Tyrosine Supplements for ADHD Symptoms With Comorbid Phenylketonuria
To the Editor: Phenylketonuria is the most common genetic disorder of amino acid metabolism with an incidence of 1 per 15,000 births. It is caused by a mutation in the gene coding for phenylalanine hydroxylase resulting in an inability to metabolize phenylalanine to tyrosine—a precursor of dopamine and norepinephrine.
Treatment for phenylketonuria involves restricting protein intake. If a low protein diet is commenced at birth and maintained throughout development, many patients achieve normal cognitive functioning. Failure to maintain the diet, however, leads to elevated serum phenylalanine with subsequent cognitive decline and potential mental retardation. 1
As individuals with phenylketonuria are unable to metabolize phenylalanine to tyrosine, and tyrosine is an essential precursor to dopamine, some authors have suggested that tyrosine-enriched foods be included as part of the diet for patients with phenylketonuria. Several studies have investigated the use of tyrosine supplements to reverse the cognitive effects associated with hyperphenylalaninemia, but the results have been mixed. 2 To our knowledge, however, no studies have investigated the use of tyrosine supplements for psychiatric conditions comorbid with phenylketonuria. We present the case of a young boy with phenylketonuria and comorbid attention-deficit/hyperactivity disorder (ADHD) who was treated with tyrosine supplementation.
Given that tyrosine is an essential precursor to dopamine, we hypothesized that the patient’s ADHD symptoms may have been exacerbated by hypotyrosinemia. By supplementing his diet with tyrosine, we were able to achieve a reduction in his ADHD symptoms, and we suspect that the mechanism of action was an augmentation of dopaminergic activity.
Case Report
AA, a 4-year-old boy with phenylketonuria, was started at birth on a protein-restricted diet and was followed in a metabolic disease clinic. He was developing normally until age 3, when his parents noted behavioral problems characterized by impulsivity and poor frustration tolerance. At age 4, he was enrolled in an early intervention program and received psychosocial treatments to address worsening symptoms of inattention, hyperactivity, and aggression. After 4 months of treatment, AA showed little improvement. He underwent a comprehensive psychiatric evaluation, and a diagnosis of ADHD, Combined Type, was made. AA was started on a tyrosine supplement at a dose of 100 mg/kg/day. The treatment was well tolerated and after 4 weeks of treatment, he showed a dramatic improvement in his ADHD symptoms.
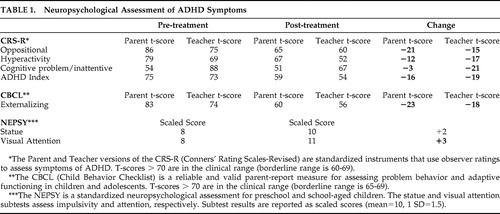
Standardized ratings are shown in Table 1 .
 |
Comment
Attention-deficit/hyperactivity disorder is a heterogeneous condition characterized by inattention, hyperactivity, and impulsivity. Although its precise pathophysiology is unknown, neuropsychological studies have found deficits in executive functions, including inhibitory control and set shifting. 3 Moreover, consistent with longstanding data that psychostimulants reduce the symptoms of ADHD, functional imaging studies have implicated abnormalities in the dopaminergic pathways of the anterior attentional system. 4
Our findings suggest that our patient’s symptoms of ADHD may have been exacerbated by a deficiency in tyrosine and suggest a potential approach for treating patients with comorbid phenylketonuria and ADHD. Moreover, our findings suggest that inquiring into dietary habits may be important when evaluating children with ADHD.
1. Wappner R, Cho S, Kronmal RA, et al: Management of phenylketonuria for optimal outcome: a review of guidelines for phenylketonuria management and a report of surveys of parents, patients, and clinic directors. Pediatrics 1999; 104:e68Google Scholar
2. Poustie VJ, Rutherford P: Tyrosine supplementation for phenylketonuria. Cochrane Database Syst Rev 2000; CD001507Google Scholar
3. Barkley RA: Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 1997; 121:65–94Google Scholar
4. Volkow ND, Wang GJ, Fowler JS, et al: Imaging the effects of methylphenidate on brain dopamine: new model on its therapeutic actions for attention-deficit/hyperactivity disorder. Biol Psychiatry 2005; 57:1410–145Google Scholar



