focus on facial features, for example) or to form a mental image of an object presented in the verbal modality.
Encoding Specificity With Support at Retrieval
These strategies were developed to provide supportive conditions at both encoding and retrieval phases of episodic learning. The encoding specificity paradigm necessitates the use of similar cues for acquisition (or encoding) and retrieval,27,45–47 since this paradigm holds that the amount of informational overlap between a cue presented at retrieval and the memory representation established at encoding is critical to episodic memory proficiency.48 In other words, the more congruent a cue is with the context prevailing during encoding or with the cognitive operations carried at encoding, the more effective it will be at retrieval. Early studies have shown a modest, almost nonsignificant improvement of recall in subjects with mild and moderate AD when the same semantic cues were provided by the experimenter at encoding and retrieval.45,49,50 The lack of efficacy of the experimenter-provided semantic cues in subjects with dementia has been attributed to a semantic encoding specificity deficit early in the AD process.46,47,50 On the other hand, the self-generated cues with encoding-retrieval compatibility have been hypothesized to optimize episodic recall in AD because an elaborative activity is taking place at encoding.51 Self-generated cueing strategies were then developed to be used similarly at encoding and retrieval: self-generated and semantic cues, that is, choice of category or description of the item to be remembered by the subject;27,52 self-generated and motor cues, that is, pantomime of the movements associated with the use of the object to be remembered;26,27 or combinations of these cues.27 In this paper we review only the articles using self-generated cues.
The Errorless Learning Approach
The errorless learning approach favors the elimination or reduction of incorrect or inappropriate responses during memory training.10,53 In other words, using this paradigm, subjects are not allowed to commit errors when they are receiving memory training. This technique was first designed to facilitate the acquisition of new information in individuals with learning disabilities, and it was successfully adapted to memory training in subjects who had suffered brain injuries.10,30,54–56 Clare et al.10 have adapted this method for patients with AD. With errors kept to a minimum during the training, it is hypothesized that interferences in the memory stores will be avoided, which will facilitate the encoding process of new information. Learning, retention, and retrieval should thus be easier.30 Baddeley and Wilson30 have shown that errorless learning improves the learning process in subjects with amnesia. The errorless learning training program is often conducted in conjunction with the spaced retrieval technique or the vanishing cues technique. In the errorless learning programs, subjects are instructed to say that they do not know an answer instead of giving a wrong answer; they are encouraged not to guess.
The Vanishing Cues Technique
The vanishing cues technique consists of several attempts to recall information, using prompts that are gradually decreased until recall is successfully achieved. This method is mainly based on two well-established and related principles: the backward chaining procedure of behavioral modification56,57 and some preservation of implicit memory in subjects with amnesia.37 Some authors view the vanishing cues technique as a complementary method to achieve an errorless learning training.58 An example of the vanishing cues technique is to first present complete words to the subject and then ask him to say the word when the last letter or last few letters are missing. Wilson56 provides the following example: PEGGY is first presented, then PEGG_, then PEG_ _, and so on.
The Spaced Retrieval Technique
The spaced retrieval technique or the expanded retrieval practice involves testing for the repeated recall of newly acquired information at increasingly longer intervals32,33,59 or with an increasing number of intervening items.60,61 This technique is based on experimental evidence suggesting that the longer the distracting interval between the first and the second successful recall, the greater the likelihood of recall at a third recall attempt.62 The expanded retrieval practice also potentially contains a practice effect and therefore implies some preservation of implicit/procedural memory, since the subjects repeat the same items over different trials. In this method, the subject is asked to recall the information with increasing numbers of intervening items (for example, zero, three, … nine, and so on interpolated items between recalls of the learned item) or at increasing intervals of time (for example, 5 seconds, 10 seconds, … 60 seconds, and so on after presentation of the item to learn, or 2, 4,…20 days after the last test). In terms of the time interval between recalls, the subject has either to reach a predetermined goal (for example, 60 seconds or 20 days) or to increase the time interval until he or she can no longer recall the information.
External Memory Aids
It may be difficult for subjects with amnesia to maintain the use of internal memory strategies, and therefore the potential of external memory aids might become more important. Indeed, external memory aids have been widely used with populations with traumatic brain injury or stroke.37–40,63 Some individuals in the early stages of AD report an increase in the spontaneous use of simple external memory aids, such as notes they write to themselves or a calendar they use to remember appointments or to remind them of important dates. Most patients with AD increase their reliance on their caregivers as a form of external memory aid.64 Using external aids nevertheless involves memory, especially metamemory and prospective memory, as well as some executive functioning, since the subjects must be aware of their memory problems and remember to record information as well as how and when to access this information. To overcome these difficulties, Hersh and Treadgold65 devised a radio paging system that involves an arrangement of microcomputers linked to a conventional computer memory and, by modem, to a paging company. Reminders for each individual using the system are entered into the computer and, at the appropriate date and time, transmitted to an individual alphanumeric pager. An audio or vibration alarm alerts the wearer that the pager contains a reminder of a task to be carried out. The pager is clipped on a waistband or carried in a pocket. Until recently, the efficacy of the NeuroPage had principally been studied in subjects with traumatic brain injury or stroke,39,63 although one study has reported on use of technology with AD patients.10
The Dyadic Approach
In the dyadic approach, the patient's caregiver becomes instrumental in carrying out different memory and cognitive improvement strategies. These strategies are used for several purposes: to facilitate the recall of significant life events; to improve memory functioning through visual and verbal mnemonic strategies designed to facilitate recall and recognition; to improve executive functioning through problem-solving exercises using planning, conceptualization, and classification within the context of interpersonal skills; and to increase social interaction by improving communication skills with targeted conversation exercises of word fluency and verbal exchange.9 In the reviewed literature, some specific memory training procedures can be used within the dyadic approach, but the training and theoretical focus are more on the patient-caregiver dyad than on the memory systems.
REVIEW OF THE EVIDENCE ON EFFICACY
We identified 17 articles that pertained to memory improvement programs used with AD patients. Table 1 presents the results obtained with the different memory remediation programs. One article10 contained results on two methods; they are reported separately in the table. Thus Table 1 provides results for 18 different studies. The severity of dementia varied from mild to moderate in 17 reviewed studies,10,26,27,31,42–44,51,53,59,66–72 with MMSE scores ranging from 9 to 29. Two studies also included subjects with severe dementia.26,27 In all studies memory assessments were performed at baseline, before the training took place, both in order to make the diagnosis of dementia and to specifically define the memory problems. However, in most of the studies, these extensive evaluations were not carried out again at the end of the training programs or, if they were, the results were not provided. Only six studies provided data on a long-term follow-up extensive memory assessment.10,42,43,53,59,67 None of the patients were reported to be on cognition-enhancing drugs in these studies.
Visual Imagery
Three studies used visual imagery–based mnemonic techniques as memory stimulation programs in dementia.31,44,66 The study by Zarit et al.31 involved 14 patients with AD in a didactic visual-imagery training group, 11 patients with AD in a problem-solving group, and 10 patients with AD in a waiting-list control group. The patients were randomly assigned to the treatment and waiting-list control groups. The training was carried out in dyads, in seven 90-minute sessions. The visual imagery tasks consisted of forming mental images of words that subjects had to remember. The problem-solving tasks consisted of learning how to take practical steps to manage day-to-day problems caused by the memory loss. Recall and recognition tasks of 15 items were used to assess memory at baseline and at the end of the training sessions, along with the Memory and Behavior Problems Checklist, to assess the impact of the training on everyday functioning capacity. The subjects in the didactic visual-imagery condition significantly improved their recall performance during the training sessions, but most of the gains had been lost by the time of the posttraining assessment. On the recall trials, the subjects in this group retained a mean of 2.4 of 15 items at baseline, a mean of 6.6 items at midtraining, and a mean of 2.4 items at posttraining evaluations. On the recognition trials, these subjects retained a mean of 4.7 of 15 items at baseline, a mean of 5.7 items at midtraining, and a mean of 5.3 items at posttraining evaluations. Overall, the memory results were mediocre, and the impact on everyday functioning capacity was not encouraging. Using the same measures, no positive effects were noted in the other two groups. There was no longitudinal follow-up to measure long-term retention of the items.
Bäckman et al.66 included eight subjects with AD in their imagery-based mnemonic training of face-name associations. There was no control group. The patients were given 6 minutes to study pictures of faces presented on cards, and they had to identify a distinctive facial feature on each card in order to create a visual association with the name of the individual shown in the picture. There was no time limit for the duration of the training. The authors did not provide the total number of pictures presented to each patient. The goal of the study was to increase the time that a face-name association could be held in memory. The authors found that the retention time of face-name associations increased in only one of the eight subjects (from 3 minutes and 30 seconds at baseline to 21 minutes and 30 seconds after training). Thus, the outcome of the training was not at all encouraging. No other subjects benefited from the training. There was no generalization of the training to other memory functions as measured by the Boston Naming Test, a word fluency task, and the Benton Visual Retention Test, Form A.
The study of Breuil et al.44 involved 29 subjects with AD in a stimulation group and 27 subjects with AD in a non-stimulation group. The stimulation training was carried out in 10 sessions each lasting 60 minutes. The authors described their method as a global stimulation program that relies strongly on mental imagery. Various perceptual modalities were stimulated through visual imagery and semantic priming. The subjects had to first connect dots to form an umbrella and were then asked to draw an upside-down, closed umbrella, to evoke associated words, to talk about rainy months, and to talk about regions of the country associated with rainfall. The subjects were also asked to mention and visualize characteristic aspects of the geographic region, such as the main cities, foods, and cultural events. Subjects were also asked to name objects presented on pictures, to classify them into categories (e.g., fruits, vegetables, and the like), to name all the objects belonging to a specific semantic category, and to provide names of fruits from other countries. The nonstimulation group received no cognitive stimulation. Breuil et al. reported an improvement of the total MMSE scores in the stimulated group after the training (the scores were not provided, however) and immediate positive effects on the Word List Memory Test (P=0.09). No other improvements were noted in the other areas measured, which were verbal fluency and activities of daily living.
In summary, the three studies using visual imagery techniques registered mediocre results, despite the fact that the authors of two of the studies reported some kind of improvement.
Encoding Specificity With Support at Retrieval
We reviewed three studies that used the encoding specificity strategies with cognitive support at retrieval in patients with AD.26,27,51 The severity of dementia varied from mild26,27,51 to moderate26,27 and severe.26,27 The three studies specifically targeted episodic and semantic memory, since the subjects had to learn lists of words or objects. All the studies examined the effects of different encoding conditions on performance at retrieval with the free and cued recall paradigms as well as the encoding-retrieval compatibility paradigm.
The study by Karlsson et al.26 included subjects with mild (n = 12), moderate (n = 17), and severe (n = 14) AD as well as 36 healthy older adults. Each subject received one training session and was asked to remember tasks performed using a given object (subject performed task, or SPT; for example, lift the cup) or to remember verbal material. The authors referred to these methods as, respectively, motor coding and verbal coding. Half of the subjects in each group received the SPT instructions, and the other half received the verbal task. Each subject in the SPT group was presented with 25 objects (belonging to five semantic categories), one at a time, which they had to manipulate according to the verbal instructions given by the experimenter. After the presentation of the last item, the subjects had 5 minutes for free recall of as many items as possible. A cued recall trial with semantic category cues was then administered. The results showed a significant effect of the task (SPT versus verbal task) in the three groups with AD and in the control group. The groups with mild, moderate, and severe AD as well as the control group performed significantly better on the SPTs than on the verbal tasks (P<0.05) and significantly better on these tasks in the cued recall than in the free recall condition (P<0.05). The authors concluded that motor coding, but not verbal coding, improves free recall and cued recall in normal older adults as well as in patients with AD, thus supporting the idea that in order to demonstrate memory enhancement in AD, it is necessary to provide a substantial amount of environmental support as a guidance process for remembering. It may be that motor coding counteracts some of the severe attentional and semantic memory deficits associated with AD.26 There was no longitudinal follow-up of this learning training.
The study by Herlitz et al.27 included subjects with mild (n = 10; mean MMSE score, 24.5), moderate (n = 10; mean MMSE score, 16.6), and severe AD (n = 10; mean MMSE score, 6.6) as well as healthy control subjects (n = 10; mean MMSE score, 29.7). All subjects experienced, in a single learning training session, five different encoding conditions: in the verbal encoding condition, the subject listened to a list of nouns read by the experimenter and read the corresponding words on cards, one at a time; in the object encoding condition, the subject was presented with the actual objects and had to name them; in the semantic encoding condition, the subject was presented with the objects and was asked to answer questions about their functional use; in the semantic/motoric condition, the subject was presented with the objects and asked to motorically demonstrate how to use them; and in the motoric condition, the subject had to use presented objects according to the experimenter-provided instructions. The goal of the study was to assess which encoding condition provided the best retention and recall performance, using the free and cued recall paradigms. After each condition, subjects were asked to free-recall all items they could remember during a 2-minute period. A cued recall was then immediately carried out whereby the semantic category names were provided as cues. Using the free recall paradigm, the patients with mild, moderate, and severe AD recalled, respectively, from 35% to 40% (best performance in the object condition), from 15% to 30% (best performance in the verbal condition), and from 0% to 5% of the items (best performance in the verbal condition). Using the cued recall paradigm, the patients with mild, moderate, and severe AD recalled, respectively, from 40% to 60%, from 20% to 35%, and from 2% to 20% of the items (best performance in the motoric condition). Although the recall performance of subjects with AD significantly benefited (P<0.001) from the cued recall paradigm, there was no significant effect of the encoding conditions in subjects with mild and moderate dementia. Only the patients with severe AD significantly improved their cued recall performance in the motoric condition (P<0.01). In comparison, the control subjects recalled 60% to 80% of the items using the free recall paradigm and 70% to 90% of the items using the cued recall paradigm. The controls significantly improved their performance in the semantic and semantic/motoric conditions as compared with the verbal condition (P<0.01). The authors concluded that patients with mild AD are able to utilize cues to increase retrieval performance after poor (i.e., verbal) as well as rich (i.e., semantic) encoding conditions; that patients with moderate AD are able to benefit from cues after all forms of encoding, with the exception of pure verbal encoding; and that patients with severe AD are able to utilize cues only after motoric encoding. There was no longitudinal follow-up of the learning training.
The study by Lipinska et al.51 included 15 subjects with mild AD and 15 older healthy control subjects. During a single session, subjects were shown 20 photographs, representing common objects, for 30 seconds each. To realize the process of self-generated semantic encoding specificity, the subjects were asked to name the first 10 pictures (the naming condition) and for the remaining 10 pictures were instructed to name the objects and to select, from two possible alternatives, the semantic category to which they belonged (the naming + category decision condition). At the retrieval phase, the subjects were first asked to freely recall as many object names as possible from the list. They then had a cued recall trial in which they were provided with semantic category cues similar to those used at the encoding phase (encoding-retrieval compatibility). Finally, subjects had a four-alternative multiple-choice recognition trial in which each target item was presented in a booklet along with three distracting items. In the poorest encoding-retrieval condition—the naming condition—using the free recall paradigm, patients with AD remembered 6.7% of the information, whereas the control subjects recalled 11.3%. Comparatively, in the richest encoding-retrieval condition—the naming + category decision condition—using the recognition paradigm, patients with AD recognized 68% of the information, whereas the control subjects recognized 67.3% of the information. The authors did not mention whether there was any significant difference between groups. Only the performance of subjects with AD significantly (P<0.05) benefited from the richest encoding situation (naming + category decision condition) in cued recall and recognition trials. In this study, patients with AD, as opposed to the normal older subjects, showed an effect of the encoding manipulation. For the normal older subjects, the requirement of naming appeared to be sufficient to optimize performance. These results suggest that patients with AD need more cognitive support at encoding than normal older adults to make effective use of cues at retrieval. The overall low numbers recorded in recall trials could have been the result of the relatively short presentation of the stimulus during learning. There was no longitudinal follow-up of this learning session.
In summary, the three studies using the encoding specificity strategies with cognitive support at retrieval found that subjects with mild to moderate AD best benefited from the richest encoding and retrieval conditions, that is, with semantic and motor encoding accompanied by a cued recall or recognition paradigm. The motor encoding was especially efficient in patients with severe AD.
The Errorless Learning Approach Combined With the Spaced Retrieval Technique
Five studies using errorless learning and spaced retrieval techniques together are reported in the literature: the studies of Arkin,53 Clare et al.,10,71,72 and Kixmiller.59 The information to be learned consisted of autobiographical information;10,53 various information such as names of people71,72 and how to use a calendar;10 and future appointments.59 Thus, the focus of the first four studies10,53,71,72 was on episodic memory, and the target of the third59 was prospective memory.
The study by Clare et al.10 included six experimental subjects in a multiple single-case study with an experimental design. Internal memory training was used with four subjects, and external memory aids training was used with the other two (results are presented separately in Table 1). For the subjects undergoing internal memory training, the information to be learned consisted of names of participants of social clubs, names of participants of a support group, names of famous people, and various personal information (episodic memory). One training session was provided for every item to be learned, and the length of the sessions varied according to the information presented. A recall test trial consisting of all items was administered at the end of each training session. Follow-up assessments were scheduled 1, 3, and 6 months after completion of the intervention. The results were based on the mean proportion (%) of correct responses. The four patients were able to significantly increase the amount of information to be learned, from approximately 20% to 60% of the information. The results were maintained at the 6-month follow-up evaluation. The subjects' neuropsychological scores were not reported, but the authors mentioned that no significant changes occurred in the global cognitive profile of three of the subjects when compared with baseline data. A deterioration of the global cognitive profile was recorded for one patient.
Clare et al.71 used an errorless learning and spaced retrieval approach in a case study to help a 72-year-old patient with mild AD learn the names of the 14 people in his social club. At a baseline presentation of the pictures, the subject knew the names of three members. These three pictures were retained for practice purposes during training. The remaining 11 faces were learned over 21 sessions. Sessions took place twice weekly; one new picture was added every week, and one session per week was used for practice. The length of the session varied depending on the time the subject required to learn the name. The subject was asked to give an answer only if he was sure; prompts in the form of vanishing cues were provided in the case he was uncertain. Recall was then asked, without prompts, using the expanded rehearsal method. The authors described the initial intervals as short but gradually increasing until a 10-minute interval was reached. Home practice was encouraged. Follow-up sessions were conducted at 1, 3, 6, and 9 months after the end of the training sessions. The subject recalled 20% of the information at baseline (three of 14 pictures). He was able to learn and retain all 14 names by the end of training (session 21), and he remembered 98% of the names over the posttests 1, 3, 6, and 9 months later. A follow-up study72 found that the patient was able to retain 70% of the names over a 2-year period. The 1999 report by Clare et al.71 was the first to show gains with the AD population using errorless learning and spaced retrieval techniques combined, and the 2001 follow-up report72 was the first to show that these gains can be maintained over 2 years. These data suggest that errorless learning and spaced retrieval can be useful methods for stimulating new and relatively durable learning in patients with AD despite the degenerative nature of the illness.
The study by Arkin53 included seven subjects in the memory training group and four in the control group. The control subjects met with the experimenter but received no specific memory training. A random assignment procedure provided homogeneous groups with all of the lower-functioning individuals in the same group. The author then assigned the subjects to the experimental and control groups in order to obtain heterogeneous groups. A single-case experimental design was used because the patients had to relearn 32 autobiographical facts (episodic and autobiographical memory) recorded on tapes for each subject. This information was obtained from the patient and his or her caregiver. The information was learned using an errorless approach and the spaced retrieval technique. For the spaced retrieval technique, the authors did not provide information about the time intervals between recall trials or the longest time interval to be achieved. A research student administered the tape-recorded exercise once a week for ten consecutive weeks; the exercise took approximately 20 minutes. The number of facts learned by the end of the 10-week training program was recorded. At baseline, the experimenters made sure that each subject knew at least 16 of the 32 (50%) autobiographical facts; the subjects had to learn the remaining 16 facts. Of the 16 facts left to be learned, the seven subjects in the memory training group learned from seven to 13 facts. These results were significant when compared with the control group. (The mean scores of the control subjects remained unchanged after 10 weeks.) For most subjects in the training group, memory functioning improved most between the third and the fourth session, or 3 to 4 weeks after baseline.
Kixmiller59 included five patients with mild AD in the experimental group and two patients with mild AD in the control group of errorless learning and spaced retrieval training program. Six training sessions, each lasting from 30 to 120 minutes, were conducted over two weeks in the patients' homes. The length of the training session depended on the length of time the subject needed to complete the task without making errors. In both the experimental and control groups, subjects had to learn how to write down appointments, take medication, and remember future important dates (prospective memory). The experimental training included observation, modeling, verbal prompt, self-instruction, independent trials with feedback, drilling with self-instructions, and trials in which subjects carried out tasks independently. Patients were prevented from making errors during training. The control group received instructions in general memory strategies, memory questionnaires, and verbal descriptions of the tasks to learn, and they independently completed the tasks. A spaced retrieval technique was also used for posttests. Recall trials were attempted immediately after training and then 3, 4, and 7 weeks after the completion of the training. Only the experimental training group improved performance on specific, prospective memory tasks. By the end of training, the participants who received memory training completed 79% of the required tasks, whereas the control group completed 14% of the tasks. The effects were maintained up to 7 weeks after the treatment in the five experimental subjects.
In summary, the 17 subjects trained with the errorless learning approach combined with the spaced retrieval technique all showed significant improvement in the percentage of information recalled after the training sessions. Of these subjects, 29% reportedly maintained their learning over a 7-week period, 17.6% over a 6-month period, and 0.06% over a 2-year period.
The Spaced Retrieval Technique
One study, that of McKitrick et al.,68 used only the spaced retrieval technique to stimulate memory in AD patients. This study included only four experimental subjects. The researchers' goal was to stimulate prospective memory by asking subjects to remember a task required for the following week. Three different tasks (a different task every week) had to be learned. The duration of the training varied with the participants, because the training was carried out until the subject could retain and recall the information for at least 60 seconds. The intervals were then increased by 30 seconds after each successful recall. The experimental subjects were able to learn 100% of the tasks. This achievement can be considered a success. However, the long-term effects of the memory training were not measured.
The Spaced Retrieval Technique With Visual Imagery
One study, that of Davis et al.,67 used the spaced retrieval technique in combination with visual imagery to stimulate memory in AD patients. This was the first randomized placebo-controlled crossover trial that measured the efficacy of a cognitive stimulation program in patients with AD. The study involved 37 subjects with mild to moderate AD (mean MMSE score, 22.4) randomly assigned to an experimental (n = 19) or a placebo group (n = 18). After an extensive baseline neuropsychological examination, both groups were started on a 5-week memory training program. All subjects first had to recall autobiographical information (seven facts). About half of the patients (19 of 37) did not know these seven autobiographical facts and participated in a spaced retrieval technique training to learn them. Every experimental subject (including those receiving the spaced retrieval training) participated in a “peg” task requiring them to learn three pairs of rhyming numbers and objects (e.g., “1-bun, 2-shoe, 3-tree”). The subjects were then instructed to use the numbers as pegs (reminders) to help them recall the words. Once they completed this task, the subjects were asked to learn the names of three staff members using “pegs” (e.g., “knee” for “Naomi”), to visualize the peg, and to associate this visualization with the person's face. The placebo group was asked to complete exercises such as repeating the alphabet (mock training) during 5 weeks. Every patient was reassessed at the end of the 5-week trial by examiners blind to the experimental conditions. The placebo group then crossed over to receive the 5-week intervention program; only this group was retested a third time by the examiners, who were no longer blind to the experimental conditions.
The performance of the subjects after the training was compared with their performance at baseline on a variety of cognitive tests (MMSE, WMS-R Logical Memory and Visual Reproduction, WAIS-R Digit Span, Verbal Series Attention Test, Controlled Word Association Test, Category Fluency, Finger Tapping Test, and Geriatric Depression Scale). The initial experimental group (IEG) and the placebo group (PG) both improved on five neuropsychological measures, although these improvements did not reach statistical significance, possibly because of the small numbers of patients in each group. The two groups improved on short-term and long-term visual recall, although the improvement of the PG was sometimes greater than that of the IEG. The IEG registered a mean positive change of 2.72 points whereas the PG had a mean positive change of 4.36 points on immediate recall of the visual reproduction subtest. The IEG had a mean positive change of 3.72 points whereas the PG had a change of 2.4 points on delayed recall of the visual reproduction subtest. Only the IEG improved on a measure of verbal attention (from 218.7 to 197.5 seconds on the Verbal Series Attention Test). The improvement in both groups was less impressive on measures of long-term verbal recall and of semantic fluency. The IEG registered a mean change of 1.15 items, and the PG had a change of 1.65 items, on the delayed recall of logical memory subtest. The subjects of the IEG increased their verbal production by a mean of 1.16 words on the Category Fluency task, whereas the subjects of the PG improved by only 0.83 words. The 19 patients who did not know the seven personal facts at baseline were able to learn a mean of 55% of the items after 5 weeks of training, and this finding was significant (P<0.01).
The authors concluded that the spaced retrieval technique showed some efficacy in helping the patients relearn autobiographical information. The authors suggested that practice effects on the tests might explain the improvement of both the experimental and control groups on the other measures. Although this is certainly possible, it does not seem likely that practice effects alone would explain all of the improvement, given the degenerative nature of the memory deficits in AD and the interval of 5 weeks between pre- and posttests. Thus the improvement may have been due in part to some generalization effect of the spaced retrieval technique that was used by the subjects in both the IEG and the PG who needed to learn the autobiographical information. Another possible explanation lies in the simple fact that meeting with an experimenter might improve or maintain functioning independently of cognitive stimulation. There was no longitudinal follow-up to measure the long-term effects of the training.
External Memory Aids
The study by Clare et al.10 included two subjects with AD who used external memory aids. The errorless learning approach, involving regular practice with prompting provided by the caregiver, was used to teach two patients how to use an external memory aid in order to decrease the repetition of questions the patients addressed to their caregivers. One subject had to learn how to use a calendar, and the other had to learn how to use a diary with a NeuroPage. The authors did not report the length and frequency of the training. Assessments took place at baseline, at the end of the training, and 3 and 6 months after the completion of training. The number of questions asked daily by the patients was recorded and used as a measure of efficacy. Only the patient trained with the calendar significantly improved his functioning: he asked a mean of 2.6 questions a day at baseline, 0.75 questions a day at the end of the training, 0.4 questions a day at the 3-month follow-up, and 0.5 questions a day at the 6-month follow-up. The patient trained with the diary and the NeuroPage initially improved his functioning and then registered a decline at the 6-month evaluation: he asked a mean of 1.6 questions a day at baseline, 0.75 questions a day at the end of the training, 0.5 questions a day at the 3-month follow-up, and 2 questions a day at the 6-month follow-up. However, since the number of questions asked by the two patients was relatively low at baseline, one can argue that there was not much room for improvement.
Dyadic Training
Four studies on dyadic training in AD were found. The study by Kesslak et al.69 included 11 subjects with AD and 11 healthy controls. They used dyadic training as well as some principles of errorless learning to teach each patient some episodic information (such as names and interests) about the other participants in the group. The training was thus carried out in a group format, but the patients learned the information through each patient-caregiver dyad. The patients met together the first week, and the following week each patient had to provide information about some other participants of the training program, as shown on individual pictures. The patients were encouraged to practice at home using the patient-caregiver dyad. The investigators did not use a pure errorless approach, since they allowed the patients to make errors but they immediately corrected them. The overall training lasted four weeks; the authors did not provide information about the duration of the individual sessions. The patients improved their performance on name recall during the training: they were able to recall a mean of six names at the second session and seven names at the fourth session, whereas the controls' performance remained the same (they remembered approximately eight names at the second session and at the end of the training). There was a significant improvement by session 2 but no further significant improvements thereafter. There was no longitudinal follow-up.
Quayhagen et al.42,43 mostly used dyadic training as a means of generally improving the cognitive and social functioning of the patients and their caregivers, and therefore they did not target any specific training strategies or memory systems. In an initial pilot study,42 the authors included ten dyads in the experimental group and six dyads in the control group. The subjects were trained with the techniques of conversation, memory-provoking exercises (the authors provided no explanations or details), and problem solving. The authors found that memory improved in the experimental group (a mean of 5.1 items [out of 25] retained on posttesting 4 months after training and 5.3 items retained 8 months after training, compared with 3.7 items retained at baseline). No such improvement was recorded for the control group (respectively, 2.5 items retained at baseline, 2.7 items 4 months after training, and 2.3 items 8 months after training).
In a more recent study, Quayhagen et al.43 used a spaced retrieval technique to perform the memory training part of their cognitive/social stimulation program. This study included 25 experimental, 25 control, and 28 placebo subjects. The placebo subjects observed their caregivers but did not participate in the training exercises (passive approach). The control subjects were placed on a waiting list and had no knowledge of any training at all. The experimental subjects were trained daily with 1-hour sessions of active memory recall and recognition exercises (the authors did not provide any explanations), interpersonal problem-solving situations, and targeted conversational exercises. The training was carried out over 6 days. Results of memory training were measured using the raw scores of the Wechsler Memory Scale–Revised (WMS-R).73 Subjects were tested before and immediately after training and again 9 months later. The experimental subjects improved their nonverbal memory as assessed on the WMS-R (with a mean of 36.7 of 76 items of information retained on the visual reproduction subtest retained at pretraining testing and a mean of 41.4 items retained at the end of training. At the 9-month follow-up evaluation, the performance of the experimental subjects was compared with that of the other two subject groups. The effects of the training were not maintained (36.8 out of 76 items retained in the experimental group versus 32.8 items for the placebo group and 29.4 items for the control group).
Sandman70 included 11 dyads of subjects with AD in a study using primarily a dyadic approach. No control group was used. In this study, an attempt was made to stimulate memory by provoking emotional memories to produce “flashbulb” memories. (The author did not precisely define what are emotional or “flashbulb” memories—that is, the kind of emotions that should have been triggered by the memories, and the required degree of emotional intensity). The patients and caregivers had to pay attention to specific information presented in films or pictures. The pictures contained information about the other subjects in the program. The training was carried out over 4 weeks. The author did not provide information about the duration and weekly frequency of the sessions. Memory was formally assessed at baseline or follow-up with a neuropsychological evaluation. Only the amount of information retained was recorded after the training. This study demonstrated that the emotional memories were best remembered: the patients retained six items in the high arousal condition, compared with approximately two items in the low arousal condition. There was no follow-up evaluation.
In summary, the four studies using a dyadic approach showed an immediate slight improvement of questionable statistical and clinical significance. In the only study that made a follow-up evaluation, the effects of the training were not maintained 9 months after the training.
DISCUSSION
Memory and cognitive stimulation programs have regularly been mentioned in the literature over the past 15 years for the AD population. However, with the exception of a few studies,26,27,31,43,44,51,67 most of the research protocols of the studies we reviewed (61.1%) have involved very small groups of subjects (n ≤ 11), which lack statistical power.
In terms of the assessment of the efficacy of the training, 61.1% (11 out of 18) of the studies reported change only on the specific tests or items for which the subjects had received training to remember.10,26,27,51,53,59,68–72 In the majority of these studies (10 of the 11), the theoretical basis of the training was very well explained and justified, and good, though modest, results were generally reported. In some of these studies the new learned material had no real impact on the life of the patients.26,27,51,70 Nevertheless, the learned or relearned material in other studies10,53,59,68,69,71,72 had some importance in improving the capacity to manage memory problems in everyday life (such as the capacity to remember an appointment or future important dates or to stop asking questions repetitively). Eventually an amelioration of these capacities might have a positive effect on the quality of life of the patients and their caregivers. However, these studies did not measure the possible generalization effect of the memory stimulation training to other memory functions or other cognitive functions, and they did not measure the impact of the cognitive training on measures of quality of life.
Only three studies reported a generalization of the effects of general cognitive stimulation using exclusively standardized cognitive tests, such as memory scales and the MMSE.42–44 The theory underlying these studies was generally weaker in terms of cognitive neuropsychology than the theoretical rationales given in the studies cited in the previous paragraph. In addition, the techniques used to stimulate memory were often only partially described and not well justified by the authors. The obtained results were barely explained, which made them difficult to understand for the readers. For example, in one study,44 the training targeted visual imagery (and thus, to some extent, semantic memory), whereas the posttraining evaluation assessed global cognition as measured by the MMSE, episodic memory (word list), and verbal fluency. The results of this study were limited and reportedly had no effect on the patients' activities of daily living. The biggest challenge in the assessment of the cognitive stimulation programs using this method is the incapacity to directly translate the outcome of the training into specific applications in the patient's life.
Four studies reported the effects of training on both the specific tests or items for which the subjects were trained and on other standard measures of memory and cognition.10,31,66,67 These studies provided measurements of change on both the trained material itself and possible generalization of the training to other areas of memory or cognition. One study demonstrated some statistically nonsignificant amelioration,67 and two other studies showed no deterioration or change compared with baseline on the standard cognitive measures.10,66 Another study reported the absence of a positive impact on functioning in everyday life.31 Interestingly, only two of the studies10,67 reported an improvement in remembering the specific trained items. These results suggest that cognitive stimulation of memory may have an impact on cognition in general, by slightly improving attention and memory functioning67 or by maintaining general cognitive functions,10,31,66 even for a 6-month period.10 These types of results (slight cognitive improvement, maintenance of cognitive function) have been reported in cognition-enhancing drug trials, especially in studies using acetylcholinesterase inhibitors such as donepezil.74
In terms of the results reported, six controlled studies,26,27,44,51,59,69 four randomized controlled studies,42,43,53,67 three studies with a multiple single-case experimental design,10,68,70 and two case studies71,72 have reported positive effects of memory stimulation or remediation programs in AD despite the neurodegenerative impediment. These positive effects were usually registered during or immediately after the memory training26,27,44,51,53,67–70 and were thus limited. At the end of the training, the best results, listed in descending order of effectiveness, were obtained with the errorless learning approach combined with the spaced retrieval technique,10,53,59,71,72 the spaced retrieval technique alone,68 the spaced retrieval technique with visual imagery,67 the richest encoding conditions (semantic/motor and motor) with self-generated cues using the encoding specificity paradigm with cognitive support at retrieval,26,27,51 dyadic training;42,43,69,70 and external aids.10 Although the program of encoding specificity with cognitive support at retrieval showed immediate positive results, the material learned in these studies was more laboratory-type material and therefore not adapted to the needs of the patients, as it was in the other studies using other strategies principally focused on prospective and autobiographical memory.
The positive effects of the memory training were rather modest or nonexistent in the studies using only visual imagery.31,44,66 Visual imagery techniques are usually cognitively complex and effortful. These techniques require a high level of elaborative processing that most patients with brain damage, amnesia, or dementia are unable to achieve spontaneously.25,32 Furthermore, the cerebral areas typically shown to be involved with visual imagery, that is, the bilateral parietal,75 temporal, and occipital association areas,76–79 are also the brain regions impaired in AD,80 and, in the early stages of the disease, particularly the temporal81,82 and parietal association areas.83 Therefore, it might be difficult to use only these techniques with patients in their everyday life.
Only four studies using the errorless learning approach combined with the spaced retrieval technique,10,59,71,72 two studies using the dyadic approach,42,43 and one study using external aids10 provided the results of follow-up assessments. The results of the training were maintained 7 weeks10 to 24 months71,72 after training using the errorless learning with the spaced retrieval techniques, 3 to 6 months using a diary with a NeuroPage or a calendar,10 and 4 to 8 months using the dyadic approach.42 However, the positive results of the training were not maintained 9 months after the dyadic training in one study43 and 6 months after the training with the diary and the NeuroPage.10 Only the studies using errorless learning with spaced retrieval10,53,59,71,72 provided positive effects of training that were consistently maintained over time.
An important limitation of the studies of memory remediation programs in AD is the lack of information about the performance of the subjects on a variety of cognitive measures at the end of the study and, eventually, at long-term follow-up. These extensive and thorough neuropsychological assessments could provide information about a generalization of the effects of the training.
CONCLUSION AND RECOMMENDATIONS
The results from the studies we reviewed suggest that it is possible to stimulate memory in AD. The errorless learning, spaced retrieval, and vanishing cues techniques, together with the dyadic approach, seem to present the best memory training methods for patients with AD. Clearly, there is a need for more randomized controlled studies with memory stimulation programs to validate this treatment approach in the treatment of dementia. On the other hand, one of the major advantages of the client-centered case report approach used in most of the training procedures reported in this review is a training specifically adapted to the needs of the individual subject in his or her everyday life. Long-term follow-up evaluations of the content of the training, as well as exhaustive neuropsychological evaluations at baseline, at the end of the study, and at follow-up, should be a prerequisite in future study designs, since they would serve to assess the long-term effects and the generalization potential of the training procedures.
The dyadic approach could be used to carry out programs using various training techniques concomitantly, such as the errorless learning, spaced retrieval, and vanishing cues techniques. A major advantage of the dyadic approach is that it may provide the caregiver with some information about AD as well as techniques to better deal with the illness. One of the advantages of the errorless learning technique is that patients usually feel good about themselves, since errors are kept to a minimum. Among other things, this boosts self-esteem and reduces frustration in patients with cognitive impairments.6
Although procedural memory is relatively spared in AD,8,17–19 only one study was found to specifically stimulate this memory system.84 We did not include the study in our review, however, because the subjects already knew how to perform the tasks; the goal of the training was to improve the time to complete tasks (activities of daily living, or ADL) rather than to learn new tasks. No study has been found to target procedural memory in order to teach patients with AD how to learn, or relearn, ADL tasks. Future research should examine the efficacy of the combined errorless learning and spaced retrieval techniques in stimulating procedural memory in AD.
An ideal memory training should target information useful to the everyday functioning of the patients and their caregivers, such as activities of daily living,85 and use similar training procedures or techniques for every subject involved in a given program. This approach would permit the design of standardized memory training programs involving larger numbers of subjects and allow the efficacy of these programs to be tested in randomized crossover placebo-controlled trials. Finally, future research should measure the efficacy and the long-term effects of training in patients who are drug naive or on placebo compared with patients taking cognition-enhancing drugs such as donepezil, rivastigmine, and galantamine.
ACKNOWLEDGMENTS
This work was supported by the Jeanne et J.-Louis Levesque doctoral award to Mr. Grandmaison.
 |
1 Carney N, Chesnut RM, Maynard H, et al: Effect of cognitive rehabilitation on outcomes for persons with traumatic brain injury: a systematic review. J Head Trauma Rehabil 1999; 14:277-307Crossref, Medline, Google Scholar
2 Gray DS: Slow-to-recover severe traumatic brain injury: a review of outcomes and rehabilitation effectiveness. Brain Inj 2000; 14:1003-1014Crossref, Medline, Google Scholar
3 Rapoport MJ, Feinstein A: Outcome following traumatic brain injury in the elderly: a critical review. Brain Inj 2000; 14:749-761Crossref, Medline, Google Scholar
4 Calvanio R, Levine P, Petrone P: Elements of cognitive rehabilitation after right hemisphere stroke. Behav Neurol 1993; 11:25-57Google Scholar
5 Ottenbacher KJ, Jannell MS: The results of clinical trials in stroke rehabilitation research. Arch Neurol 1993; 50:37-44Crossref, Medline, Google Scholar
6 Arkin SM: Memory training in early Alzheimer's disease: an optimistic look at the field. Am J Alzheimers Care and Related Disorders and Research 1991; 6:17-25Google Scholar
7 Bäckman L: Memory training and memory improvement in Alzheimer's disease: rules and exceptions. Acta Neurol Scand Suppl 1992; 139:84-89Crossref, Medline, Google Scholar
8 De Vreese LP, Neri M, Fioravanti M, et al: Memory rehabilitation in Alzheimer's disease: a review of progress. Int J Geriatr Psychiatry 2001; 16:794-809Crossref, Medline, Google Scholar
9 Kasl-Godley J, Gatz M: Psychosocial interventions for individuals with dementia: an integration of theory, therapy, and a clinical understanding of dementia. Clin Psychol Rev 2000; 20:755-782Crossref, Medline, Google Scholar
10 Clare L, Wilson BA, Carter G, et al: Intervening with everyday memory problems in dementia of Alzheimer type: an errorless learning approach. J Clin Exp Neuropsychol 2000; 22:132-146Crossref, Medline, Google Scholar
11 Simard M, van Reekum R: Memory assessment in studies of cognition-enhancing drugs for Alzheimer's disease. Drugs Aging 1999; 14:197-230Crossref, Medline, Google Scholar
12 Braak H, Braak E: Neuropathological staging of Alzheimer-related changes. Acta Neuropathol 1991; 82:239-259Crossref, Medline, Google Scholar
13 Damasio AR, Van Hoesen GW, Hyman BT: Reflections on the selectivity of neuropathological changes in Alzheimer's disease, in Molecular Deficits in Alzheimer's-Type Dementia. Edited by Schwartz MF. Cambridge, MA, MIT Press, 1990Google Scholar
14 Deweer B, Lehéricy S, Pillon B, et al: Memory disorders in probable Alzheimer's disease: the role of hippocampal atrophy as shown with MRI. J Neurol Neurosurgery Psychiatry 1995; 58:590-597Crossref, Medline, Google Scholar
15 Hodges JR, Patterson K: Is semantic memory consistently impaired early in the course of AD? Neuroanatomical and diagnostic implications. Neuropsychologia 1995; 33:441-459Crossref, Medline, Google Scholar
16 Jobst KA, Barnetson LPD, Shepstone BJ: Accurate prediction of histologically confirmed Alzheimer's disease and the differential diagnosis of dementia: the use of NINCDS-ADRDA and DSM-III-R criteria, SPECT, X-ray CT, and apoE4 in medial temporal lobe dementias. Int Psychogeriatr 1998; 10:271-302Crossref, Medline, Google Scholar
17 Postle BR, Corkin S, Growdon JH: Intact implicit memory for novel patterns in Alzheimer's disease. Learn Mem 1996; 3:305-312Crossref, Medline, Google Scholar
18 Kuzis G, Sabe L, Tiberti C, et al: Explicit and implicit learning in patients with Alzheimer's disease and Parkinson's disease with dementia. Neuropsychiatry Neuropsychol Behav Neurol 1999; 12:265-269Medline, Google Scholar
19 Verfaellie M, Keane MM, Johnson G: Preserved priming in auditory perceptual identification in Alzheimer's disease. Neuropsychologia 2000; 38:1581-1592Crossref, Medline, Google Scholar
20 Morris RG, Baddeley AD: Comment: primary and working memory functioning in Alzheimer-type dementia. J Clin Exp Neuropsychol 1988; 10:279-296Crossref, Medline, Google Scholar
21 Beck C, Heacock P, Mercer S, et al: The impact of cognitive skills remediation training on persons with Alzheimer's disease or mixed dementia. J Geriatr Psychiatry 1988; 21:73-88Medline, Google Scholar
22 Quayhagen MP, Quayhagen M, Corbeil RR, et al: Coping with dementia: evaluation of four nonpharmacologic interventions. Int Psychogeriatr 2000; 12:249-265Crossref, Medline, Google Scholar
23 Squire LR: Memory and Brain. New York, Oxford University Press, 1987Google Scholar
24 Wilson BA, Baddeley AD: Semantic, episodic, and autobiographical memory in a postmeningitic amnesic patient. Brain Cogn 1988; 8:31-46Crossref, Medline, Google Scholar
25 Baddeley AD: Memory theory and memory therapy, in Clinical Management of Memory Problems, 2nd ed. Edited by Wilson BA, Moffat N. London, Chapman and Hall, 1992, pp 1-31Google Scholar
26 Karlsson T, Bäckman L, Herlitz A, et al: Memory improvement at different stages of Alzheimer's disease. Neuropsychologia 1989; 27:737-742Crossref, Medline, Google Scholar
27 Herlitz A, Adolfsson R, Bäckman L, et al: Cue utilization following different forms of encoding in mildly, moderately, and severely demented patients with Alzheimer's disease. Brain Cogn 1991; 15:119-130Crossref, Medline, Google Scholar
28 Bäckman L: The link between knowledge and remembering in Alzheimer's disease. Scand J Psychol 1998; 39:131-139Crossref, Medline, Google Scholar
29 Wilson BA, Baddeley A, Evans JJ: Errorless learning in the rehabilitation of memory impaired people. Neuropsychol Rehab 1994; 4:307-326Crossref, Google Scholar
30 Baddeley AD, Wilson BA: When implicit learning fails: amnesia and the problem of error elimination. Neuropsychologia 1994; 32:53-68Crossref, Medline, Google Scholar
31 Zarit SH, Zarit JM, Reever KE: Memory training for severe memory loss: effects on senile dementia patients and their families. Gerontologist 1982; 22:373-377Crossref, Medline, Google Scholar
32 Schacter DL, Rich SA, Stampp MS: Remediation of memory disorders: experimental evaluation of the spaced-retrieval technique. J Clin Exp Neuropsychol 1985; 7:79-96Crossref, Medline, Google Scholar
33 Camp CJ: Facilitation of new learning in Alzheimer's disease, in Memory, Aging, and Dementia. Edited by Gilmore SC, Whitehouse PJ, Wykle ML. New York, Springer, 1989, pp 212-225Google Scholar
34 Camp CJ, Foss JW, O'Hanlon AM, et al: Memory interventions for persons with dementia. Appl Cog Psychol 1996; 10:193-210Crossref, Google Scholar
35 Glisky EL, Schacter DL, Tulving E: Learning and retention of computer-related vocabulary in memory-impaired patients: method of vanishing cues. J Clin Exp Neuropsychol 1986; 8:292-312Crossref, Medline, Google Scholar
36 Moffat N: Strategies of memory therapy, in Clinical Management of Memory Problems, 2nd ed. Edited by Wilson BA, Moffat N. London, Chapman and Hall, 1992, pp 87-119Google Scholar
37 Glisky EL, Schacter DL, Tulving E: Computer learning by memory impaired patients: acquisition and retention of complex knowledge. Neuropsychologia 1986; 24:313-328Crossref, Medline, Google Scholar
38 Glisky EL, Schacter D: Acquisition of domain-specific knowledge in organic amnesia: training for computer-related work. Neuropsychologia 1987; 25:893-906Crossref, Google Scholar
39 Wilson BA, Evans JJ, Emslie H, et al: Evaluation of NeuroPage: a new memory aid. J Neurol Neurosurg Psychiatry 1997; 63:113-115Crossref, Medline, Google Scholar
40 Kime SK, Lamb DG, Wilson BA: Use of a comprehensive programme of external cueing to enhance procedural memory in a patient with dense amnesia. Brain Inj 1996; 10:17-25Crossref, Medline, Google Scholar
41 Teri L, Gallagher-Thompson D: Cognitive-behavioural interventions for treatment of depression in Alzheimer's patients. Gerontologist 1991; 31:413-416Crossref, Medline, Google Scholar
42 Quayhagen MP, Quayhagen M: Differential effects of family-based strategies on Alzheimer's disease. Gerontologist 1989; 29:150-155Crossref, Medline, Google Scholar
43 Quayhagen MP, Quayhagen M, Corbeil RR, et al: A dyadic remediation program for care recipients with dementia. Nurs Res 1995; 44:153-159Crossref, Medline, Google Scholar
44 Breuil V, De Rotrou J, Forette F, et al: Cognitive stimulation of patients with dementia: preliminary results. Int J Geriatr Psychiatry 1994; 9:211-217Crossref, Google Scholar
45 Buschke H: Cued recall in amnesia. J Clin Neuropsych 1994; 6:433-440Crossref, Google Scholar
46 Buschke H, Sliwinski M, Kuslanski G, et al: Aging, encoding specificity, and memory change in the Double Memory Test. J Int Neuropsych Soc 1995; 1:483-493Crossref, Medline, Google Scholar
47 Buschke H, Sliwinski MJ, Kuslansky G, et al: Diagnosis of early dementia by the Double Memory Test: encoding specificity improves diagnostic sensitivity and specificity. Neurology 1997; 48:989-997Crossref, Medline, Google Scholar
48 Tulving E, Thompson DM: Encoding specificity and retrieval processes in episodic memory. Psychol Rev 1973; 80:352-373Crossref, Google Scholar
49 Diesfeldt HFA: The importance of encoding instructions and retrieval cues in the assessment of memory in senile dementia. Arch Gerontol Geriatr 1984; 3:51-57Crossref, Medline, Google Scholar
50 Martin A, Brouwers P, Cox C, et al: On the nature of the verbal memory deficit in Alzheimer's disease. Brain Lang 1985; 25:323-341Crossref, Medline, Google Scholar
51 Lipinska B, Bäckman L, Mantyla T, et al: Effectiveness of self-generated cues in early Alzheimer's disease. J Clin Exp Psychol 1994; 19:809-819Google Scholar
52 Lipinska B, Bäckman L: Encoding-retrieval interactions in mild Alzheimer's disease: the role of access to categorical information. Brain Cogn 1997; 34:274-286Crossref, Medline, Google Scholar
53 Arkin SM: Alzheimer memory training: students replicate learning success. Am J Alzheimers Dis 2000; 15:152-162Crossref, Google Scholar
54 Squires EJ, Hunkin NM, Parkin AJ: Memory notebook training in a case of severe amnesia: generalising from paired associate learning to real life. Neuropsychol Rehab 1996; 6:55-65Crossref, Medline, Google Scholar
55 Squires EJ, Hunkin NM, Parkin AJ: Errorless learning of novel association in amnesia. Neuropsychologia 1997; 35:1103-1111Crossref, Medline, Google Scholar
56 Wilson BA: Case Studies in Neuropsychological Rehabilitation. New York, Oxford University Press, 1999Google Scholar
57 Robertson IH: Cognitive rehabilitation in neurologic disease. Curr Opin Neurol 1993; 6:756-760Crossref, Medline, Google Scholar
58 Andrewes D, Gielewski E: The work rehabilitation of a herpes simplex encephalitis patient with retrograde amnesia. Neuropsychol Rehabil 1999; 9:77-99Crossref, Google Scholar
59 Kixmiller JS: Evaluation of prospective memory training for individuals with mild Alzheimer's disease. Brain Cogn 2002; 49:237-241Medline, Google Scholar
60 Landauer TK, Bjork RA: Optimal rehearsal patterns and name learning, in Practical Aspects of Memory. Edited by Gruneberg MM, Morris P, Sykes R. London, Academic Press, 1978, pp 625-632Google Scholar
61 Linton M: The maintenance of knowledge: some long-term specific and generic changes, in Practical Aspects of Memory. Edited by Gruneberg MM, Morris P, Sykes R. New York, Wiley, 1988, pp 378-384Google Scholar
62 Bjork RA: Retrieval practice and the maintenance of knowledge, in Practical Aspects of Memory, vol 2. Edited by Gruneberg MM, Morris R. London, Academic Press, 1988, pp 396-401Google Scholar
63 Wilson BA, Emslie HC, Quirk K, et al: Reducing everyday memory and planning problems by means of a paging system: a randomized control crossover study. J Neurol Neurosurg Psychiatry 2001; 70:477-482Crossref, Medline, Google Scholar
64 Camp CJ, McKitrick LA: Memory interventions in Alzheimer's-type dementia populations: methodological and theoritical issues, in Everyday Memory and Aging: Current Research and Methodology. Edited by West RL, Sinnott JD. New York, Springer-Verlag, 1992, pp 155-172Google Scholar
65 Hersh N, Treadgold L: NeuroPage: the rehabilitation of memory dysfunction by prosthetic memory and cueing. Neurorehabilitation 1994; 4:187-197Medline, Google Scholar
66 Bäckman L, Josephsson S, Herlitz A, et al: The generalizability of training gains in dementia: effects of an imagery-based mnemonic on face-name retention duration. Psychol Aging 1991; 6:489-492Crossref, Medline, Google Scholar
67 Davis RN, Massman PJ, Doody RS: Cognitive intervention in Alzheimer disease: a randomized placebo-controlled study. Alzheimer Dis Assoc Disord 2001; 15:1-9Crossref, Medline, Google Scholar
68 McKitrick LA, Camp CJ, Black FW: Prospective memory intervention in Alzheimer's disease. J Gerontol 1992; 47:337-343Crossref, Google Scholar
69 Kesslak JP, Nackoul K, Sandman CA: Memory training for individuals with Alzheimer's disease improves name recall. Behav Neurol 1997; 10:137-142Crossref, Medline, Google Scholar
70 Sandman C: Memory rehabilitation in Alzheimer's disease: preliminary findings. Clin Gerontol 1993; 13:19-33Crossref, Google Scholar
71 Clare L, Wilson BA, Breen K, et al: Errorless learning of face-name associations in early Alzheimer's disease. Neurocase 1999; 5:37-46Crossref, Google Scholar
72 Clare L, Wilson BA, Carter G, et al: Long-term maintenance of treatment gains following a cognitive rehabilitation intervention in early dementia of Alzheimer type: a single case study. Neuropsychol Rehab 2001; 11:477-494Crossref, Google Scholar
73 Wechsler D: Wechlser Memory Scale-Revised: Manual. San Antonio, TX, Psychological Corporation, 1987Google Scholar
74 Simard M, van Reekum R, Suvajac B: Improving cognition, behavior and function, and slowing disease progression of Alzheimer's disease: a review. Clin Geriatr 2000; 8:32-58Google Scholar
75 Alivisatos B, Petrides M: Functional activation of the human brain during mental rotation. Neuropsychologia 1997; 35:111-118Crossref, Medline, Google Scholar
76 Levine DN, Warach J, Farah M: Two visual systems in mental imagery: dissociation of “what” and “where” in imagery disorders due to bilateral posterior cerebral lesions. Neurology 1985; 35:1010-1018Crossref, Medline, Google Scholar
77 Farah MJ: The neurological basis of mental imagery: a componential analysis. Cognition 1984; 18:245-272Crossref, Medline, Google Scholar
78 Farah MJ: Is visual imagery really visual? Overlooked evidence from neuropsychology. Psychol Rev 1988; 95:307-317Crossref, Medline, Google Scholar
79 Bowers D, Blonder LX, Feinberg T, et al: Differential impact of right and left hemisphere lesions on facial emotion and object imagery. Brain 1991; 114:2593-2609Crossref, Medline, Google Scholar
80 Iyo M, Namba H, Fukushi K, et al: Measurement of acetylcholinesterase by positron emission tomography in the brains of healthy controls and patients with Alzheimer's disease. Lancet 1997; 349:1805-1809Crossref, Medline, Google Scholar
81 Haxby JV, Grady CL, Koss E, et al: Longitudinal study of cerebral metabolic asymmetries and associated neuropsychological patterns in early dementia of the Alzheimer type. Arch Neurol 1990; 47:753-760Crossref, Medline, Google Scholar
82 Wolfe N, Reed BR, Eberling JL, et al: Temporal lobe perfusion on single photon emission computed tomography predicts the rate of cognitive decline in Alzheimer's disease. Arch Neurol 1995; 52:257-262Crossref, Medline, Google Scholar
83 Montaldi D, Brooks DN, McColl JH, et al: Measurements of regional cerebral blood flow and cognitive performance in Alzheimer's disease. J Neurol Neurosurg Psychiatry 1990; 53:33-38Crossref, Medline, Google Scholar
84 Zanetti O, Zanieri G, Di Giovanni G, et al: Effectiveness of procedural memory stimulation in mild Alzheimer's disease patients: a controlled study. Neuropsychol Rehab 2001; 11:263-272Crossref, Google Scholar
85 Wilson BA: Cognitive rehabilitation: how it is and how it might be. J Int Neuropsychol Soc 1997; 3:487-496Crossref, Medline, Google Scholar