Psychopharmacological Neuroprotection in Neurodegenerative Disease: Heuristic Clinical Applications
This report is the second of a two-part series on psychopharmacological neuroprotection in neurodegenerative disease. Part I appeared in the Winter 2010 issue of The Journal of Neuropsychiatry and Clinical Neurosciences , available at http://neuro.psychiatryonline.org/.
Neuropsychiatric conditions abound in these neurodegenerative diseases, and psychotropic drugs are routinely applied in treating them. Aggression, agitation, anxiety, apathy, depression, disinhibition, and psychosis are among the many behavioral complications in neurodegenerative diseases, are highly prevalent, and add tremendously to patient distress and caregiver burden. 1 – 29 Psychotropics are often prescribed to control neuropsychiatric behavioral disturbances in these diseases. 2 , 3 , 8 , 9 , 11 – 16 , 18 , 19 , 23 , 29 – 38 Thus, it is fortuitous that drugs that provide clinical benefit in neurodegenerative diseases may also afford the neuroprotective capacity to deter the progression of underlying pathobiologies.
In Part I of this report, we reviewed preclinical effects of psychotropics on selected pathophysiological processes operant in neurodegenerative disease. Here, we review the broader diversity of neuroprotective actions and the potential effects of selected psychotropics representing pharmacological classes of drugs with promising neuroprotective potential. These psychotropics are selected to represent pharmacodynamic drug classes with multiple neuroprotective actions. We will overview these neuroprotective actions and provide some examples of the complexity of their interactions.
A Diversity of Neuroprotective Actions
A wide array of mechanisms provide potential opportunities for neuroprotective treatment in the neurodegenerative diseases. Briefly, the enzyme glycogen synthase kinase-3 (GSK-3) promotes alpha-synuclein (αSyn) expression, 39beta-amyloid (Aβ) production, 40 and tau phosphorylation. 39 , 41 The neurodegenerative diseases are linked to pathological protein accumulation, for example, αSyn, particularly in Parkinson’s disease, 42 Parkinson’s disease dementia, 43 and dementia with Lewy bodies, 43 and Aβ and hyperphosphorylated tau, especially in Alzheimer’s disease. 42 , 44 , 45 The newly emergent transactive response RNA/DNA binding protein TDP-43 affects RNA splicing 46 and is the dominant component of ubiquinated inclusions present in the TDP-43 proteinopathies, including frontotemporal lobar degeneration with ubiquitin immunoreactive inclusions (FTLD-U) and amyotrophic lateral sclerosis, 47 although psychotropic effects on TDP-43 remain to be discovered. It is these pathogenic protein inclusions that form the pathological stigmata of the neurodegenerative diseases, namely, Lewy bodies (αSyn) in Parkinson’s disease and amyloid plaques (Aβ) and neurofibrillary tangles (hyperphosphorylated tau) in Alzheimer’s disease.
Interestingly, treatments lowering plasma Aβ are thought to reduce the risk of developing Alzheimer’s disease, 48 – 50 and it is likely that modulation of plasma αSyn, Aβ, and tau concentrations can similarly lower the risk of developing other neurodegenerative diseases. Consistent with this concept, plasma αSyn oligomers are increased in Parkinson’s disease 51 , 52 and in multiple system atrophy. 52 Just as the plasma Aβ 42/40 forms ratio falls at the onset of Alzheimer’s disease, 53 , 54 plasma αSyn concentrations also appear to fall with the advent of Parkinson’s disease, 55 presumably attributable to deposition within the CNS. Consequently, reductions in plasma pathogenic proteins may, in the future, translate to reduced brain neuropathology in a number of neurodegenerative diseases.
Pathogenic proteins can lead to proteasomal56 – 58 and mitochondrial dysfunction , 59 , 60 increase intracellular calcium61 and free radicals , 62 and compromise axonal transport and cytoskeletal integrity , 63 leading to apoptosis .
The proteasome degrades damaged, toxic, excessive, and unwanted proteins from cells. 56 Undesirable proteins are tagged with a poly-ubiquitin chain by the E1-E3 ubiquitin conjugase-ligase system. 56 Poly-ubiquitylated proteins then enter the proteasome for degradation. The 26S proteasome consists of a 20S proteolytic core capped by 19S caps. 56 Unwanted proteins enter the caps, ubiquitin chains are cleaved, and the protein is unfolded and fed into the proteolytic core for cleavage into peptide fragments. It is interesting to note that the ubiquitinopathic frontotemporal dementia FTDU-17 is associated with tau-negative, ubiquitin-positive inclusions, and that mutant PARK 2 autosomal recessive juvenile Parkinson’s disease parkin has E3 ubiquitin ligase activity (part of the E1-E3 ubiquitin conjugase-ligase system). Oxidative stress impairs both ubiquitylation and proteasomal function, and proteasomal dysfunction engenders additional oxidative stress and free radical formation. 64 Proteasomal failure further leads to impaired degradation of pathogenic proteins, apoptotic mediators (e.g., caspases and bcl-2 proteins), 65 and regulators of apoptotic transcription factors (e.g., p53, NF-kappaB, HIF-1 alpha), 65 reduced axonal viability and synaptic integrity, 66 and mitochondrial dysfunction. 60
Mitochondrial dysfunction leads to the generation of reactive oxygen species and consequent mitochondrial depolarization and mitochondrial permeability transition pore development with the release of free radicals and cytochrome c into the cytoplasm, which in turn trigger the apoptotic cascade. 67 Mitochondrial respiratory dysfunction, including complex I 68 and complex II 69 , 70 deficiencies and the complex I inhibitors rotenone 71 and tumor necrotic factor, 72 each leads to apoptosis. Additionally, free radicals including reactive oxygen species and reactive nitrogen species result in lipid peroxidation that advances the course of neurodegenerative disease. 73 , 74 In Parkinson’s disease, free radicals are linked to dopaminergic neuronal loss. 75 Reactive species include peroxide radicals, especially linked to dopamine oxidation and superoxide dismutase, and nitric oxide, especially related to inducible nitric oxide synthase, constituting major mechanisms of interest in neurodegenerative diseases. 73 , 76 Nitric oxide promotes the generation of free radicals, 77 which in turn advance the progression of neurodegenerative diseases. 78
There are several apoptotic pathways that play key roles in neurodegenerative diseases, including mitochondrial-, death receptor-, and p53-mediated apoptotic pathways. 79 , 80 The mitochondrial pathway involves cytochrome c-related activation of caspase-9, which activates caspase-3 81 and the apoptotic cascade. 82 This mitochondrial apoptotic pathway plays a principal role in neurodegenerative diseases. 83 The death receptor, or Fas pathway, involves FADD and caspase-8 activation, whereas the p53 pathway involves glyceraldehyde-3-phosphate dehydrogenase and Bax, with caspase-8 and Bax initiating the apoptotic cascade. 79 , 80
In addition, glutamate excitotoxicity is a leading theory of neurodegeneration in Alzheimer’s disease, 84 Parkinson’s disease, 85 , 86 Huntington’s disease, 87 , 88 and amyotrophic lateral sclerosis 89 , 90 and is a basis for the potential neuroprotective effects of memantine 84 , 91 and riluzole. 92 Glutamate mediates apoptosis through mechanisms that include glutamatergic N -methyl-D-aspartate (NMDA) receptors, 93 , 94 calcium influx, 95 and free radicals. 93 , 95 , 96 Inhibition of GSK-3β protects against glutamate-induced, caspase-3-mediated apoptosis. 97
Inflammatory processes are also evident in the neurodegenerative diseases. Aβ neuritic plaques and proinflammatory cytokines in Alzheimer’s disease lead to microglial activation and inflammation . 98 Activated microglia, reactive astrogliosis, and lymphocytic infiltration are also apparent in the substantia nigra in Parkinson’s disease as a later concomitant of neurodegeneration, 99 , 100 possibly related to αSyn and oxidative stress. 64 , 100 Activated microglia then produce cytokines, reactive oxygen and nitrogen species, and eicosanoids that propagate further neurodegeneration. 101 It is interesting to note that sleep loss may promote inflammation. 102 Sleep loss is often present in neurodegenerative diseases, especially related to fragmentary daytime napping, depression, psychosis, or insomnia.
These neurodegenerative mechanisms occur in the absence of neurodegenerative diseases and are balanced by neuroregenerative processes, including neuritogenesis and the influence of neurotrophic factors. Cytoskeletal derangements occur in neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease related to changes in tau and tubulin, and there is evidence that certain drugs and hormones can affect this and stimulate neuritogenesis . 103 Neuritogenesis is key to neuronal and synaptic recovery and regeneration after injury and is a treatment target in neurodegenerative diseases. 104Neurotrophic factors include brain-derived neurotrophic factors (BDNF) and glial-derived neurotrophic factors (GDNF). BDNF 105 , 106 and GDNF 105 – 110 consitute important treatment targets in Alzheimer’s disease, 106 Parkinson’s disease, 106 , 108 – 110 Huntington’s disease, 105 amyotrophic lateral sclerosis, 107 and spinal muscular atrophy, 107 with GDNF showing more potential than BDNF in most models. 105 , 107 , 109 Persephin and other GDNFs have promoted neuronal survival and neuritogenesis in a midbrain dopamine neuron model of Parkinson’s disease. 111
Complex Interactions Between Neurodegenerative Mechanisms
The number of neuroprotective mechanisms is complex. The interaction of various mechanisms with each other is also complex. For example, proteasomal inhibition increases the accumulation of pathogenic proteins, impairs mitochondrial function, and triggers apoptosis. Further complexity of interaction is apparent in considering specific mechanisms, for example, pathogenic proteins.
It has been found that Aβ and tau each facilitate αSyn aggregation in Parkinson’s disease 112 – 114 and that αSyn is linked to Alzheimer’s disease 115 and facilitates tau aggregation in Alzheimer’s disease. 112 αSyn and tau each independently initiate amyloid formation. 116 Moreover, GSK-3 promotes Aβ formation by phosphorylating amyloid precursor protein 40 and also promotes tau hyperphosphorylation to pathogenic tau 41 in Alzheimer’s disease. In Parkinson’s disease, GSK-3 alleles are associated with Parkinson’s disease risk. 113 , 114 Furthermore, GSK-3β inhibitors may reduce αSyn 39 and αSyn upregulates GSK-3β, 117 suggesting that GSK-3β and αSyn mutually upregulate each other in Parkinson’s disease models. These pathological proteins interact at various levels in the pathological chain of events that involves protein processing at the proteasome, mitochondrial destabilization, free radical generation, apoptotic pathway activation, cell death, and neuroinflammation.
GSK-3, αSyn, tau, and Aβ each inhibit the proteasome, 56 impair mitochondrial function, 59 , 60 generate free radicals, 62 and result in apoptosis. 42 , 118 These processes are compounded by their induction of microglial activation 98 – 100 and neuroinflamation. 101 Mutual upregulation of αSyn and GSK-3β in Parkinson’s disease can lead to apoptosis by GSK-3β-induced bcl-2 downregulation, 117 and by synphilin-1 phosphorylation 119 that induces endoplasmic stress and proteasomal dysfunction 119 in Parkinson’s disease. Also, in Parkinson’s disease models, GSK-3 further provides pathways through which rotenone, 120 6-hydroxydopamine, 121 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), 120 , 122 and l -dopa 123 , 124 mediate apoptosis. Finally, apoptosis is also indirectly triggered by tau and Aβ 118 in both Alzheimer’s disease and Parkinson’s disease 42 by inhibiting proteasomal 56 and mitochondrial 60 function and inducing free radical damage, 62 microglial activation, 98 – 100 and inflammation. 101
These relationships of pathogenic proteins to specific neurodegenerative mechanisms are just one example of the complexity of interaction between various components of the neurodegenerative process. Thus, neuroprotective strategies that address individual neurodegenerative mechanisms can potentially enhance their neuroprotective effects through these complex interactions.
Neuroprotection Targets
It is apparent from the above discussion that a number of independent mechanisms produce neurodegeneration. Consequently, a wide variety of neuroprotective targets exist and these include GSK-3, glutamate, tau hyperphosphorylation and aggregation, Aβ production and aggregation, αSyn production and aggregation, other protein (e.g., TDP-43) production and aggregation, proteasomal function, free radical generation (reactive oxygen, nitrogen, and other species), oxidative stress, antioxidant enzymes, mitochondrial dysfunction (including complex I, complex II, other respiratory chain components, and ATP production), apoptosis, neuroinflammation, cytoskeletal integrity, trophic factors (e.g., BDNF, GDNF), and neuritogenesis.
Scope of the Present Report
The findings in Part I of this report indicate possible neuroprotective applications for psychotropics in neurodegenerative diseases. Here, we integrate those findings and consider some neuroprotective candidate agents that are used to treat neuropsychiatric disturbances in the clinical arena and, based on their pharmacological class membership, may have salutary effects at various levels of the neurodegenerative pathophysiological sequence. In Part I (Winter 2010 issue, available at http://neuro.psychiatryonline.org/), we considered candidate neuroprotective agents based upon research findings for first-line psychotropics in regard to only certain neuroprotective mechanisms. In contrast, here we consider the broader diversity of neuroprotective mechanisms for representative drugs that exert pharmacodynamic actions consistent with those of promising agents discussed in Part I. We further consider the wider spectrum of neuroprotective attributes for the selected psychotropics, building upon the findings in Part I of this report.
An important caveat to this synthesis is that the neuroprotective actions of these psychotropics may not necessarily be mediated by their established pharmacodynamic mechanisms. While there is early evidence that at least some of their actions are in fact mediated by these pharmacodynamic actions, this literature is in its infancy. Further, although representative drugs are put forth, supporting evidence is drawn from drugs within their pharmacological class possessing identical primary pharmacodynamic actions. Nevertheless, there are common neuroprotective effects within given psychotropic classes (see Part I of this report), and some of these have already been linked to specific pharmacodynamic mechanisms (e.g., serotonin, melatonin receptors, etc.).
The drugs considered here appear to have been neglected and subjected to little research thus far, as is evident in Part I of this report. They are selected based on evidence in Part I of this report supporting the neuroprotective potential of psychotropic drugs possessing their mechanisms of action. We consider representative drugs of pharmacological classes that have symptomatic utility in neurodegenerative diseases and should now be subjected to preclinical investigations according to the criteria in Table 1 . Based on these criteria, research using delayed-start (staggered start) and randomized-withdrawal designs 125 can be undertaken to determine their disease-modifying neuroprotective utility. Examples of wakefulness promoting, anxiolytic, antidepressant, antipsychotic, and hypnotic agents are provided.
 |
METHODS
The method is specified in Part I of this report but, briefly, it relied on the Part I search strategy extended by bibliographic review and other sources including literature searches of peer reviewed published articles for the drugs specified and for neuroprotective actions ranging beyond those focused on in Part I.
Modafinil
Modafinil is a drug with symptomatic potential in neurodegenerative diseases that binds to the dopamine transporter 126 – 128 and increases synaptic DA. 127 It may act as a direct dopamine D2 receptor agonist 129 and may secondarily stimulate noradrenergic activity. 130 – 132 Dopaminergic and noradrenergic deficits occur in Alzheimer’s disease and Parkinson’s disease, and these modafinil actions could improve daytime somnolence, sundowning, cognition, and neuropsychiatric disorders in dementia. Modafinil has effectively treated excessive daytime sleepiness in Parkinson’s disease 133 and amyotrophic lateral sclerosis. 134 Performance on the clock drawing task, which integrates executive, visuospatial, and other cognitive functions that are impaired in dementia and is commonly used to screen for dementia, improved in healthy middle-aged subjects given modafinil. 135 Modafinil has also been demonstrated to increase hippocampal glutamate release. 136 Glutamate is critical for proper memory function through the process of long-term potentiation. 137 , 138 Increasing glutamate release may lead to improved memory function in disorders where the hippocampus is degenerating. In various disorders, modafinil has improved executive function, 139 – 144 verbal fluency, 145 attention, 139 , 144 , 146 – 150 memory, 140 , 141 , 144 apathy, 151 , 152 fatigue, 153 depression, 154 – 157 and response inhibition. 139 – 141 , 144 Improvements in cognition and response inhibition may further improve impulsivity, disinhibition, and aggression. Moreover, modafinil has been suggested to potentially improve Parkinson’s disease symptoms related to enhanced glutamatergic striatal stimulation and reduced striatopallidal GABA release. 158
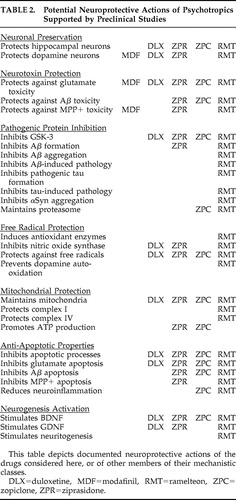
Modafinil appears to simultaneously enhance glutamatergic symptomatic function while blocking its neurotoxic effects, 159 consistent with a neuroprotective action potentially applicable in a number of neurodegenerative diseases, including Alzheimer’s disease, Huntington’s disease, and amyotrophic lateral sclerosis. Modafinil also dose-dependently 160 blocks MPTP neurotoxicity in the marmoset monkey Parkinson’s disease model 160 , 161 through antioxidant effects and the modulation of nigrostriatal monoamines. 162 This same effect has been observed in nigral neuronal and glial cells in black mice. 163 Thus, modafinil neuroprotective properties against glutamate toxicity and nigral degeneration may translate to clinical neuroprotection in patients with neurodegenerative diseases. The potential neuroprotective actions of modafinil are summarized in Table 2 .
 |
Duloxetine
The antidepressant duloxetine is a dual serotonin and norepinephrine reuptake inhibitor (SNRI). 164 Duloxetine has improved several measures of depression and cognition in a double-blind, placebo-controlled trial in geriatric patients. 165 Experience with selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibiting antidepressants, together with neurotransmitter correlate findings for certain neuropsychiatric disorders, suggests that duloxetine has the potential to improve depression, 165 – 175 anxiety, 15 , 16 , 166 , 172 , 176 hallucinations, 177 – 181 delusions, 177 , 181 , 182 sleep, 183 , 184 agitation, 166 , 181 , 182 , 185 , 186 aggression, 181 , 182 , 186 irritability, 166 , 176 , 181 , 182 , 186 , 187 disinhibition, 188 , 189 excitement, 176 , 182 wandering, 182 overall cognition, 165 , 190 – 193 attention, 194 – 196 executive functioning, 197 and memory 165 across neurodegenerative diseases. Apathy and urinary incontinence may also respond to duloxetine. Apathy and other dopamine-related symptoms can respond to duloxetine because norepinephrine reuptake inhibitors block frontal dopamine reuptake. 198 Indeed, apathy responds to agents that increase frontal dopamine. 199 , 200 Similarly, in Parkinson’s disease, neurotransmitter correlates and agents that affect neurotransmitters further evidence the potential for improvements in Parkinson’s disease visuospatial processing 201 as well as bradyphrenia, akinesia, postural instability, freezing, dyskinesia, and Parkinson’s disease stage. 202 – 206 Urinary incontinence in dementia usually results from either sphincteric or detrusor muscle dysfunctions. Duloxetine is thought to work centrally at Onuf’s nucleus in the sacral spinal cord to improve sphincter tone mediated through 5HT2 and alpha-1 receptor effects 207 during urine storage but not during voiding, thereby significantly improving stress urinary incontinence. 208 , 209 In addition, a recent placebo-controlled study in women with overactive bladders due to documented detrusor instability revealed improved detrusor stability with reduced episodes of incontinence and voiding. This presumably is related to raising the sensory threshold for triggering micturition mediated by the 5HT1a receptor at the primary afferent neurons in the superficial dorsal horn of the sacral spinal cord. 210
Duloxetine and agents with related modes of action together have demonstrated neuroprotective properties in neurodegenerative models relevant to neurodegenerative diseases, such as reducing pathogenic tau and Aβ, proteins that also facilitate and synergize αSyn pathogenic oligomeric fibrillation and promote proteinopathic inclusions in Alzheimer’s disease and Parkinson’s disease. Other properties include inhibition of GSK-3β (thereby reducing αS, tau, and Aβ formation) and reductions in free radical production, nitric oxide synthase activity, mitochondrial permeability transition pore development, apoptosis (especially 6-hydroxydopamine- and glutamate-induced apoptosis in Parkinson’s disease and Alzheimer’s disease models), microglial activation, and inflammation. These drugs also upregulate BDNF and GDNF. We will sequentially summarize the evidence for SSRIs, selective norepinephrine reuptake inhibitors (NERIs), and SNRIs.
SSRIs reduce Aβ and tau concentrations and inhibit GSK-3β and apoptosis, including in the hippocampal formation. The SSRI paroxetine preserved cognitive performance and reduced hippocampal Aβ and tau levels in transgenic mice. 211 Additionally, antidepressants have effects on GSK-3, affecting neuronal pathological protein concentrations. The SSRI fluoxetine 212 and the SNRI imipramine 213 have each inhibited GSK-3. SSRI-induced GSK-3β inhibition appears to be mediated by 5HT1a receptor stimulation, which inhibits GSK-3β through serine 9 phosphorylation. 214 SSRIs improve cell proliferation in several models and inhibit several types of apoptosis in a variety of cell lines. Fluoxetine improved contextual memory and cell proliferation in Aβ transgenic mice. 215 Fluoxetine, 216 – 220 clomipramine, 220 paroxetine, 218 and citalopram 218 have inhibited apoptosis in neoplastic models. Of particular relevance in Alzheimer’s disease, fluoxetine enhanced cell proliferation and prevented dentate gyrus apoptosis in a rat model. 221
Selective NERIs block free radical generation including intramitochondrial radicals, mitochondrial permeability transition pore development, and several types of apoptosis in various cell lines. The selective NERI desipramine 222 , 223 has inhibited HDAC inhibitor/perifosine-induced 224 and tumor necrotic factor a -induced 225 , 226 reactive oxygen species production, glutamate-induced mitochondrial permeability transition pore opening in Huntington’s disease transgenic mice, 227 and apoptosis in a wide variety of models. 224 – 226 , 228 – 234 These apoptotic models include glutamate in transgenic Huntington’s disease mice 227 and 6-OHDA in neuronal PC12 cells relevant to Parkinson’s disease. 235 , 236
SNRIs like duloxetine inhibit GSK-3β, nitric oxide synthase, mitochondrial permeability transition pore opening, and several types of apoptosis in various cell lines. Duloxetine inhibits nitric oxide synthase 237 and, hence, free radical generation. The SNRI nortriptyline blocked glutamate-induced mitochondrial permeability transition pore opening and apoptosis in a transgenic mouse Huntington’s disease model. 227 As noted above, glutamate is also key to Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis. Imipramine inhibited tumor necrotic factor a -induced apoptosis 238 and cisplatin-induced clustering of CD95 apoptotic death receptors. 239
All three types of antidepressants reduce microglial activation and the expression of interleukin-6 and nitric oxide, 240 and several antidepressants including duloxetine upregulate the neurotrophic factors BDNF and GDNF to produce ex vivo and in vivo neuroprotection. BDNF is reduced in the frontal 241 and temporal 242 cortex and hippocampus 242 in Alzheimer’s disease. Chronic administration of duloxetine upregulates BDNF mRNA in frontal cortical synaptosomes, providing the potential to maintain or improve frontal cognition. 241 , 243 In Parkinson’s disease, BDNF is colocalized with dopamine neurons in the substantia nigra where it can function neuroprotectively, and it may have a beneficial neuromodulatory action as well. 244 Plasma BDNF levels were significantly lower in depressed patients than in healthy control subjects and normalized after 1 month of antidepressant treatment. 245 The same phenomenon has been demonstrated for serum GDNF, 246 a target in most neurodegenerative diseases. Antidepressant-induced increases in GDNF have been shown to be neuroprotective in both ex vivo 247 and in vivo 248 models and are mediated through a monoamine-independent mechanism. 110 , 249 Each of these effects is particularly relevant to Parkinson’s disease pathogenesis 64 and has the potential to protect against neurodegeneration in Parkinson’s disease and other neurodegenerative diseases. In principle, duloxetine offers the potential to combine the symptomatic and neuroprotective properties of the different antidepressants into an effective neurodegenerative disease treatment. The potential neuroprotective actions of duloxetine are summarized in Table 2 .
Ziprasidone
Ziprasidone is an atypical antipsychotic with D2 antagonist, 5HT2 inverse agonist, and 5HT1a agonist properties, as well as SNRI activity. 250 , 251 Ziprasidone modes of action thereby confer antipsychotic, antidepressant, and anxiolytic properties translating to a broad therapeutic potential in neurodegenerative diseases.
Aside from antipsychotic effects on hallucinations and delusions, 252 other ziprasidone benefits include effects on agitated behavior, 253 – 256 anxiety, 257 depression, 250 , 251 , 258 , 259 sleep, 260 and cognition. 251 , 261 Although results from controlled studies in dementia are lacking, in three frail elderly patients with dementia, ziprasidone was effective in improving psychosis, agitation, depression, and cognition in each case. 262 Additionally, improvement in negative symptoms 263 , 264 and cognition 266 – 268 in schizophrenia trials suggests that apathy and cognition (particularly executive function, working memory, episodic memory, attention/vigilance, and psychomotor speed) may improve in patients with dementia. Moreover, MMSE scores 269 and working memory 270 are sensitive to serotonin availability. Furthermore, as referenced in the duloxetine section, the dual SNRI action of ziprasidone suggests specific additional nonantipsychotic-mediated therapeutic effects on a wide variety of symptoms. These include hallucinations, delusions, depression, anxiety, apathy, sleep, agitation, aggression, irritability, disinhibition, excitement, wandering, incontinence, overall cognition, attention, executive function, memory, and visuospatial function. In Parkinson’s disease, at doses low enough to invoke ziprasidone actions other than D2 blockade, it is possible that beneficial effects may be seen on bradyphrenia, motor symptoms including akinesia, postural instability, freezing, stage, disability, dyskinesia, and on-off syndrome. In contrast to most other atypical antipsychotics, early clinical evidence suggests minimal motor impairment in Parkinson’s disease with ziprasidone. 255 , 271
Ziprasidone and agents with related modes of action together demonstrate neuroprotective properties in neurodegenerative models, including inhibition of GSK-3β, pathogenic protein formation, and GSK-3β and Aβ pathogenic effects. These drugs have also improved mitochondrial energy production and energy preservation after injury and protected against mitochondrial depolarization, transition pore development, and cytochrome c release. Additionally, these agents have reduced free radical production and lipid peroxidation, particularly free radicals induced by Aβ, and inhibited apoptosis, especially that induced by glutamate, Aβ, MPP + , and the proteasome inhibitor MG132 (relevant to Huntington’s disease, amyotrophic lateral sclerosis, Alzheimer’s disease, Parkinson’s disease, and other neurodegenerative diseases). Finally, SNRI properties of ziprasidone further suggest the capacity to reduce GSK-3β, pathogenic protein concentrations, nitric oxide synthesis, other free radicals, mitochondrial depolarization, apoptosis, microglial activation, and neuroinflammation while upregulating BDNF and GDNF.
In considering the putative neuroprotective effects of ziprasidone, we will sequentially consider the neuroprotective effects associated with D2 antagonists, drugs with 5HT2 antagonist properties, and 5HT1a agonists (SNRI properties are described in the duloxetine section).
D2 antagonists inhibit Aβ formation, 272 Aβ-induced calcium imbalances, 273 and apoptosis induced by glutamate in Huntington’s disease transgenic mice, 227 MPP + in a Parkinson’s disease model, 274 , 275 and MG132 proteasome inhibition in PC12 cells. 276 These actions are mediated through antipsychotic effects on D2 receptors, 273 sigma receptors, 272 , 273 respiratory chain complex I and II inhibition, 276 and mitochondrial transition pore development. 274 , 275
Ziprasidone and other D2-5HT2 antagonist antipsychotics have inhibited GSK-3, 212 leading to reductions in Aβ, tau, αSyn, and mitochondrial dysfunction (see introduction). 5HT2 receptor stimulation regulates GSK-3β activity by reducing serine 9 phosphorylation, 214 indicating that 5HT2 antagonism can promote GSK-3β inhibition. D2-5HT2 antagonists have increased energy charge and redox reaction velocity, 277 increased ATP production, 278 and prevented ATP reductions after injury. 279 , 280 They also have reduced superoxide radicals, 281 protected against Aβ-induced reactive oxygen species, 282 and inhibited mitochondrial depolarization, 282 mitochondrial permeability transition pore development, 281 and cytochrome c release. 278 , 281 Ziprasidone has been shown to reduce lipid peroxidation. 283 Finally, D2-5HT2 antagonists exhibit antiapoptotic properties including calmodulin antagonism 284 and endonuclease inhibition 284 and have inhibited apoptotic events in a variety of models, 284 – 289 including Aβ-induced 282 , 290 and MPP + -induced 291 apoptosis in neuronal PC12 cells.
In light of its SNRI properties, ziprasidone may have the additional antiapoptotic property of monoamine oxidase B inhibition. 292 5HT1a agonists have also demonstrated antiapoptotic effects. 293 – 296 Moreover, 5HT1a receptor stimulation also inhibits GSK-3β through serine 9 phosphorylation. 214
The combined D2 and 5HT2 antagonist, 5HT1a agonist, and SNRI properties of ziprasidone suggest a wealth of potential neuroprotective actions for this agent. The potential neuroprotective actions of ziprasidone are summarized in Table 2 .
S-Zopiclone
S-zopiclone is a short half-life nonbenzodiazepine cyclopyrrolone GABA-A receptor subunit agonist with preference for omega-1 receptors. 297 Short half-life benzodiazepine receptor site-specific agonists such as s-zopiclone are considered first-line treatments for sleep disturbances in Alzheimer’s disease 298 , 299 and Parkinson’s disease. 16 Short half-life hypnotics have been found to be safe and effective without notable side effects in the elderly, 300 and zopiclone is particularly well tolerated 301 and effective. 302
S-zopiclone and zopiclone have each been demonstrated to improve anxiety, depression, and cognitive impairment in patients with insomnia. 303 S-zopiclone REM suppression 304 may also improve REM behavior disorder in synucleinopathic neurodegenerative diseases. Moreover, “sleep benefit” has been observed for Parkinson’s disease motor symptoms. 305 – 308 Similarly, sleep appears to replenish neurotransmitter availability in dementia, especially acetylcholine, 309 the depletion of which has been linked to behavioral 310 , 311 and cognitive 312 disturbances. Consistent with this concept, sleep disturbances are correlated with reduced function in Alzheimer’s disease and in nondemented elderly. 313 A number of neuropsychiatric features are sensitive to sleep, including cognitive and noncognitive conditions. Noncognitive neuropsychiatric conditions that are sensitive to sleep include depression, 305 anxiety, 314 perceptual distortions and hallucinations, 315 , 316 aggressive behavior, 317 and apathy. 318 Sleep-sensitive cognitive conditions include delirium, 319 cognitive impairment, 318 psychomotor impairment, 320 attention and vigilance, 321 – 325 working memory, 326 – 331 learning, 332 , 333 short-term recognition memory encoding, 334 semantic memory retrieval, 326 hippocampus-dependent declarative memory, 335 , 336 visual memory, 325 , 337 visual processing, 325 long-term memory, 338 frontal executive performance, 309 , 326 , 339 – 342 response inhibition, 343 reasoning, 344 and other higher cognitive functions. 345
Zopiclone and similar agents have improved insomnia and nocturnal wandering, 346 anxiety, 347 , 348 and agitation 298 , 349 – 353 arising within the context of dementia. These drugs have also been reported to improve aggression in brain disease, 354 , 355 psychosis, 356 – 358 depression, 359 , 360 and apathy in schizophrenia. 361 , 362 Thus, s-zopiclone has the potential to improve a wide range of neuropsychiatric, cognitive, and motor disturbances in patients with neurodegenerative diseases.
Although the effects of s-zopiclone on neurodegenerative disease pathophysiology are in the early stages of investigation, s-zopiclone and other drugs sharing properties of s-zopiclone seem to exhibit neuroprotective properties that include protection against pathogenic proteins, free radical-induced lipid peroxidation, mitochondrial transition pore development, cytochrome c release, and apoptosis. There is also evidence of neurorestorative effects on GSK-3β over-activity, proteasomal processing, hippocampal neuronal ATP production, neuroinflammation, and BDNF expression.
GABA-A agonists have been shown to protect against Aβ-induced neurotoxicity, 363 glutamate-induced free radical formation, 364 free radical-induced lipid peroxidation, 365 calcium-induced mitochondrial permeability transition pore development, 366 and ischemia-induced mitochondrial cytochrome c release. They also promote ATP recovery in ischemic hippocampal slices 367 and may protect against apoptosis induced by Aβ 363 and by glutamate in hippocampal neurons. 364 These antiapoptotic properties are in contrast to GABA-A agonists that bind to peripheral benzodiazepine (TSPO) receptors (e.g., diazepam) and promote apoptosis. Finally, sleep deprivation, often present in neurodegenerative diseases, has been associated with GSK-3β activation, 368 altered proteasomal processing, 369 oxidative damage, 370 impaired mitochondrial integrity and function, 371 neurodegenerative inflammation, 102 and decreased BDNF expression. 372 (While sleep deprivation increases BDNF in developing rats, 373 developing tissue and organisms are different from mature tissues and organisms.) Correction of the insomnia with treatment can potentially reverse these impairments. S-zopiclone and related drugs may therefore provide polymodal neuroprotection in these diseases. The potential neuroprotective actions of s-zopiclone are summarized in Table 2 .
Ramelteon
Ramelteon is a melatonin (MT) MT1 and MT2 receptor agonist 374 with demonstrated efficacy in elderly subjects with insomnia. 375 , 376 Ramelteon is more potent and has greater affinity at melatonin receptors than does melatonin itself. 374 As mentioned above (see s-zopiclone section, third paragraph), a large number of neuropsychiatric features are sensitive to sleep. Additionally, reduced melatonin excretion has been observed in beta-blocker hallucinosis, 377 a condition that resembles the hallucinations 378 and delirial features 379 of Parkinson’s disease and dementia with Lewy bodies. Consistent with these symptoms induced by beta-blockers, noradrenergic locus coeruleus degeneration is observed in Parkinson’s disease 380 and dementia with Lewy bodies, 381 suggesting a potential link between these symptoms and melatonin receptor activity.
Melatonin administration itself has improved sleep 382 , 383 and has demonstrated efficacy in neuropsychiatric disturbances in general, 383 including anxiety, 384 delirium, 385 , 386 disturbances of attention, 387 , 388 some aspects of memory, 384 , 389 daytime sleepiness and “sundowning behavior” in dementia, 386 and REM behavior disorder 390 that is commonly seen in dementia with Lewy bodies and Parkinson’s disease dementia. 15 , 16 Melatonin has also been suggested as a treatment for fluctuations in cognition and alertness in Parkinson’s disease. 391 The greater potency and affinity of ramelteon at melatonin receptors may lead to outcomes superior to those obtained with melatonin.
Melatonin has many neuroprotective actions in preclinical models, as exemplified in Parkinson’s disease and Alzheimer’s disease. As mentioned in the s-Zopiclone section, sleep deprivation promotes neurodegenerative disease through effects on GSK-3β, the proteasome, oxidative damage, mitochondrial impairment, and neuroinflammation. Besides improvement in these functions ascribable to alleviating insomnia in neurodegenerative disease, results of melatonin treatment studies suggest ramelteon may exert neuroprotective effects by preserving dopaminergic, 392 – 402 striatal, 396 , 399 , 403 – 406 and hippocampal 403 neurons. Other potential neuroprotective actions include inhibiting αSyn aggregation, 407 , 408 pathogenic tau formation and tau-induced pathogenesis, 282 , 409 – 419 and Aβ fiber formation, aggregation, and deposition 411 , 412 , 420 – 422 and preventing tau- and Aβ-induced αSyn oligomerization. 112 – 114 , 116 Moreover, ramelteon has the potential to inhibit nitric oxide synthase, 423 scavenge free radicals, 396 , 397 , 403 , 404 , 423 – 429 induce antioxidant enzymes, 423 , 430 prevent dopamine auto-oxidation, 431 – 434 maintain mitochondrial integrity, 425 , 435 – 438 and protect against losses of complex I 439 – 446 in Parkinson’s disease and complex IV. 440 , 442 – 447 Furthermore, ramelteon may be able to prevent apoptotic cascades, 395 , 397 , 399 – 402 , 404 – 407 , 424 , 428 , 430 , 448 – 456 particularly those induced by glutamate, 457 – 459 Aβ, 460 and MPP +406 , 454 , 456 , 461 apoptosis. It is particularly interesting to note that the protection afforded against glutamate-induced apoptosis appears to be mediated by activation of the MT1 receptor. 459 Finally, ramelteon may stimulate BDNF, 462 – 464 GDNF, 108 , 110 , 462 – 465 and neuritogenesis. 103 Each of these effects is particularly relevant to neurodegenerative disease pathogenesis (see introduction), and ramelteon may prove to clinically protect against neurodegeneration.
The evidence is far too extensive to review here (see Part I of this report, and Table 3 of the online data supplement to Part I of this report), but by way of examples in Parkinson’s disease, melatonin prevented αSyn aggregation after maneb 407 and rotenone exposure 408 in Parkinson’s disease models and has preserved dopaminergic tyrosine hydroxylase-positive nigral neurons bearing MT1 and MT2 receptors after 6-hydroxy-dopamine lesions in rats. 395 Melatonin has prevented nigrostriatal free radical damage in mice 403 and rats 396 treated with MPTP and has led to essentially full nigrostriatal recovery in rats treated with MPTP 397 and those treated with 6-hydroxydopamine. 404 Melatonin reduced auto-oxidative semiquinone formation and increased l -dopa bioavailability in rats treated with intrastriatal l -dopa. 433 A rat striatal 6-hydroxydopamine study indicated neuroprotection by melatonin manifest in reduced nigral neurodegeneration as evidenced by apomorphine-induced turning behavior. 405 Melatonin reduced nigrostriatal neuronal apoptosis in an MPTP mouse model. 406 BDNF is colocalized with dopamine neurons in the substantia nigra, where it may exert neuromodulatory and neuroprotective effects. 244 BDNF and GDNF correlate with MT1 receptor activity, 463 and melatonin increases both GDNF and BDNF and promotes the viability of MT1 and MT2 receptor-bearing neural stem cells derived from rat ventral midbrain. It also significantly increases tyrosine hydroxylase and its mRNA, 464 indicative of enhanced nigral dopaminergic neurotrophism that is highly relevant to Parkinson’s disease. Melatonin and dopamine exhibit similar gene expression and protein profiles. 452 , 453 Recently, ramelteon has been demonstrated to increase neuronal BDNF concentrations in cultured mouse cerebellar granule cells bearing MT1 and others bearing MT2 receptors. 466
Neither melatonin nor ramelteon has undergone clinical trials for its clinical and disease-modifying neuroprotective properties in neurodegenerative disease, and melatonin preclinical and ramelteon clinical findings remain to be confirmed in neurodegenerative disease patients. An important caveat regards the need to determine which of the above neuroprotective properties of melatonin are mediated through melatonin receptors and other mechanisms common to both melatonin and ramelteon. The potential neuroprotective actions of ramelteon are summarized in Table 2 .
Directions for Future Research
The potential neuroprotective actions for each agent have been specified above. In Table 1 (also discussed in Part I of this report), we have indicated candidate criteria for potential prediction of translational neuroprotection in clinical patients.
| 1. | We therefore suggest that each of these promising agents be evaluated in terms of the specific enumerated neuroprotective actions in accord with the criteria of Table 1 . Such inquiries can clarify the mechanisms of these drugs and may determine the likelihood of positive outcomes in randomized, double-blind, placebo-controlled delayed-start or randomized-withdrawal neuroprotective clinical trials. 125 Although ethical issues regarding withholding treatment have been raised in such trials, it cannot be known whether a given drug has neuroprotective efficacy until such trials are conducted. In evaluating antidepressants in patients with depression, these procedures might be modified by using an antidepressant with less robust neuroprotective properties to supplant the placebo, avoiding an ethical dilemma by providing equally efficacious treatment for the depression. | ||||
| 2. | Furthermore, given that these agents are widely used to treat clinical neuropsychiatric conditions that arise in the context of neurodegenerative disease, and given that their safety and tolerability are known, neuroprotective clinical trials need not necessarily await the fulfillment of the Table 1 criteria. Nevertheless, caution is advised in light of adverse events recently identified for psychotropic drugs (e.g., increased death and stroke risks with antipsychotics) in elderly populations, the population most at risk for the most common neurodegenerative diseases. | ||||
| 3. | Research should be continued into the correlation of psychotropic pharmacodynamic mechanisms with neuroprotective actions. | ||||
| 4. | Finally, research to determine the clinical neuroprotective predictive utility of each of the Table 1 criteria can greatly assist the efforts of propelling agents of interest from preclinical studies to the clinical trial stage. | ||||
CONCLUSION
The above examples suggest that psychotropics may have neuroprotective potential. These neuroprotective properties based on preclinical studies are summarized in Table 2 .
It should be remembered that the properties of the drugs discussed above do not necessarily emanate from research data on the drugs themselves, but from agents representative of their class with similar pharmacodynamic properties. Whether the pharmacodynamic properties that are relevant to their psychotropic effects pertain to their neuroprotective actions is a subject of ongoing research, but there is preliminary evidence justifying this assumption for at least some of the effects of each drug mentioned.
These agents act at multiple levels of pathophysiological processes operant across the spectrum of neurodegenerative diseases. Although it is possible that strategic combinations of these agents may afford neuroprotective benefit superior to monotherapy in clinical trials, at the present time, selection of agents should be determined by their clinical symptomatic effects because they have not yet been comprehensively and systematically investigated in neurodegenerative disease models. Moreover, some of the drugs have been subjected to less comprehensive preclinical investigations than others, with neuroprotective features of some drugs being investigated only recently. The preliminary status of this neuroprotective research notwithstanding, a future strategy that may be useful is to use several drugs that each target the primary neurodegenerative processes in a selected disease of interest. Ziprasidone is a single drug that represents such an approach, combining the actions of D2-5HT2 antagonists, SNRIs, and 5HT1a agonists. Still, it seems more plausible that effective disease management will require identifying several drugs with complementary benefits. Consistent with this combination strategy, the combination of memantine with a cholinesterase inhibitor, cognitive enhancers with neuroprotective effects in preclinical models, yields progressively greater improvement in potential neuroprotective outcomes when coadministered than when a cholinesterase inhibitor is administered individually. 467 On the other hand, some combination therapies have actually abolished efficacy while multiplying toxicity, 468 and animal trials should first be conducted to evaluate this. In any event, it is important that these psychotropic drugs now be studied systematically in neurodegenerative disease preclinical models and that they be investigated for clinical neuroprotective efficacy in patients with those diseases.
1. Aarsland D, Sharp S, Ballard C: Psychiatric and behavioral symptoms in Alzheimer’s disease and other dementias: etiology and management. Curr Neurol Neurosci Rep 2005; 5:345–354Google Scholar
2. Anderson KE, Marshall FJ: Behavioral symptoms associated with Huntington’s disease. Adv Neurol 2005; 96:197–208Google Scholar
3. Aupperle P: Management of aggression, agitation, and psychosis in dementia: focus on atypical antipsychotics. Am J Alzheimers Dis Other Demen 2006; 21:101–108Google Scholar
4. Boyle PA, Malloy PF: Treating apathy in Alzheimer’s disease. Dement Geriatr Cogn Disord 2004; 17:91–99Google Scholar
5. Brodaty H, Draper B, Saab D, et al: Psychosis, depression and behavioral disturbances in Sydney nursing home residents: prevalence and predictors. Int J Geriatr Psychiatry 2001; 16:504–512Google Scholar
6. Brodaty H, Low LF: Aggression in the elderly. J Clin Psychiatry 2003; 64(suppl 4):36–43Google Scholar
7. Burgut FT, Benaur M, Hencliffe C: Late-life depression: a neuropsychiatric approach. Expert Rev Neurother 2006; 6:65–72Google Scholar
8. Buhr GT, White HK: Difficult behaviors in long-term care patients with dementia. J Am Med Dir Assoc 2007; 8(suppl 2):e101–113Google Scholar
9. Burns A, De Deyn PP: Risperidone for the treatment of neuropsychiatric features in dementia. Drugs Aging 2006; 23:887–896Google Scholar
10. Fischer C, Bozanovic-Sosic R, Norris M: Review of delusions in dementia. Am J Alzheimers Dis Other Demen 2004; 19:19–23Google Scholar
11. Fischer C, Bozanovic R, Atkins JH, et al: Treatment of delusions in Alzheimer’s disease: response to pharmacotherapy. Dement Geriatr Cogn Disord 2006; 22:260–266Google Scholar
12. Fischer C, Bozanovic R, Atkins JH, et al: Treatment of delusions in dementia with Lewy bodies: response to pharmacotherapy. Dement Geriatr Cogn Disord 2007; 23:307–311Google Scholar
13. Kozman MN, Wattis J, Curran S: Pharmacological management of behavioral and psychological disturbance in dementia. Hum Psychopharmacol 2006; 21:1–12Google Scholar
14. Kurt A, Nijboer F, Matuz T, et al: Depression and anxiety in individuals with amyotrophic lateral sclerosis: epidemiology and management. CNS Drugs 2007; 21:279–291Google Scholar
15. Lauterbach EC: The neuropsychiatry of Parkinson’s disease and related disorders. Psychiatr Clin North Am 2004; 27:801–825Google Scholar
16. Lauterbach EC: The neuropsychiatry of Parkinson’s disease. Minerva Medica 2005; 96:155–173Google Scholar
17. Lee HB, Lyketsos CG: Depression in Alzheimer’s disease: heterogeneity and related issues. Biol Psychiatry 2003; 54:353–362Google Scholar
18. Lesser JM, Hughes S: Psychosis-related disturbances: psychosis, agitation, and disinhibition in Alzheimer’s disease: definitions and treatment options. Geriatrics 2006; 61:14–20Google Scholar
19. Lyketsos CG, Lee HB: Diagnosis and treatment of depression in Alzheimer’s disease: a practical update for the clinician. Dement Geriatr Cogn Disord 2004; 17:55–64Google Scholar
20. McKeith I, Cummings J: Behavioral changes and psychological symptoms in dementia disorders. Lancet Neurol 2005; 4:735–742Google Scholar
21. Mendez MF, Lauterbach EC, Sampson SM, ANPA Committee on Research: An evidence-based review of the psychopathology of frontotemporal dementia: a report of the ANPA Committee on Research. J Neuropsychiatry Clin Neurosci 2008; 20:130–149Google Scholar
22. Mizrahi R, Starkstein SE: Epidemiology and management of apathy in patients with Alzheimer’s disease. Drugs Aging 2007; 24:547–554Google Scholar
23. Overshott R, Byrne J, Burns A: Nonpharmacological and pharmacological interventions for symptoms in Alzheimer’s disease. Expert Rev Neurother 2004; 4:809–821Google Scholar
24. Pace-Savitsky CE, Johnson JK, Miller BL: Behavioral changes in frontotemporal dementia with parkinsonism. Adv Neurol 2005; 96:187–196Google Scholar
25. Potter GG, Steffens DC: Contribution of depression to cognitive impairment and dementia in older adults. Neurologist 2007; 13:105–117Google Scholar
26. Pulsford D, Duxbury J: Aggressive behavior by people with dementia in residential care settings: a review. J Psychiatr Ment Health Nurs 2006; 13:611–618Google Scholar
27. Ropacki SA, Jeste DV: Epidemiology of and risk factors for psychosis of Alzheimer’s disease: a review of 55 studies published from 1990 to 2003. Am J Psychiatry 2005; 162:2022–2030Google Scholar
28. Rosenblatt A: Neuropsychiatry of Huntington’s disease. Dialogues Clin Neurosci 2007; 9:191–197Google Scholar
29. Starkstein SE, Mizrahi R: Depression in Alzheimer’s disease. Expert Rev Neurother 2006; 6:887–895Google Scholar
30. Alexopoulos GS, Jeste DV, Chung H, et al: Treatment of Dementia and Its Behavioral Disturbances. Minneapolis, McGraw-Hill, 2005Google Scholar
31. Ballard C, Howard R: Neuroleptic drugs in dementia: benefits and harm. Nat Rev Neurosci 2006; 7:492–500Google Scholar
32. Caine ED: Clinical perspectives on atypical antipsychotics for treatment of agitation. J Clin Psychiatry 2006; 67(suppl 10):22–31Google Scholar
33. Herrmann N, Lanctot KL: Pharmacologic management of neuropsychiatric symptoms of Alzheimer disease. Can J Psychiatry 2007; 52:630–646Google Scholar
34. Lee PE, Gill SS, Freedman M, et al: Atypical antipsychotic drugs in the treatment of behavioural and psychological symptoms of dementia: systematic review. BMJ 2004; 329:75Google Scholar
35. Madhusoodanan S, Shah P, Brenner R, et al: Pharmacological treatment of the psychosis of Alzheimer’s disease: what is the best approach? CNS Drugs 2007; 21:101–115Google Scholar
36. Moretti R, Torre P, Antonello RM, et al: Atypical neuroleptics as a treatment of agitation and anxiety in Alzheimer’s disease: risks or benefits. Expert Rev Neurother 2006; 6:705–710Google Scholar
37. Rummans TA, Lauterbach EC, Coffey CE, et al: Pharmacologic efficacy in neuropsychiatry: a review of placebo-controlled treatment trials. A report of the ANPA Committee on Research. J Neuropsychiatry Clin Neurosci 1999; 11:176–189Google Scholar
38. Wang PS, Brookhart MA, Setoguchi S, et al: Psychotropic medication use for behavioral symptoms of dementia. Curr Neurol Neurosci Rep 2006; 6:490–495Google Scholar
39. Kozikowski AP, Gaisina IN, Petukhov PA, et al: Highly potent and specific GSK-3beta inhibitors that block tau phosphorylation and decrease alpha-synuclein protein expression in a cellular model of Parkinson’s disease. ChemMedChem 2006; 1:256–266Google Scholar
40. Rockenstein E, Torrance M, Adame A, et al: Neuroprotective effects of regulators of the glycogen synthase kinase-3beta signaling pathway in a transgenic model of Alzheimer’s disease are associated with reduced amyloid precursor protein phosphorylation. J Neurosci 2007; 27:1981–1991Google Scholar
41. Brion JP, Anderton BH, Authelet M, et al: Neurofibrillary tangles and tau phosphorylation. Biochem Soc Symp 2001; 67:81–88Google Scholar
42. Nussbaum RL, Ellis CE: Alzheimer’s disease and Parkinson’s disease. N Engl J Med 2003; 348:1356–1364Google Scholar
43. Ballard C, Ziabreva I, Perry R, et al: Differences in neuropathologic characteristics across the Lewy body dementia spectrum. Neurology 2006; 67:1931–1934Google Scholar
44. Selkoe DJ, Schenk D: Alzheimer’s disease: molecular understanding predicts amyloid-based therapeutics. Annu Rev Pharmacol Toxicol 2003; 43:545–584Google Scholar
45. Cummings JL: Alzheimer’s disease. N Engl J Med 2004; 351:56–67Google Scholar
46. Buratti E, Baralle FE: Multiple roles of TDP-43 in gene expression, splicing regulation, and human disease. Front Biosci 2008; 13:867–878Google Scholar
47. Liscic RM, Grinberg LT, Zidar J, et al: ALS and FTLD: two faces of TDP-43 proteinopathy. Eur J Neurol 2008; 15:772–780Google Scholar
48. Kulstad JJ, Green PS, Cook DG, et al: Differential modulation of plasma beta-amyloid by insulin in patients with Alzheimer disease. Neurology 2006; 66:1506–1510Google Scholar
49. Flicker L, Martins RN, Thomas J, et al: B-vitamins reduce plasma levels of beta amyloid. Neurobiol Aging 2008; 29:303–305Google Scholar
50. Gurol ME, Irizarry MC, Smith EE, et al: Plasma beta-amyloid and white matter lesions in AD, MCI, and cerebral amyloid angiopathy. Neurology 2006; 66:23–29Google Scholar
51. El-Agnaf OM, Salem SA, Paleologou KE, et al: Detection of oligomeric forms of alpha-synuclein protein in human plasma as a potential biomarker for Parkinson’s disease. FASEB J 2006; 20:419–425Google Scholar
52. Lee PH, Lee G, Park HJ, et al: The plasma alpha-synuclein levels in patients with Parkinson’s disease and multiple system atrophy. J Neural Transm 2006; 113:1435–1439Google Scholar
53. Pesaresi M, Lovati C, Bertora P, et al: Plasma levels of beta-amyloid (1–42) in Alzheimer’s disease and mild cognitive impairment. Neurobiol Aging 2006; 27:904–905Google Scholar
54. Graff-Radford NR, Crook JE, Lucas J, et al: Association of low plasma abeta42/Abeta40 ratios with increased imminent risk for mild cognitive impairment and Alzheimer disease. Arch Neurol 2007; 64:354–362Google Scholar
55. Li QX, Mok SS, Laughton KM, et al: Plasma alpha-synuclein is decreased in subjects with Parkinson’s disease. Exp Neurol 2007; 204:583–588Google Scholar
56. Layfield R, Cavey JR, Lowe J: Role of ubiquitin-mediated proteolysis in the pathogenesis of neurodegenerative disorders. Ageing Res Rev 2003; 2:343–356Google Scholar
57. Lopez Salon M, Pasquini L, Besio MM, et al: Relationship between beta-amyloid degradation and the 26S proteasome in neural cells. Exp Neurol 2003; 180:131–143Google Scholar
58. Almeida CG, Takahashi RH, Gouras GK: Beta-amyloid accumulation impairs multivesicular body sorting by inhibiting the ubiquitin-proteasome system. J Neurosci 2006; 26:4277–4288Google Scholar
59. Hoshi M, Takashima A, Noguchi K, et al: Regulation of mitochondrial pyruvate dehydrogenase activity by tau protein kinase I/glycogen synthase kinase 3beta in brain. Proc Natl Acad Sci U S A 1996; 93:2719–2723Google Scholar
60. Feany MB: New genetic insights into Parkinson’s disease. N Engl J Med 2004; 351:1937–1940Google Scholar
61. Hölscher C: Development of beta-amyloid-induced neurodegeneration in Alzheimer’s disease and novel neuroprotective strategies. Rev Neurosci 2005; 16:181–212Google Scholar
62. Migliore L, Fontana I, Colognato R, et al: Searching for the role and the most suitable biomarkers of oxidative stress in Alzheimer’s disease and in other neurodegenerative diseases. Neurobiol Aging 2005; 26:567–573Google Scholar
63. Michaelis ML: Ongoing in vivo studies with cytoskeletal drugs in tau transgenic mice. Curr Alzheimer Res 2006; 3:215–219Google Scholar
64. Jenner P: Oxidative stress in Parkinson’s disease. Ann Neurol 2003; 53(suppl 3):S26–S36Google Scholar
65. Thompson SJ, Loftus LT, Ashley MD, et al: Ubiquitin-proteasome system as a modulator of cell fate. Curr Opin Pharmacol 2008; 8:90–95Google Scholar
66. Coleman MP, Ribchester RR: Programmed axon death, synaptic dysfunction and the ubiquitin proteasome system. Curr Drug Targets CNS Neurol Disord 2004; 3:227–238Google Scholar
67. Orrenius S, Gogvadze V, Zhivotovsky B: Mitochondrial oxidative stress: implications for cell death. Annu Rev Pharmacol Toxicol 2007; 47:143–183Google Scholar
68. Perier C, Tieu K, Guégan C, et al: Complex I deficiency primes Bax-dependent neuronal apoptosis through mitochondrial oxidative damage. Proc Natl Acad Sci U S A 2005; 102:19126–19131Google Scholar
69. Senoo-Matsuda N, Hartman PS, Akatsuka A, et al: A complex II defect affects mitochondrial structure, leading to ced-3- and ced-4-dependent apoptosis and aging. J Biol Chem 2003; 278:22031–22036Google Scholar
70. Ishii T, Yasuda K, Akatsuka A, et al: A mutation in the SDHC gene of complex II increases oxidative stress, resulting in apoptosis and tumorigenesis. Cancer Res 2005; 65:203–209Google Scholar
71. Li N, Ragheb K, Lawler G, et al: Mitochondrial complex I inhibitor rotenone induces apoptosis through enhancing mitochondrial reactive oxygen species production. J Biol Chem 2003; 278:8516–8525Google Scholar
72. Higuchi M, Proske RJ, Yeh ET: Inhibition of mitochondrial respiratory chain complex I by TNF results in cytochrome c release, membrane permeability transition, and apoptosis. Oncogene 1998; 17:2515–2524Google Scholar
73. Rotilio G, Aquilano K, Ciriolo MR: Interplay of Cu,Zn superoxide dismutase and nitric oxide synthase in neurodegenerative processes. IUBMB Life 2003; 55:629–634Google Scholar
74. Agil A, Duran R, Barrero F, et al: Plasma lipid peroxidation in sporadic Parkinson’s disease: role of the l -dopa. J Neurol Sci 2006; 240:31–36 Google Scholar
75. Okuno T, Nakatsuji Y, Kumanogoh A, et al: Loss of dopaminergic neurons by the induction of inducible nitric oxide synthase and cyclooxygenase-2 via CD 40: relevance to Parkinson’s disease. J Neurosci Res 2005; 81:874–882Google Scholar
76. Pannu R, Singh I: Pharmacological strategies for the regulation of inducible nitric oxide synthase: neurodegenerative versus neuroprotective mechanisms. Neurochem Int 2006; 49:170–182Google Scholar
77. Clark CB, Zhang Y, Martin SM, et al: The nitric oxide synthase inhibitor N(G)-nitro-L-arginine decreases defibrillation-induced free radical generation. Resuscitation 2004; 60:351–357Google Scholar
78. Gomez-Vargas M, Nishibayashi-Asanuma S, Asanuma M, et al: Pergolide scavenges both hydroxyl and nitric oxide free radicals in vitro and inhibits lipid peroxidation in different regions of the rat brain. Brain Res 1998; 790:202–208Google Scholar
79. Tatton WG, Chalmers-Redman R, Brown D, et al: Apoptosis in Parkinson’s disease: signals for neuronal degradation. Ann Neurol 2003; 53(suppl 3):S61–S70Google Scholar
80. Charriaut-Marlangue C: Apoptosis: a target for neuroprotection. Therapie 2004; 59:185–190Google Scholar
81. Lemasters JJ, Qian T, Trost LC, et al: Confocal microscopy of the mitochondrial permeability transition in necrotic and apoptotic cell death. Biochem Soc Symp 1999; 66:205–222Google Scholar
82. Zhang JH, Xu M: DNA fragmentation in apoptosis. Cell Res 2000; 10:205–211Google Scholar
83. Krieger C, Duchen MR: Mitochondria, Ca2+ and neurodegenerative disease. Eur J Pharmacol 2002; 447:177–188Google Scholar
84. Hynd MR, Scott HL, Dodd PR: Glutamate-mediated excitotoxicity and neurodegeneration in Alzheimer’s disease. Neurochem Int 2004; 45:583–595Google Scholar
85. Oh JD, Chase TN: Glutamate-mediated striatal dysregulation and the pathogenesis of motor response complications in Parkinson’s disease. Amino Acids 2002; 23:133–139Google Scholar
86. Marino MJ, Valenti O, Conn PJ: Glutamate receptors and Parkinson’s disease: opportunities for intervention. Drugs Aging 2003; 20:377–397Google Scholar
87. Arzberger T, Krampfl K, Leimgruber S, et al: Changes of NMDA receptor subunit (NR1, NR2B) and glutamate transporter (GLT1) mRNA expression in Huntington’s disease: an in situ hybridization study. J Neuropathol Exp Neurol 1997; 56:440–454Google Scholar
88. Wu J, Tang T, Bezprozvanny I: Evaluation of clinically relevant glutamate pathway inhibitors in in vitro model of Huntington’s disease. Neurosci Lett 2006; 407:219–223Google Scholar
89. Ludolph AC, Meyer T, Riepe MW, et al: Amyotrophic lateral sclerosis and glutamate. Restor Neurol Neurosci 1998; 13:59–67Google Scholar
90. Iwasaki Y, Ikeda K, Kinoshita M: Molecular and cellular mechanism of glutamate receptors in relation to amyotrophic lateral sclerosis. Curr Drug Targets CNS Neurol Disord 2002; 1:511–518Google Scholar
91. Molinuevo JL, Llado A, Rami L: Memantine: targeting glutamate excitotoxicity in Alzheimer’s disease and other dementias. Am J Alzheimers Dis Other Demen 2005; 20:77–85Google Scholar
92. Lamanauskas N, Nistri A: Riluzole blocks persistent Na+ and Ca2+ currents and modulates release of glutamate via presynaptic NMDA receptors on neonatal rat hypoglossal motoneurons in vitro. Eur J Neurosci 2008; 27:2501–2514Google Scholar
93. Nucci C, Piccirilli S, Bagetta G, et al: N-methyl-D-aspartate (NMDA) and non-NMDA glutamate receptor antagonists protect from apoptosis induced in the lateral geniculate nucleus of rabbits exposed to the dark. Neurosci Lett 1997; 229:185–188Google Scholar
94. Mailly F, Marin P, Israël M, et al: Increase in external glutamate and NMDA receptor activation contribute to H2O2-induced neuronal apoptosis. J Neurochem 1999; 73:1181–1188Google Scholar
95. Lu WY, Jackson MF, Bai D, et al: In CA1 pyramidal neurons of the hippocampus protein kinase C regulates calcium-dependent inactivation of NMDA receptors. J Neurosci 2000; 20:4452–4461Google Scholar
96. Nikolova S, Lee YS, Lee YS, et al: Rac1-NADPH oxidase-regulated generation of reactive oxygen species mediates glutamate-induced apoptosis in SH-SY5Y human neuroblastoma cells. Free Radic Res 2005; 39:1295–1304Google Scholar
97. Nishimoto T, Kihara T, Akaike A, et al: Alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionate attenuates glutamate-induced caspase-3 cleavage via regulation of glycogen synthase kinase 3beta. J Neurosci Res 2008; 86:1096–1105Google Scholar
98. Benveniste EN, Nguyen VT, O’Keefe GM: Immunological aspects of microglia: relevance to Alzheimer’s disease. Neurochem Int 2001; 39:381–391Google Scholar
99. Hirsch EC, Hunot S, Hartmann A: Neuroinflammatory processes in Parkinson’s disease. Parkinsonism Relat Disord 2005; 11(suppl 1):S9–S15Google Scholar
100. Wersinger C, Sidhu A: An inflammatory pathomechanism for Parkinson’s disease? Curr Med Chem 2006; 13:591–602Google Scholar
101. Liu Y, Qin L, Li G, et al: Dextromethorphan protects dopaminergic neurons against inflammation-mediated degeneration through inhibition of microglial activation. J Pharmacol Exp Ther 2003; 305:212–218Google Scholar
102. Cirelli C, Faraguna U, Tononi G: Changes in brain gene expression after long-term sleep deprivation. J Neurochem 2006; 98:1632–1645Google Scholar
103. Benitez-King G, Ramírez-Rodríguez G, Ortíz L, et al: The neuronal cytoskeleton as a potential therapeutical target in neurodegenerative diseases and schizophrenia. Curr Drug Targets CNS Neurol Disord 2004; 3:515–533Google Scholar
104. Grundman M, Capparelli E, Kim HT, et al: A multicenter, randomized, placebo controlled, multiple-dose, safety and pharmacokinetic study of AIT-082 (Neotrofin) in mild Alzheimer’s disease patients. Life Sci 2003; 73:539–553Google Scholar
105. Kells AP, Fong DM, Dragunow M, et al: AAV-mediated gene delivery of BDNF or GDNF is neuroprotective in a model of Huntington’s disease. Mol Ther 2004; 9:682–688Google Scholar
106. Weinreb O, Amit T, Bar-Am O, et al: Induction of neurotrophic factors GDNF and BDNF associated with the mechanism of neurorescue action of rasagiline and ladostigil: new insights and implications for therapy. Ann N Y Acad Sci 2007; 1122:155–168Google Scholar
107. Zurn AD, Winkel L, Menoud A, et al: Combined effects of GDNF, BDNF, and CNTF on motoneuron differentiation in vitro. J Neurosci Res 1996; 44:133–141Google Scholar
108. Ray DE: CINP 2000: Collegium Internationale Neuro Psychopharmacologicum 22nd Congress. IDrugs 2000; 3:1023–1025Google Scholar
109. Sun M, Kong L, Wang X, et al: Comparison of the capability of GDNF, BDNF, or both, to protect nigrostriatal neurons in a rat model of Parkinson’s disease. Brain Res 2005; 1052:119–129Google Scholar
110. Hisaoka K, Takebayashi M: [Glia as targets for antidepressants: an involvement in glial cell line-derived neurotrophic factor.] Nihon Shinkei Seishin Yakurigaku Zasshi 2007; 27:173–179 (Japanese)Google Scholar
111. Akerud P, Holm PC, Castelo-Branco G, et al: Persephin-overexpressing neural stem cells regulate the function of nigral dopaminergic neurons and prevent their degeneration in a model of Parkinson’s disease. Mol Cell Neurosci 2002; 21:205–222Google Scholar
112. Giasson BI, Forman MS, Higuchi M, et al: Initiation and synergistic fibrillization of tau and alpha-synuclein. Science 2003; 300:636–640Google Scholar
113. Kwok JB, Hallupp M, Loy CT, et al: GSK3B polymorphisms alter transcription and splicing in Parkinson’s disease. Ann Neurol 2005; 58:829–839Google Scholar
114. Goris A, Williams-Gray CH, Clark GR, et al: Tau and alpha-synuclein in susceptibility to, and dementia in, Parkinson’s disease. Ann Neurol 2007; 62:145–153Google Scholar
115. Sahin HA, Emre M, Ziabreva I, et al: The distribution pattern of pathology and cholinergic deficits in amygdaloid complex in Alzheimer’s disease and dementia with Lewy bodies. Acta Neuropathol (Berl) 2006; 111:115–125Google Scholar
116. Giasson BI, Lee VM, Trojanowski JQ: Interactions of amyloidogenic proteins. Neuromolecular Med 2003; 4:49–58Google Scholar
117. Yuan Y, Jin J, Yang B, et al: Overexpressed alpha-synuclein regulated the nuclear factor-kappaB signal pathway. Cell Mol Neurobiol 2008; 28:21–33Google Scholar
118. Ekshyyan O, Aw TY: Apoptosis: a key in neurodegenerative disorders. Curr Neurovasc Res 2004; 1:355–371Google Scholar
119. Avraham E, Szargel R, Eyal A, et al: Glycogen synthase kinase 3beta modulates synphilin-1 ubiquitylation and cellular inclusion formation by SIAH: implications for proteasomal function and Lewy body formation. J Biol Chem 2005; 280:42877–42886Google Scholar
120. King TD, Bijur GN, Jope RS: Caspase-3 activation induced by inhibition of mitochondrial complex I is facilitated by glycogen synthase kinase-3beta and attenuated by lithium. Brain Res 2001; 919:106–114Google Scholar
121. Chen G, Bower KA, Ma C, et al: Glycogen synthase kinase 3beta (GSK3beta) mediates 6-hydroxydopamine-induced neuronal death. FASEB J 2004; 18:1162–1164Google Scholar
122. Wang W, Yang Y, Ying C, et al: Inhibition of glycogen synthase kinase-3beta protects dopaminergic neurons from MPTP toxicity. Neuropharmacology 2007; 52:1678–1684Google Scholar
123. Bychkov E, Ahmed MR, Dalby KN, et al: Dopamine depletion and subsequent treatment with l -DOPA, but not the long-lived dopamine agonist pergolide, enhances activity of the Akt pathway in the rat striatum. J Neurochem 2007; 102:699–711 Google Scholar
124. Koh SH, Song C, Noh MY, et al: Inhibition of glycogen synthase kinase-3 reduces l -dopa-induced neurotoxicity. Toxicology 2008; 247:112–118 Google Scholar
125. Mani RB: The evaluation of disease modifying therapies in Alzheimer’s disease: a regulatory viewpoint. Stat Med 2004; 23:305–314Google Scholar
126. Mignot E, Nishino S, Guilleminault C, et al: Modafinil binds to the dopamine uptake carrier site with low affinity. Sleep 1994; 17:436–437Google Scholar
127. Wisor JP, Nishino S, Sora I, et al: Dopaminergic role in stimulant-induced wakefulness. J Neurosci 2001; 21:1787–1794Google Scholar
128. Madras BK, Xie Z, Lin Z, et al: Modafinil occupies dopamine and norepinephrine transporters in vivo and modulates the transporters and trace amine activity in vitro. J Pharmacol Exp Ther 2006; 319:561–569Google Scholar
129. Korotkova TM, Klyuch BP, Ponomarenko AA, et al: Modafinil inhibits rat midbrain dopaminergic neurons through D2-like receptors. Neuropharmacology 2007; 52:626–633Google Scholar
130. Nishino S, Mao J, Sampathkumaran R, et al: Increased dopaminergic transmission mediates the wake-promoting effects of CNS stimulants. Sleep Res Online 1998; 1:49–61Google Scholar
131. Taneja I, Diedrich A, Black BK, et al: Modafinil elicits sympathomedullary activation. Hypertension 2005; 45:612–618Google Scholar
132. Hou RH, Freeman C, Langley RW, et al: Does modafinil activate the locus coeruleus in man? Comparison of modafinil and clonidine on arousal and autonomic functions in human volunteers. Psychopharmacology (Berl) 2005; 181:537–549Google Scholar
133. Högl B, Saletu M, Brandauer E, et al: Modafinil for the treatment of daytime sleepiness in Parkinson’s disease: a double-blind, randomized, crossover, placebo-controlled polygraphic trial. Sleep 2002; 25:905–909Google Scholar
134. Carter GT, Weiss MD, Lou JS, et al: Modafinil to treat fatigue in amyotrophic lateral sclerosis: an open label pilot study. Am J Hosp Palliat Care 2005; 22:55–59Google Scholar
135. Randall DC, Fleck NL, Shneerson JM, et al: The cognitive-enhancing properties of modafinil are limited in non-sleep-deprived middle-aged volunteers. Pharmacol Biochem Behav 2004; 77:547–555Google Scholar
136. Ferraro L, Antonelli T, Tanganelli S, et al: The vigilance promoting drug modafinil increases extracellular glutamate levels in the medial preoptic area and the posterior hypothalamus of the conscious rat: prevention by local GABAA receptor blockade. Neuropsychopharmacology 1999; 20:346–356Google Scholar
137. Whitlock JR, Heynen AJ, Shuler MG, et al: Learning induces long-term potentiation in the hippocampus. Science 2006; 313:1093–1097Google Scholar
138. Zhong WX, Dong ZF, Tian M, et al: N-methyl-D-aspartate receptor-dependent long-term potentiation in CA1 region affects synaptic expression of glutamate receptor subunits and associated proteins in the whole hippocampus. Neuroscience 2006; 141:1399–1413Google Scholar
139. Taylor FB, Russo J: Efficacy of modafinil compared to dextroamphetamine for the treatment of attention deficit hyperactivity disorder in adults. J Child Adolesc Psychopharmacol 2000; 10:311–320Google Scholar
140. Turner DC, Clark L, Dowson J, et al: Modafinil improves cognition and response inhibition in adult attention-deficit/hyperactivity disorder. Biol Psychiatry 2004; 55:1031–1040Google Scholar
141. Turner DC, Clark L, Pomarol-Clotet E, et al: Modafinil improves cognition and attentional set shifting in patients with chronic schizophrenia. Neuropsychopharmacology 2004; 29:1363–1373Google Scholar
142. Schwartz JR, Nelson MT, Schwartz ER, et al: Effects of modafinil on wakefulness and executive function in patients with narcolepsy experiencing late-day sleepiness. Clin Neuropharmacol 2004; 27:74–79Google Scholar
143. Walsh JK, Randazzo AC, Stone KL, et al: Modafinil improves alertness, vigilance, and executive function during simulated night shifts. Sleep 2004; 27:434–439Google Scholar
144. Turner DC, Robbins TW, Clark L, et al: Cognitive enhancing effects of modafinil in healthy volunteers. Psychopharmacology (Berl) 2003; 165:260–269Google Scholar
145. Hunter MD, Ganesan V, Wilkinson ID, et al: Impact of modafinil on prefrontal executive function in schizophrenia. Am J Psychiatry 2006; 163:2184–2186Google Scholar
146. Biederman J, Swanson JM, Wigal SB, et al: Efficacy and safety of modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder: results of a randomized, double-blind, placebo-controlled, flexible-dose study. Pediatrics 2005; 116:777–784Google Scholar
147. Swanson JM, Greenhill LL, Lopez FA, et al: Modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder: results of a randomized, double-blind, placebo-controlled, fixed-dose study followed by abrupt discontinuation. J Clin Psychiatry 2006; 67:137–147Google Scholar
148. Greenhill LL, Biederman J, Boellner SW, et al: A randomized, double-blind, placebo-controlled study of modafinil film-coated tablets in children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2006; 45:503–511Google Scholar
149. Biederman J, Swanson JM, Wigal SB, et al: A comparison of once-daily and divided doses of modafinil in children with attention-deficit/hyperactivity disorder: a randomized, double-blind, and placebo-controlled study. J Clin Psychiatry 2006; 67:727–735Google Scholar
150. Randall DC, Viswanath A, Bharania P, et al: Does modafinil enhance cognitive performance in young volunteers who are not sleep-deprived? J Clin Psychopharmacol 2005; 25:175–179Google Scholar
151. Schillerstrom JE, Seaman JS: Modafinil augmentation of mirtazapine in a failure-to-thrive geriatric inpatient. Int J Psychiatry Med 2002; 32:405–410Google Scholar
152. Padala PR, Burke WJ, Bhatia SC: Modafinil therapy for apathy in an elderly patient. Ann Pharmacother 2007; 41:346–349Google Scholar
153. Carter GT, Han JJ, Mayadev A, et al: Modafinil reduces fatigue in Charcot-Marie-Tooth disease type 1A: a case series. Am J Hosp Palliat Care 2006; 23:412–416Google Scholar
154. Fava M, Thase ME, DeBattista C: A multicenter, placebo-controlled study of modafinil augmentation in partial responders to selective serotonin reuptake inhibitors with persistent fatigue and sleepiness. J Clin Psychiatry 2005; 66:85–93Google Scholar
155. Rasmussen NA, Schroder P, Olsen LR, et al: Modafinil augmentation in depressed patients with partial response to antidepressants: a pilot study on self-reported symptoms covered by the Major Depression Inventory (MDI) and the Symptom Checklist (SCL-92). Nord J Psychiatry 2005; 59:173–178Google Scholar
156. Thase ME, Fava M, DeBattista C, et al: Modafinil augmentation of SSRI therapy in patients with major depressive disorder and excessive sleepiness and fatigue: a 12-week, open-label, extension study. CNS Spectr 2006; 11:93–102Google Scholar
157. Vaishnavi S, Gadde K, Alamy S, et al: Modafinil for atypical depression: effects of open-label and double-blind discontinuation treatment. J Clin Psychopharmacol 2006; 26:373–378Google Scholar
158. Ferraro L, Antonelli T, O’Connor WT, et al: The effects of modafinil on striatal, pallidal and nigral GABA and glutamate release in the conscious rat: evidence for a preferential inhibition of striato-pallidal GABA transmission. Neurosci Lett 1998; 253:135–138Google Scholar
159. Antonelli T, Ferraro L, Hillion J, et al: Modafinil prevents glutamate cytotoxicity in cultured cortical neurons. Neuroreport 1998; 9:4209–4213Google Scholar
160. Jenner P, Zeng BY, Smith LA, et al: Antiparkinsonian and neuroprotective effects of modafinil in the MPTP-treated common marmoset. Exp Brain Res 2000; 133:178–188Google Scholar
161. van Vliet SA, Vanwersch RA, Jongsma MJ, et al: Neuroprotective effects of modafinil in a marmoset Parkinson model: behavioral and neurochemical aspects. Behav Pharmacol 2006; 17:453–462Google Scholar
162. Xiao YL, Fu JM, Dong Z, et al: Neuroprotective mechanism of modafinil on Parkinson disease induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine. Acta Pharmacol Sin 2004; 25:301–305Google Scholar
163. Aguirre JA, Cintra A, Hillion J, et al: A stereological study on the neuroprotective actions of acute modafinil treatment on 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced nigral lesions of the male black mouse. Neurosci Lett 1999; 275:215–218Google Scholar
164. Bymaster FP, Lee TC, Knadler MP, et al: The dual transporter inhibitor duloxetine: a review of its preclinical pharmacology, pharmacokinetic profile, and clinical results in depression. Curr Pharm Des 2005; 11:1475–1493Google Scholar
165. Raskin J, Wiltse CG, Siegal A, et al: Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial. Am J Psychiatry 2007; 164:900–909Google Scholar
166. Nyth AL, Gottfries CG: The clinical efficacy of citalopram in treatment of emotional disturbances in dementia disorders: a Nordic multicentre study. Br J Psychiatry 1990; 157:894–901Google Scholar
167. Alexopoulos GS, Jeste DV, Chung H, et al: The expert consensus guideline series. Treatment of dementia and its behavioral disturbances: Introduction: methods, commentary, and summary. Postgrad Med 2005; Spec No:6–22Google Scholar
168. Thompson S, Herrmann N, Rapoport MJ, et al: Efficacy and safety of antidepressants for treatment of depression in Alzheimer’s disease: a meta-analysis. Can J Psychiatry 2007; 52:248–255Google Scholar
169. Richard IH: Depression in Parkinson’s disease. Curr Treat Options Neurol 2000; 2:263–274Google Scholar
170. Shabnam GN, Th C, Kho D, et al: Therapies for depression in Parkinson’s disease. Cochrane Database Syst Rev 2003; 3:CD003465Google Scholar
171. Chung TH, Deane KH, Ghazi-Noori S, et al: Systematic review of antidepressant therapies in Parkinson’s disease. Parkinsonism Relat Disord 2003; 10:59–65Google Scholar
172. Menza M, Marin H, Kaufman K, et al: Citalopram treatment of depression in Parkinson’s disease: the impact on anxiety, disability, and cognition. J Neuropsychiatry Clin Neurosci 2004; 16:315–319Google Scholar
173. Weintraub D, Taraborelli D, Morales KH, et al: Escitalopram for major depression in Parkinson’s disease: an open-label, flexible-dosage study. J Neuropsychiatry Clin Neurosci 2006; 18:377–383Google Scholar
174. Lemke MR: Effect of reboxetine on depression in Parkinson’s disease patients. J Clin Psychiatry 2002; 63:300–304Google Scholar
175. Devos D, Dujardin K, Poirot I, et al: Comparison of desipramine and citalopram treatments for depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled study. Mov Disord 2008; 23:850–857Google Scholar
176. Pancrazi MP, Metais P: [Treatment of the psychological and behavioral disorders of Alzheimer’s disease.] Presse Med 2005; 34:667–672 (French)Google Scholar
177. Tanaka M, Kita T: Paroxetine and improvement of visual hallucinations in patients with dementia with Lewy bodies. J Am Geriatr Soc 2005; 53:732–733Google Scholar
178. Meco G, Bernardi S: Antidepressant use in treatment of psychosis with comorbid depression in Parkinson’s disease. Prog Neuropsychopharmacol Biol Psychiatry 2007; 31:311–313Google Scholar
179. Voon V, Lang AE: Antidepressants in the treatment of psychosis with comorbid depression in Parkinson’s disease. Clin Neuropharmacol 2004; 27:90–92Google Scholar
180. Sa DS, Kapur S, Lang AE: Amoxapine shows an antipsychotic effect but worsens motor function in patients with Parkinson’s disease and psychosis. Clin Neuropharmacol 2001; 24:242–244Google Scholar
181. Pollock BG, Mulsant BH, Rosen J, et al: A double-blind comparison of citalopram and risperidone for the treatment of behavioral and psychotic symptoms associated with dementia. Am J Geriatr Psychiatry 2007; 15:942–952Google Scholar
182. Kurita M, Sato T, Nishino S, et al: Effects of fluvoxamine on behavioral and psychological symptoms of dementia in Alzheimer’s disease: a report of three cases. Fukushima J Med Sci 2006; 52:143–148Google Scholar
183. Chalon S, Pereira A, Lainey E, et al: Comparative effects of duloxetine and desipramine on sleep EEG in healthy subjects. Psychopharmacology (Berl) 2005; 177:357–366Google Scholar
184. Kluge M, Schüssler P, Steiger A: Duloxetine increases stage 3 sleep and suppresses rapid eye movement (REM) sleep in patients with major depression. Eur Neuropsychopharmacol 2007; 17:527–531Google Scholar
185. Franco KN, Messinger-Rapport B: Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. J Am Med Dir Assoc 2006; 7:201–202Google Scholar
186. Lanctôt KL, Herrmann N, van Reekum R, et al: Gender, aggression, and serotonergic function are associated with response to sertraline for behavioral disturbances in Alzheimer’s disease. Int J Geriatr Psychiatry 2002; 17:531–541Google Scholar
187. Flint AJ, van Reekum R: The pharmacologic treatment of Alzheimer’s disease: a guide for the general psychiatrist. Can J Psychiatry 1998; 43:689–697Google Scholar
188. Leo RJ, Kim KY: Clomipramine treatment of paraphilias in elderly demented patients. J Geriatr Psychiatry Neurol 1995; 8:123–124Google Scholar
189. Swartz JR, Miller BL, Lesser IM, et al: Frontotemporal dementia: treatment response to serotonin selective reuptake inhibitors. J Clin Psychiatry 1997; 58:212–216Google Scholar
190. Nyth AL, Gottfries CG, Lyby K, et al: A controlled multicenter clinical study of citalopram and placebo in elderly depressed patients with and without concomitant dementia. Acta Psychiatr Scand 1992; 86:138–145Google Scholar
191. Greenwald BS, Kramer-Ginsberg E, Marin DB, et al: Dementia with coexistent major depression. Am J Psychiatry 1989; 146:1472–1478Google Scholar
192. Fregni F, Santos CM, Myczkowski ML, et al: Repetitive transcranial magnetic stimulation is as effective as fluoxetine in the treatment of depression in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 2004; 75:1171–1174Google Scholar
193. Munro CA, Brandt J, Sheppard JM, et al: Cognitive response to pharmacological treatment for depression in Alzheimer disease: secondary outcomes from the depression in Alzheimer’s disease study (DIADS). Am J Geriatr Psychiatry 2004; 12:491–498Google Scholar
194. Caballero J, Nahata MC: Atomoxetine hydrochloride for the treatment of attention-deficit/hyperactivity disorder. Clin Ther 2003; 25:3065–3083Google Scholar
195. Buitelaar JK, Danckaerts M, Gillberg C, et al: A prospective, multicenter, open-label assessment of atomoxetine in non-North American children and adolescents with ADHD. Eur Child Adolesc Psychiatry 2004; 13:249–257Google Scholar
196. Newman LA, Darling J, McGaughy J: Atomoxetine reverses attentional deficits produced by noradrenergic deafferentation of medial prefrontal cortex. Psychopharmacology (Berl) 2008; 200:39–50Google Scholar
197. Boggio PS, Fregni F, Bermpohl F, et al: Effect of repetitive TMS and fluoxetine on cognitive function in patients with Parkinson’s disease and concurrent depression. Mov Disord 2005; 20:1178–1184Google Scholar
198. Carboni E, Silvagni A: Dopamine reuptake by norepinephrine neurons: exception or rule? Crit Rev Neurobiol 2004; 16:121–128Google Scholar
199. Chatterjee A, Fahn S: Methylphenidate treats apathy in Parkinson’s disease. J Neuropsychiatry Clin Neurosci 2002; 14:461–462Google Scholar
200. Roth RM, Flashman LA, McAllister TW: Apathy and its treatment. Curr Treat Options Neurol 2007; 9:363–370Google Scholar
201. Gasparini M, Fabrizio E, Bonifati V, et al: Cognitive improvement during tolcapone treatment in Parkinson’s disease. J Neural Transm 1997; 104:887–894Google Scholar
202. Tohgi H, Abe T, Takahashi S, et al: Monoamine metabolism in the cerebrospinal fluid in Parkinson’s disease: relationship to clinical symptoms and subsequent therapeutic outcomes. J Neural Transm Park Dis Dement Sect 1993; 5:17–26Google Scholar
203. Narabayashi H, Yokochi F, Ogawa T, et al: [Analysis of L-threo-3,4-dihydroxyphenylserine effect on motor and psychological symptoms in Parkinson’s disease.] No To Shinkei 1991; 43:263–268 (Japanese)Google Scholar
204. Brotchie JM: Adjuncts to dopamine replacement: a pragmatic approach to reducing the problem of dyskinesia in Parkinson’s disease. Mov Disord 1998; 13:871–876Google Scholar
205. Kannari K, Kurahashi K, Tomiyama M, et al: [Tandospirone citrate, a selective 5-HT1A agonist, alleviates l -dopa-induced dyskinesia in patients with Parkinson’s disease.] No To Shinkei 2002; 54:133–137 (Japanese) Google Scholar
206. Savola JM, Hill M, Engstrom M, et al: Fipamezole (JP-1730) is a potent alpha2 adrenergic receptor antagonist that reduces levodopa-induced dyskinesia in the MPTP-lesioned primate model of Parkinson’s disease. Mov Disord 2003; 18:872–883Google Scholar
207. Thor KB, Katofiasc MA: Effects of duloxetine, a combined serotonin and norepinephrine reuptake inhibitor, on central neural control of lower urinary tract function in the chloralose-anesthetized female cat. J Pharmacol Exp Ther 1995; 274:1014–1024Google Scholar
208. Nitti VW: Duloxetine: a new pharmacologic therapy for stress urinary incontinence. Rev Urol 2004; 6(suppl 3):S48–S55Google Scholar
209. Zahariou A, Papaioannou P, Kalogirou G: Is HCl duloxetine effective in the management of urinary stress incontinence after radical prostatectomy? Urol Int 2006; 77:9–12Google Scholar
210. Steers WD, Herschorn S, Kreder KJ, et al: Duloxetine compared with placebo for treating women with symptoms of overactive bladder. Br J Urology Internat 2007; 100:337–345Google Scholar
211. Nelson RL, Guo Z, Halagappa VM, et al: Prophylactic treatment with paroxetine ameliorates behavioral deficits and retards the development of amyloid and tau pathologies in 3xTgAD mice. Exp Neurol 2007; 205:166–176Google Scholar
212. Li X, Rosborough KM, Friedman AB, et al: Regulation of mouse brain glycogen synthase kinase-3 by atypical antipsychotics. Int J Neuropsychopharmacol 2007; 10:7–19Google Scholar
213. Roh MS, Eom TY, Zmijewska AA, et al: Hypoxia activates glycogen synthase kinase-3 in mouse brain in vivo: protection by mood stabilizers and imipramine. Biol Psychiatry 2005; 57:278–286Google Scholar
214. Li X, Zhu W, Roh MS, et al: In vivo regulation of glycogen synthase kinase-3beta (GSK3beta) by serotonergic activity in mouse brain. Neuropsychopharmacology 2004; 29:1426–1431Google Scholar
215. Dong H, Goico B, Martin M, et al: Modulation of hippocampal cell proliferation, memory, and amyloid plaque deposition in APPsw (Tg2576) mutant mice by isolation stress. Neuroscience 2004; 127:601–609Google Scholar
216. Nahon E, Israelson A, Abu-Hamad S, et al: Fluoxetine (Prozac) interaction with the mitochondrial voltage-dependent anion channel and protection against apoptotic cell death. FEBS Lett 2005; 579:5105–5110Google Scholar
217. Chiou SH, Chen SJ, Peng CH, et al: Fluoxetine up-regulates expression of cellular FLICE-inhibitory protein and inhibits LPS-induced apoptosis in hippocampus-derived neural stem cell. Biochem Biophys Res Commun 2006; 343:391–400Google Scholar
218. Serafeim A, Grafton G, Chamba A, et al: 5-hydroxytryptamine drives apoptosis in biopsylike Burkitt lymphoma cells: reversal by selective serotonin reuptake inhibitors. Blood 2002; 99:2545–2553Google Scholar
219. Bengel D, Isaacs KR, Heils A, et al: The appetite suppressant d-fenfluramine induces apoptosis in human serotonergic cells. Neuroreport 1998; 9:2989–2993Google Scholar
220. Meredith EJ, Holder MJ, Chamba A, et al: The serotonin transporter (SLC6A4) is present in B-cell clones of diverse malignant origin: probing a potential anti-tumor target for psychotropics. FASEB J 2005; 19:1187–1189Google Scholar
221. Lee HJ, Kim JW, Yim SV, et al: Fluoxetine enhances cell proliferation and prevents apoptosis in dentate gyrus of maternally separated rats. Mol Psychiatry 2001; 6:610, 725–728Google Scholar
222. Delgado PL, Miller HL, Salomon RM, et al: Tryptophan-depletion challenge in depressed patients treated with desipramine or fluoxetine: implications for the role of serotonin in the mechanism of antidepressant action. Biol Psychiatry 1999; 46:212–220Google Scholar
223. Javors MA, Houston JP, Tekell JL, et al: Reduction of platelet serotonin content in depressed patients treated with either paroxetine or desipramine. Int J Neuropsychopharmacol 2000; 3:229–235Google Scholar
224. Rahmani M, Reese E, Dai Y, et al: Coadministration of histone deacetylase inhibitors and perifosine synergistically induces apoptosis in human leukemia cells through Akt and ERK1/2 inactivation and the generation of ceramide and reactive oxygen species. Cancer Res 2005; 65:2422–2432Google Scholar
225. Corda S, Laplace C, Vicaut E, et al: Rapid reactive oxygen species production by mitochondria in endothelial cells exposed to tumor necrosis factor-alpha is mediated by ceramide. Am J Respir Cell Mol Biol 2001; 24:762–768Google Scholar
226. Therade-Matharan S, Laemmel E, Carpentier S, et al: Reactive oxygen species production by mitochondria in endothelial cells exposed to reoxygenation after hypoxia and glucose depletion is mediated by ceramide. Am J Physiol Regul Integr Comp Physiol 2005; 289:R1756–R1762Google Scholar
227. Tang TS, Slow E, Lupu V, et al: Disturbed Ca2+ signaling and apoptosis of medium spiny neurons in Huntington’s disease. Proc Natl Acad Sci U S A 2005; 102:2602–2607Google Scholar
228. Tsao CW, Cheng JT, Lin YS: Down-regulation of Bcl-2, activation of caspases, and involvement of reactive oxygen species in 6-hydroxydopamine-induced thymocyte apoptosis. Neuroimmunomodulation 2002–2003; 10:328–336Google Scholar
229. Tsao CW, Cheng JT, Shen CL, et al: 6-hydroxydopamine induces thymocyte apoptosis in mice. J Neuroimmunol 1996; 65:91–95Google Scholar
230. Muranaka S, Kanno T, Fujita H, et al: Involvement of ceramide in the mechanism of Cr(VI)-induced apoptosis of CHO cells. Free Radic Res 2004; 38:613–621Google Scholar
231. Chatterjee M, Wu S: Cell line dependent involvement of ceramide in ultraviolet light-induced apoptosis. Mol Cell Biochem 2001; 219:21–27Google Scholar
232. Pilane CM, LaBelle EF: NO induced apoptosis of vascular smooth muscle cells accompanied by ceramide increase. J Cell Physiol 2004; 199:310–315Google Scholar
233. Li YF, Luo ZP: Desipramine antagonized corticosterone-induced apoptosis in cultured PC12 cells. Acta Pharmacol Sin 2002; 23:311–314Google Scholar
234. Li YF, Gong ZH, Yang M, et al: Inhibition of the oligosaccharides extracted from Morinda officinalis, a Chinese traditional herbal medicine, on the corticosterone induced apoptosis in PC12 cells. Life Sci 2003; 72:933–942Google Scholar
235. Walkinshaw G, Waters CM: Neurotoxin-induced cell death in neuronal PC12 cells is mediated by induction of apoptosis. Neuroscience 1994; 63:975–987Google Scholar
236. Woodgate A, MacGibbon G, Walton M, et al: The toxicity of 6-hydroxydopamine on PC12 and P19 cells. Brain Res Mol Brain Res 1999; 69:84–92Google Scholar
237. Angulo J, Cuevas P, Cuevas B, et al: Mechanisms for the inhibition of genital vascular responses by antidepressants in a female rabbit model. J Pharmacol Exp Ther 2004; 310:141–149Google Scholar
238. Osawa Y, Uchinami H, Bielawski J, et al: Roles for C16-ceramide and sphingosine 1-phosphate in regulating hepatocyte apoptosis in response to tumor necrosis factor-alpha. J Biol Chem 2005; 280:27879–27887Google Scholar
239. Lacour S, Hammann A, Grazide S, et al: Cisplatin-induced CD95 redistribution into membrane lipid rafts of HT29 human colon cancer cells. Cancer Res 2004; 64:3593–3598Google Scholar
240. Hashioka S, Klegeris A, Monji A, et al: Antidepressants inhibit interferon-gamma-induced microglial production of IL-6 and nitric oxide. Exp Neurol 2007; 206:33–42Google Scholar
241. Ferrer I, Marín C, Rey MJ, et al: BDNF and full-length and truncated TrkB expression in Alzheimer disease. Implications in therapeutic strategies. J Neuropathol Exp Neurol 1999; 58:729–739Google Scholar
242. Lee J, Fukumoto H, Orne J, et al: Decreased levels of BDNF protein in Alzheimer temporal cortex are independent of BDNF polymorphisms. Exp Neurol 2005; 194:91–96Google Scholar
243. Calabrese F, Molteni R, Maj PF, et al: Chronic duloxetine treatment induces specific changes in the expression of BDNF transcripts and in the subcellular localization of the neurotrophin protein. Neuropsychopharmacology 2007; 32:2351–2359Google Scholar
244. Fumagalli F, Racagni G, Riva MA: Shedding light into the role of BDNF in the pharmacotherapy of Parkinson’s disease. Pharmacogenomics J 2006; 6:95–104Google Scholar
245. Piccinni A, Marazziti D, Catena M, et al: Plasma and serum brain-derived neurotrophic factor (BDNF) in depressed patients during 1 year of antidepressant treatments. J Affect Disord 2008; 105:279–283Google Scholar
246. Zhang X, Zhang Z, Xie C, et al: Effect of treatment on serum glial cell line-derived neurotrophic factor in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 2008; 32:886–890Google Scholar
247. Hisaoka K, Nishida A, Koda T, et al: Antidepressant drug treatments induce glial cell line-derived neurotrophic factor (GDNF) synthesis and release in rat C6 glioblastoma cells. J Neurochem 2001; 79:25–34Google Scholar
248. Shibata SB, Osumi Y, Yagi M, et al: Administration of amitriptyline attenuates noise-induced hearing loss via glial cell line-derived neurotrophic factor (GDNF) induction. Brain Res 2007; 1144:74–81Google Scholar
249. Hisaoka K, Takebayashi M: [Glia as targets for antidepressants: an involvement in glial cell line-derived neurotrophic factor.] Nihon Shinkei Seishin Yakurigaku Zasshi 2007; 27:173–179 (Japanese)Google Scholar
250. Stahl SM, Shayegan DK: The psychopharmacology of ziprasidone: receptor-binding properties and real-world psychiatric practice. J Clin Psychiatry 2003; 64(suppl 19):6–12Google Scholar
251. Nemeroff CB, Lieberman JA, Weiden PJ, et al: From clinical research to clinical practice: a 4-year review of ziprasidone. CNS Spectr 2005; 10:s1–s20Google Scholar
252. Arango C, Gómez-Beneyto M, Brenlla J, et al: A 6-month prospective, observational, naturalistic, uncontrolled study to evaluate the effectiveness and tolerability of oral ziprasidone in patients with schizophrenia. Eur Neuropsychopharmacol 2007; 17:456–463Google Scholar
253. Kasckow JW, Mulchahey JJ, Mohamed S: The use of novel antipsychotics in the older patient with neurodegenerative disorders in the long-term care setting. J Am Med Dir Assoc 2004; 5:242–248Google Scholar
254. Battaglia J: Pharmacological management of acute agitation. Drugs 2005; 65:1207–1222Google Scholar
255. Oechsner M, Korchounov A: Parenteral ziprasidone: a new atypical neuroleptic for emergency treatment of psychosis in Parkinson’s disease? Hum Psychopharmacol 2005; 20:203–205Google Scholar
256. Cole SA, Saleem R, Shea WP, et al: Ziprasidone for agitation or psychosis in dementia: four cases. Int J Psychiatry Med 2005; 35:91–98Google Scholar
257. Wilner KD, Anziano RJ, Johnson AC, et al: The anxiolytic effect of the novel antipsychotic ziprasidone compared with diazepam in subjects anxious before dental surgery. J Clin Psychopharmacol 2002; 22:206–210Google Scholar
258. Nemeroff CB: Use of atypical antipsychotics in refractory depression and anxiety. J Clin Psychiatry 2005; 66(suppl 8):13–21Google Scholar
259. Papakostas GI, Petersen TJ, Nierenberg AA, et al: Ziprasidone augmentation of selective serotonin reuptake inhibitors (SSRIs) for SSRI-resistant major depressive disorder. J Clin Psychiatry 2004; 65:217–221Google Scholar
260. Cohrs S, Meier A, Neumann AC, et al: Improved sleep continuity and increased slow wave sleep and REM latency during ziprasidone treatment: a randomized, controlled, crossover trial of 12 healthy male subjects. J Clin Psychiatry 2005; 66:989–996Google Scholar
261. Byerly MJ, Weber MT, Brooks DL, et al: Antipsychotic medications and the elderly: effects on cognition and implications for use. Drugs Aging 2001; 18:45–61Google Scholar
262. Berkowitz A: Ziprasidone for dementia in elderly patients: case review. J Psychiatr Pract 2003; 9:469–473Google Scholar
263. Daniel DG, Zimbroff DL, Potkin SG, et al: Ziprasidone 80 mg/day and 160 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 6-week placebo-controlled trial. Ziprasidone Study Group. Neuropsychopharmacology 1999; 20:491–505Google Scholar
264. Arato M, O’Connor R, Meltzer HY, et al: A 1-year, double-blind, placebo-controlled trial of ziprasidone 40, 80 and 160 mg/day in chronic schizophrenia: the Ziprasidone Extended Use in Schizophrenia (ZEUS) study. Int Clin Psychopharmacol 2002; 17:207–215Google Scholar
265. Olié JP, Spina E, Murray S, et al: Ziprasidone and amisulpride effectively treat negative symptoms of schizophrenia: results of a 12-week, double-blind study. Int Clin Psychopharmacol 2006; 21:143–151Google Scholar
266. Harvey PD: Ziprasidone and cognition: the evolving story. J Clin Psychiatry 2003; 64(suppl 19):33–39Google Scholar
267. Harvey PD, Siu C, Romano S: Randomized, controlled, double-blind, multicenter comparison of the cognitive effects of ziprasidone versus olanzapine in acutely ill inpatients with schizophrenia or schizoaffective disorder. Psychopharmacology (Berl) 2004; 172:324–332Google Scholar
268. Loebel A, Siu C, Romano S: Improvement in prosocial functioning after a switch to ziprasidone treatment. CNS Spectr 2004; 9:357–364Google Scholar
269. Porter RJ, Lunn BS, Walker LL, et al: Cognitive deficit induced by acute tryptophan depletion in patients with Alzheimer’s disease. Am J Psychiatry 2000; 157:638–640Google Scholar
270. Porter RJ, Lunn BS, O’Brien JT: Effects of acute tryptophan depletion on cognitive function in Alzheimer’s disease and in the healthy elderly. Psychol Med 2003; 33:41–49Google Scholar
271. Gómez-Esteban JC, Zarranz JJ, Velasco F, et al: Use of ziprasidone in parkinsonian patients with psychosis. Clin Neuropharmacol 2005; 28:111–114Google Scholar
272. Maurice T, Su TP, Privat A: Sigma1 (sigma 1) receptor agonists and neurosteroids attenuate B25–35-amyloid peptide-induced amnesia in mice through a common mechanism. Neuroscience 1998; 83:413–428Google Scholar
273. Palotás A, Penke B, Palotás M, et al: Haloperidol attenuates beta-amyloid-induced calcium imbalance in human fibroblasts. Skin Pharmacol Physiol 2004; 17:195–199Google Scholar
274. Lee CS, Park SY, Ko HH, et al: Inhibition of MPP + -induced mitochondrial damage and cell death by trifluoperazine and W-7 in PC12 cells. Neurochem Int 2005; 46:169–178 Google Scholar
275. Lee CS, Park WJ, Ko HH, et al: Differential involvement of mitochondrial permeability transition in cytotoxicity of 1-methyl-4-phenylpyridinium and 6-hydroxydopamine. Mol Cell Biochem 2006; 289:193–200Google Scholar
276. Lee SJ, Youn YC, Han ES, et al: Depressant effect of mitochondrial respiratory complex inhibitors on proteasome inhibitor-induced mitochondrial dysfunction and cell death in PC12 cells. Neurochem Res 2005; 30:1191–1200Google Scholar
277. Ozaki N, Tokunage Y, Wakashiro S, et al: Evaluation of cytoprotective drugs for liver preservation by pyridine nucleotide fluorometry. Surgery 1988; 104:98–103Google Scholar
278. Zhelev Z, Ohba H, Bakalova R, et al: Phenothiazines suppress proliferation and induce apoptosis in cultured leukemic cells without any influence on the viability of normal lymphocytes: phenothiazines and leukemia. Cancer Chemother Pharmacol 2004; 53:267–275Google Scholar
279. Beitner R, Chen-Zion M, Sofer-Bassukevitz Y, et al: Therapeutic and prophylactic treatment of skin burns with several calmodulin antagonists. Gen Pharmacol 1989; 20:165–173Google Scholar
280. Beitner R, Chen-Zion M, Sofer-Bassukevitz Y, et al: Treatment of frostbite with the calmodulin antagonists thioridazine and trifluoperazine. Gen Pharmacol 1989; 20:641–646Google Scholar
281. Rodrigues T, Santos AC, Pigoso AA, et al: Thioridazine interacts with the membrane of mitochondria acquiring antioxidant activity toward apoptosis–potentially implicated mechanisms. Br J Pharmacol 2002; 136:136–142Google Scholar
282. Wang H, Xu H, Dyck LE, et al: Olanzapine and quetiapine protect PC12 cells from beta-amyloid peptide (25–35)-induced oxidative stress and the ensuing apoptosis. J Neurosci Res 2005; 81:572–580Google Scholar
283. Pillai A, Parikh V, Terry AV Jr, et al: Long-term antipsychotic treatments and crossover studies in rats: differential effects of typical and atypical agents on the expression of antioxidant enzymes and membrane lipid peroxidation in rat brain. J Psychiatr Res 2007; 41:372–386Google Scholar
284. Ray SD, Balasubramanian G, Bagchi D, et al: Ca(2+)-calmodulin antagonist chlorpromazine and poly(ADP-ribose) polymerase modulators 4-aminobenzamide and nicotinamide influence hepatic expression of BCL-XL and P53 and protect against acetaminophen-induced programmed and unprogrammed cell death in mice. Free Radic Biol Med 2001; 31:277–291Google Scholar
285. Maeda S, Suzuki A, Lin KH, et al: DNA fragmentation induced in high-cell-density culture of primary rat hepatocytes is an active process dependent on energy availability, gene expression, and calmodulin. J Biochem (Tokyo) 1995; 118:1161–1165Google Scholar
286. He P, Yan ZL, Wu MC, et al: Chlorpromazine inhibits hepatocyte apoptosis caused by withdrawal of phenobarbital in mice. Zhongguo Yao Li Xue Bao 1999; 20:970–974Google Scholar
287. He J, Xu H, Yang Y, et al: Neuroprotective effects of olanzapine on methamphetamine-induced neurotoxicity are associated with an inhibition of hyperthermia and prevention of Bcl-2 decrease in rats. Brain Res 2004; 1018:186–192Google Scholar
288. Wang C, McInnis J, Ross-Sanchez M, et al: Long-term behavioral and neurodegenerative effects of perinatal phencyclidine administration: implications for schizophrenia. Neuroscience 2001; 107:535–550Google Scholar
289. Vargas F, Rivas C, Perdomo H, et al: Clozapine prevents apoptosis and enhances receptor dependent respiratory burst in human neutrophils. Pharmazie 2005; 60:364–368Google Scholar
290. Wei Z, Mousseau DD, Richardson JS, et al: Atypical antipsychotics attenuate neurotoxicity of beta-amyloid(25–35) by modulating Bax and Bcl-X(l/s) expression and localization. J Neurosci Res 2003; 74:942–947Google Scholar
291. Qing H, Xu H, Wei Z, et al: The ability of atypical antipsychotic drugs vs. haloperidol to protect PC12 cells against MPP + -induced apoptosis. Eur J Neurosci 2003; 17:1563–1570 Google Scholar
292. Gnerre C, Kosel M, Baumann P, et al: Interaction of psychotropic drugs with monoamine oxidase in rat brain. J Pharm Pharmacol 2001; 53:1125–1130Google Scholar
293. Ahlemeyer B, Krieglstein J: Stimulation of 5-HT1A receptor inhibits apoptosis induced by serum deprivation in cultured neurons from chick embryo. Brain Res 1997; 777:179–186Google Scholar
294. Ahlemeyer B, Glaser A, Schaper C, et al: The 5-HT1A receptor agonist Bay x 3702 inhibits apoptosis induced by serum deprivation in cultured neurons. Eur J Pharmacol 1999; 370:211–216Google Scholar
295. Druse MJ, Tajuddin NF, Gillespie RA, et al: The serotonin-1A agonist ipsapirone prevents ethanol-associated death of total rhombencephalic neurons and prevents the reduction of fetal serotonin neurons. Brain Res Dev Brain Res 2004; 150:79–88Google Scholar
296. Druse M, Tajuddin NF, Gillespie RA, et al: Signaling pathways involved with serotonin1A agonist-mediated neuroprotection against ethanol-induced apoptosis of fetal rhombencephalic neurons. Brain Res Dev Brain Res 2005; 159:18–28Google Scholar
297. Terzano MG, Rossi M, Palomba V, et al: New drugs for insomnia: comparative tolerability of zopiclone, zolpidem and zaleplon. Drug Saf 2003; 26:261–282Google Scholar
298. Devanand DP: Behavioral complications and their treatment in Alzheimer’s disease. Geriatrics 1997; 52(suppl 2):S37–S39Google Scholar
299. Bliwise DL: Sleep disorders in Alzheimer’s disease and other dementias. Clin Cornerstone 2004; 6(suppl 1A):S16–S28Google Scholar
300. Cotroneo A, Gareri P, Nicoletti N, et al: Effectiveness and safety of hypnotic drugs in the treatment of insomnia in over 70-year old people. Arch Gerontol Geriatr 2007; 44(suppl 1):121–124Google Scholar
301. Mattila MJ, Vanakoski J, Kalska H, et al: Effects of alcohol, zolpidem, and some other sedatives and hypnotics on human performance and memory. Pharmacol Biochem Behav 1998; 59:917–923Google Scholar
302. Katsunuma H, Shimizu T, Ogawa K, et al: Treatment of insomnia by concomitant therapy with zopiclone and aniracetam in patients with cerebral infarction, cerebroatrophy, Alzheimer’s disease and Parkinson’s disease. Psychiatry Clin Neurosci 1998; 52:198–200Google Scholar
303. Krystal AD: Treating the health, quality of life, and functional impairments in insomnia. J Clin Sleep Med 2007; 3:63–72Google Scholar
304. Hemmeter U, Müller M, Bischof R, et al: Effect of zopiclone and temazepam on sleep EEG parameters, psychomotor and memory functions in healthy elderly volunteers. Psychopharmacology (Berl) 2000; 147:384–396Google Scholar
305. Lauterbach EC: Sleep benefit, sleep deprivation, and Parkinsonian depressive subtypes. Am J Psychiatry 1994; 151:782–783Google Scholar
306. Currie LJ, Bennett JP Jr, Harrison MB, et al: Clinical correlates of sleep benefit in Parkinson’s disease. Neurology 1997; 48:1115–1117Google Scholar
307. Merello M, Hughes A, Colosimo C, et al: Sleep benefit in Parkinson’s disease. Mov Disord 1997; 12:506–508Google Scholar
308. Tandberg E, Larsen JP, Karlsen K: Excessive daytime sleepiness and sleep benefit in Parkinson’s disease: a community-based study. Mov Disord 1999; 14:922–927Google Scholar
309. Boonstra TW, Stins JF, Daffertshofer A, et al: Effects of sleep deprivation on neural functioning: an integrative review. Cell Mol Life Sci 2007; 64:934–946Google Scholar
310. Cummings JL, Back C: The cholinergic hypothesis of neuropsychiatric symptoms in Alzheimer’s disease. Am J Geriatr Psychiatry 1998; 6(suppl 1):S64–S78Google Scholar
311. Kaufer D: Beyond the cholinergic hypothesis: the effect of metrifonate and other cholinesterase inhibitors on neuropsychiatric symptoms in Alzheimer’s disease. Dement Geriatr Cogn Disord 1998; 9(suppl 2):8–14Google Scholar
312. Terry AV Jr, Buccafusco JJ: The cholinergic hypothesis of age and Alzheimer’s disease-related cognitive deficits: recent challenges and their implications for novel drug development. J Pharmacol Exp Ther 2003; 306:821–827Google Scholar
313. Tractenberg RE, Singer CM, Kaye JA: Symptoms of sleep disturbance in persons with Alzheimer’s disease and normal elderly. J Sleep Res 2005; 14:177–185Google Scholar
314. Sagaspe P, Sanchez-Ortuno M, Charles A, et al: Effects of sleep deprivation on Color-Word, Emotional, and Specific Stroop interference and on self-reported anxiety. Brain Cogn 2006; 60:76–87Google Scholar
315. Babkoff H, Sing HC, Thorne DR, et al: Perceptual distortions and hallucinations reported during the course of sleep deprivation. Percept Mot Skills 1989; 68(part 1):787–798Google Scholar
316. Kulisevsky J, Roldan E: Hallucinations and sleep disturbances in Parkinson’s disease. Neurology 2004; 63(suppl 3):S28–S30Google Scholar
317. O’Reilly MF: Functional analysis and treatment of escape-maintained aggression correlated with sleep deprivation. J Appl Behav Anal 1995; 28:225–226Google Scholar
318. Kelly J, Feigenbaum LZ: Another cause of reversible dementia: sleep deprivation due to prostatism. J Am Geriatr Soc 1982; 30:645–646Google Scholar
319. Chassagne P, Druesne L, Bentot C, et al: [Mental confusion in the elderly.] Presse Med 2005; 34:863–868 (French)Google Scholar
320. Gorissen M, Tielemans M, Coenen A: Alertness and memory after sleep deprivation and diazepam intake. J Psychopharmacol 1997; 11:233–239Google Scholar
321. Kendall AP, Kautz MA, Russo MB, et al: Effects of sleep deprivation on lateral visual attention. Int J Neurosci 2006; 116:1125–1138Google Scholar
322. Adam M, Rétey JV, Khatami R, et al: Age-related changes in the time course of vigilant attention during 40 hours without sleep in men. Sleep 2006; 29:55–57Google Scholar
323. Pilcher JJ, Band D, Odle-Dusseau HN, et al: Human performance under sustained operations and acute sleep deprivation conditions: toward a model of controlled attention. Aviat Space Environ Med 2007; 78(suppl 5):B15–B24Google Scholar
324. Coenen AM, van Luijtelaar EL: Effects of benzodiazepines, sleep and sleep deprivation on vigilance and memory. Acta Neurol Belg 1997; 97:123–129Google Scholar
325. Chee MW, Chuah YM: Functional neuroimaging and behavioral correlates of capacity decline in visual short-term memory after sleep deprivation. Proc Natl Acad Sci U S A 2007; 104:9487–9492Google Scholar
326. Fluck E, File SE, Springett J, et al: Does the sedation resulting from sleep deprivation and lorazepam cause similar cognitive deficits? Pharmacol Biochem Behav 1998; 59:909–915Google Scholar
327. Chee MW, Chuah LY, Venkatraman V, et al: Functional imaging of working memory following normal sleep and after 24 and 35 h of sleep deprivation: correlations of fronto-parietal activation with performance. Neuroimage 2006; 31:419–428Google Scholar
328. Lim J, Choo WC, Chee MW: Reproducibility of changes in behavior and fMRI activation associated with sleep deprivation in a working memory task. Sleep 2007; 30:61–70Google Scholar
329. Mu Q, Nahas Z, Johnson KA, et al: Decreased cortical response to verbal working memory following sleep deprivation. Sleep 2005; 28:55–67Google Scholar
330. Casement MD, Broussard JL, Mullington JM, et al: The contribution of sleep to improvements in working memory scanning speed: a study of prolonged sleep restriction. Biol Psychol 2006; 72:208–212Google Scholar
331. Turner TH, Drummond SP, Salamat JS, et al: Effects of 42 hr of total sleep deprivation on component processes of verbal working memory. Neuropsychology 2007; 21:787–795Google Scholar
332. Stickgold R, Walker MP: Memory consolidation and reconsolidation: what is the role of sleep? Trends Neurosci 2005; 28:408–415Google Scholar
333. Huber R: Memory formation: sleep enough before learning. Curr Biol 2007; 17:R367–R368Google Scholar
334. Polzella DJ: Effects of sleep deprivation on short-term recognition memory. J Exp Psychol [Hum Learn] 1975; 104:194–200Google Scholar
335. Tucker MA, Hirota Y, Wamsley EJ, et al: A daytime nap containing solely non-REM sleep enhances declarative but not procedural memory. Neurobiol Learn Mem 2006; 86:241–247Google Scholar
336. Gais S, Lucas B, Born J: Sleep after learning aids memory recall. Learn Mem 2006; 13:259–262Google Scholar
337. Raidy DJ, Scharff LF: Effects of sleep deprivation on auditory and visual memory tasks. Percept Mot Skills 2005; 101:451–467Google Scholar
338. Rauchs G, Desgranges B, Foret J, et al: The relationships between memory systems and sleep stages. J Sleep Res 2005; 14:123–140Google Scholar
339. Wimmer F, Hoffmann RF, Bonato RA, et al: The effects of sleep deprivation on divergent thinking and attention processes. J Sleep Res 1992; 1:223–230Google Scholar
340. Nilsson JP, Soderstrom M, Karlsson AU, et al: Less effective executive functioning after one night’s sleep deprivation. J Sleep Res 2005; 14:1–6Google Scholar
341. Gottselig JM, Adam M, Retey JV, et al: Random number generation during sleep deprivation: effects of caffeine on response maintenance and stereotypy. J Sleep Res 2006; 15:31–40Google Scholar
342. Chuah YM, Venkatraman V, Dinges DF, et al: The neural basis of interindividual variability in inhibitory efficiency after sleep deprivation. J Neurosci 2006; 26:7156–7162Google Scholar
343. Hsieh S, Cheng IC, Tsai LL: Immediate error correction process following sleep deprivation. J Sleep Res 2007; 16:137–147Google Scholar
344. Lieberman HR, Bathalon GP, Falco CM, et al: Severe decrements in cognition function and mood induced by sleep loss, heat, dehydration, and undernutrition during simulated combat. Biol Psychiatry 2005; 57:422–429Google Scholar
345. Durmer JS, Dinges DF: Neurocognitive consequences of sleep deprivation. Semin Neurol 2005; 25:117–129Google Scholar
346. Shelton PS, Hocking LB: Zolpidem for dementia-related insomnia and nighttime wandering. Ann Pharmacother 1997; 31:319–322Google Scholar
347. Furuse S, Kanaya N, Takeda T, et al: [Comparison of zopiclone and midazolam premedication for preoperative anxiolysis.] Masui 2002; 51:1094–1099 (Japanese)Google Scholar
348. Rainer MK, Mucke HA, Masching AJ, et al: [State of the art management of BPSD in dementia.] Psychiatr Prax 2005; 32:31–38 (German)Google Scholar
349. Jackson CW, Pitner JK, Mintzer JE: Zolpidem for the treatment of agitation in elderly demented patients. J Clin Psychiatry 1996; 57:372–373Google Scholar
350. Coccaro EF, Kramer E, Zemishlany Z, et al: Pharmacologic treatment of noncognitive behavioral disturbances in elderly demented patients. Am J Psychiatry 1990; 147:1640–1645Google Scholar
351. Meehan KM, Wang H, David SR, et al: Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: a double-blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology 2002; 26:494–504Google Scholar
352. Christensen DB, Benfield WR: Alprazolam as an alternative to low-dose haloperidol in older, cognitively impaired nursing facility patients. J Am Geriatr Soc 1998; 46:620–625Google Scholar
353. Ancill RJ, Carlyle WW, Liang RA, et al: Agitation in the demented elderly: a role for benzodiazepines? Int Clin Psychopharmacol 1991; 6:141–146Google Scholar
354. Monroe RR: Anticonvulsants in the treatment of aggression. J Nerv Ment Dis 1975; 160:119–126Google Scholar
355. Yudofsky SC, Silver JM, Hales RE: Pharmacologic management of aggression in the elderly. J Clin Psychiatry 1990; 51(suppl):22–28Google Scholar
356. Volz A, Khorsand V, Gillies D, et al: Benzodiazepines for schizophrenia. Cochrane Database Syst Rev 2007; 1:CD006391Google Scholar
357. Wolkowitz OM, Pickar D: Benzodiazepines in the treatment of schizophrenia: a review and reappraisal. Am J Psychiatry 1991; 148:714–726Google Scholar
358. Wolkowitz OM, Turetsky N, Reus VI, et al: Benzodiazepine augmentation of neuroleptics in treatment-resistant schizophrenia. Psychopharmacol Bull 1992; 28:291–295Google Scholar
359. Krystal A, Fava M, Rubens R, et al: Evaluation of eszopiclone discontinuation after cotherapy with fluoxetine for insomnia with coexisting depression. J Clin Sleep Med 2007; 3:48–55Google Scholar
360. Soares CN, Joffe H, Rubens R, et al: Eszopiclone in patients with insomnia during perimenopause and early postmenopause: a randomized controlled trial. Obstet Gynecol 2006; 108:1402–1410Google Scholar
361. Kajimura N, Kato M, Okuma T, et al: Effects of zopiclone on sleep and symptoms in schizophrenia: comparison with benzodiazepine hypnotics. Prog Neuropsychopharmacol Biol Psychiatry 1994; 18:477–490Google Scholar
362. Kato M, Kajimura N, Okuma T, et al: Association between delta waves during sleep and negative symptoms in schizophrenia: pharmaco-EEG studies by using structurally different hypnotics. Neuropsychobiology 1999; 39:165–172Google Scholar
363. Louzada PR, Lima AC, Mendonca-Silva DL, et al: Taurine prevents the neurotoxicity of beta-amyloid and glutamate receptor agonists: activation of GABA receptors and possible implications for Alzheimer’s disease and other neurological disorders. FASEB J 2004; 18:511–518Google Scholar
364. García-Santos G, Herrera F, Martin V, et al: Antioxidant activity and neuroprotective effects of zolpidem and several synthesis intermediates. Free Radic Res 2004; 38:1289–1299Google Scholar
365. Bishnoi M, Chopra K, Kulkarni SK: Possible anti-oxidant and neuroprotective mechanisms of zolpidem in attenuating typical anti-psychotic-induced orofacial dyskinesia: a biochemical and neurochemical study. Prog Neuropsychopharmacol Biol Psychiatry 2007; 31:1130–1138Google Scholar
366. Berson A, Descatoire V, Sutton A, et al: Toxicity of alpidem, a peripheral benzodiazepine receptor ligand, but not zolpidem, in rat hepatocytes: role of mitochondrial permeability transition and metabolic activation. J Pharmacol Exp Ther 2001; 299:793–800Google Scholar
367. Galeffi F, Sinnar S, Schwartz-Bloom RD: Diazepam promotes ATP recovery and prevents cytochrome c release in hippocampal slices after in vitro ischemia. J Neurochem 2000; 75:1242–1249Google Scholar
368. Benedetti F, Serretti A, Colombo C, et al: A glycogen synthase kinase 3-beta promoter gene single nucleotide polymorphism is associated with age at onset and response to total sleep deprivation in bipolar depression. Neurosci Lett 2004; 368:123–126Google Scholar
369. Sehgal A, Joiner W, Crocker A, et al: Molecular analysis of sleep: wake cycles in Drosophila. Cold Spring Harb Symp Quant Biol 2007; 72:557–564Google Scholar
370. Kumar A, Singh A: Protective effect of St. John’s wort ( Hypericum perforatum ) extract on 72-hour sleep deprivation-induced anxiety-like behavior and oxidative damage in mice. Planta Med 2007; 73:1358–1364 Google Scholar
371. Cirelli C, Tononi G: Uncoupling proteins and sleep deprivation. Arch Ital Biol 2004; 142:541–549Google Scholar
372. Sei H, Saitoh D, Yamamoto K, et al: Differential effect of short-term REM sleep deprivation on NGF and BDNF protein levels in the rat brain. Brain Res 2000; 877:387–390Google Scholar
373. Hairston IS, Peyron C, Denning DP, et al: Sleep deprivation effects on growth factor expression in neonatal rats: a potential role for BDNF in the mediation of delta power. J Neurophysiol 2004; 91:1586–1595Google Scholar
374. Kato K, Hirai K, Nishiyama K, et al: Neurochemical properties of ramelteon (TAK-375), a selective MT1/MT2 receptor agonist. Neuropharmacology 2005; 48:301–310Google Scholar
375. Roth T, Seiden D, Sainati S, et al: Effects of ramelteon on patient-reported sleep latency in older adults with chronic insomnia. Sleep Med 2006; 7:312–318Google Scholar
376. Mini LJ, Wang-Weigand S, Zhang J: Self-reported efficacy and tolerability of ramelteon 8 mg in older adults experiencing severe sleep-onset difficulty. Am J Geriatr Pharmacother 2007; 5:177–184Google Scholar
377. Brismar K, Mogensen L, Wetterberg L: Depressed melatonin secretion in patients with nightmares due to beta-adrenoceptor blocking drugs. Acta Med Scand 1987; 221:155–158Google Scholar
378. Silber MH, Hansen MR, Girish M: Complex nocturnal visual hallucinations. Sleep Med 2005; 6:363–366Google Scholar
379. Fisher AA, Davis M, Jeffery I: Acute delirium induced by metoprolol. Cardiovasc Drugs Ther 2002; 16:161–165Google Scholar
380. Chan-Palay V, Asan E: Alterations in catecholamine neurons of the locus coeruleus in senile dementia of the Alzheimer type and in Parkinson’s disease with and without dementia and depression. J Comp Neurol 1989; 287:373–392Google Scholar
381. Szot P, White SS, Greenup JL, et al: Compensatory changes in the noradrenergic nervous system in the locus ceruleus and hippocampus of postmortem subjects with Alzheimer’s disease and dementia with Lewy bodies. J Neurosci 2006; 26:467–478Google Scholar
382. Olde Rikkert MG, Rigaud AS: Melatonin in elderly patients with insomnia: a systematic review. Z Gerontol Geriatr 2001; 34:491–497Google Scholar
383. Jansen SL, Forbes DA, Duncan V, et al: Melatonin for cognitive impairment. Cochrane Database Syst Rev 2006; 1:CD003802Google Scholar
384. Arushanian EB, Baida OA, Mastiagin SS: [Effect of melatonin on memory, individual time perception, and anxiety in young people of different chronotype groups.] Eksp Klin Farmakol 2006; 69:21–23 (Russian)Google Scholar
385. Hanania M, Kitain E: Melatonin for treatment and prevention of postoperative delirium. Anesth Analg 2002; 94:338–339Google Scholar
386. Cohen-Mansfield J, Garfinkel D, Lipson S: Melatonin for treatment of sundowning in elderly persons with dementia: a preliminary study. Arch Gerontol Geriatr 2000; 31:65–76Google Scholar
387. Suhner A, Schlagenhauf P, Tschopp A, et al: Impact of melatonin on driving performance. J Travel Med 1998; 5:7–13Google Scholar
388. Cavallo A, Ris MD, Succop P, et al: Melatonin treatment of pediatric residents for adaptation to night shift work. Ambul Pediatr 2005; 5:172–177Google Scholar
389. Gorfine T, Yeshurun Y, Zisapel N: Nap and melatonin-induced changes in hippocampal activation and their role in verbal memory consolidation. J Pineal Res 2007; 43:336–342Google Scholar
390. Boeve BF, Silber MH, Ferman TJ: Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: results in 14 patients. Sleep Med 2003; 4:281–284Google Scholar
391. Serrano C, García-Borreguero D: Fluctuations in cognition and alertness in Parkinson’s disease and dementia. Neurology 2004; 63(suppl 3):S31–S34Google Scholar
392. Iacovitti L, Stull ND, Johnston K: Melatonin rescues dopamine neurons from cell death in tissue culture models of oxidative stress. Brain Res 1997; 768:317–326Google Scholar
393. Coulom H, Birman S: Chronic exposure to rotenone models sporadic Parkinson’s disease in Drosophila melanogaster. J Neurosci 2004; 24:10993–10998 Google Scholar
394. McMillan CR, Sharma R, Ottenhof T, et al: Modulation of tyrosine hydroxylase expression by melatonin in human SH-SY5Y neuroblastoma cells. Neurosci Lett 2007; 419:202–206Google Scholar
395. Sharma R, McMillan CR, Niles LP: Neural stem cell transplantation and melatonin treatment in a 6-hydroxydopamine model of Parkinson’s disease. J Pineal Res 2007; 43:245–254Google Scholar
396. Chen ST, Chuang JI, Hong MH, et al: Melatonin attenuates MPP + -induced neurodegeneration and glutathione impairment in the nigrostriatal dopaminergic pathway. J Pineal Res 2002; 32:262–269 Google Scholar
397. Jin BK, Shin DY, Jeong MY, et al: Melatonin protects nigral dopaminergic neurons from 1-methyl-4-phenylpyridinium (MPP + ) neurotoxicity in rats. Neurosci Lett 1998; 245:61–64 Google Scholar
398. Sharma R, McMillan CR, Tenn CC, et al: Physiological neuroprotection by melatonin in a 6-hydroxydopamine model of Parkinson’s disease. Brain Res 2006; 1068:230–236Google Scholar
399. Kim YS, Joo WS, Jin BK, et al: Melatonin protects 6-OHDA-induced neuronal death of nigrostriatal dopaminergic system. Neuroreport 1998; 9:2387–2390Google Scholar
400. Sharma SK, Ebadi M: Metallothionein attenuates 3-morpholinosydnonimine (SIN-1)-induced oxidative stress in dopaminergic neurons. Antioxid Redox Signal 2003; 5:251–264Google Scholar
401. Ebadi M, Sharma SK, Ghafourifar P, et al: Peroxynitrite in the pathogenesis of Parkinson’s disease and the neuroprotective role of metallothioneins. Methods Enzymol 2005; 396:276–298Google Scholar
402. Antolin I, Mayo JC, Sainz RM, et al: Protective effect of melatonin in a chronic experimental model of Parkinson’s disease. Brain Res 2002; 943:163–173Google Scholar
403. Acuña-Castroviejo D, Coto-Montes A, Gaia Monti M, et al: Melatonin is protective against MPTP-induced striatal and hippocampal lesions. Life Sci 1997; 60:PL23–PL29Google Scholar
404. Joo WS, Jin BK, Park CW, et al: Melatonin increases striatal dopaminergic function in 6-OHDA-lesioned rats. Neuroreport 1998; 9:4123–4126Google Scholar
405. Singh S, Ahmed R, Sagar RK, et al: Neuroprotection of the nigrostriatal dopaminergic neurons by melatonin in hemiparkinsonium rat. Indian J Med Res 2006; 124:419–426Google Scholar
406. Ortiz GG, Crespo-Lopez ME, Moran-Moguel C, et al: Protective role of melatonin against MPTP-induced mouse brain cell DNA fragmentation and apoptosis in vivo. Neuro Endocrinol Lett 2001; 22:101–108Google Scholar
407. Ishido M: Melatonin inhibits maneb-induced aggregation of alpha-synuclein in rat pheochromocytoma cells. J Pineal Res 2007; 42:125–130Google Scholar
408. Lin CH, Huang JY, Ching CH, et al: Melatonin reduces the neuronal loss, downregulation of dopamine transporter, and upregulation of D2 receptor in rotenone-induced parkinsonian rats. J Pineal Res 2008; 44:205–213Google Scholar
409. Zhu LQ, Wang SH, Ling ZQ, et al: Effect of inhibiting melatonin biosynthesis on spatial memory retention and tau phosphorylation in rat. J Pineal Res 2004; 37:71–77Google Scholar
410. Zhu LQ, Wang SH, Ling ZQ, et al: Inhibition of melatonin biosynthesis activates protein kinase a and induces Alzheimer-like tau hyperphosphorylation in rats. Chin Med Sci J 2005; 20:83–87Google Scholar
411. Wang JZ, Wang ZF: Role of melatonin in Alzheimer-like neurodegeneration. Acta Pharmacol Sin 2006; 27:41–49Google Scholar
412. Cheng Y, Feng Z, Zhang QZ, et al: Beneficial effects of melatonin in experimental models of Alzheimer disease. Acta Pharmacol Sin 2006; 27:129–139Google Scholar
413. Olivieri G, Brack C, Muller-Spahn F, et al: Mercury induces cell cytotoxicity and oxidative stress and increases beta-amyloid secretion and tau phosphorylation in SHSY5Y neuroblastoma cells. J Neurochem 2000; 74:231–236Google Scholar
414. Gutierrez-Cuesta J, Sureda FX, Romeu M, et al: Chronic administration of melatonin reduces cerebral injury biomarkers in SAMP8. J Pineal Res 2007; 42:394–402Google Scholar
415. Yin J, Liu YH, Xu YF, et al: Melatonin arrests peroxynitrite-induced tau hyperphosphorylation and the overactivation of protein kinases in rat brain. J Pineal Res 2006; 41:124–129Google Scholar
416. Liu SJ, Wang JZ: Alzheimer-like tau phosphorylation induced by wortmannin in vivo and its attenuation by melatonin. Acta Pharmacol Sin 2002; 23:183–187Google Scholar
417. Deng YQ, Xu GG, Duan P, et al: Effects of melatonin on wortmannin-induced tau hyperphosphorylation. Acta Pharmacol Sin 2005; 26:519–526Google Scholar
418. Wang DL, Ling ZQ, Cao FY, et al: Melatonin attenuates isoproterenol-induced protein kinase A overactivation and tau hyperphosphorylation in rat brain. J Pineal Res 2004; 37:11–16Google Scholar
419. Li XC, Wang ZF, Zhang JX, et al: Effect of melatonin on calyculin A-induced tau hyperphosphorylation. Eur J Pharmacol 2005; 510:25–30Google Scholar
420. Matsubara E, Bryant-Thomas T, Pacheco Quinto J, et al: Melatonin increases survival and inhibits oxidative and amyloid pathology in a transgenic model of Alzheimer’s disease. J Neurochem 2003; 85:1101–1108Google Scholar
421. Cheng X, van Breemen RB: Mass spectrometry-based screening for inhibitors of beta-amyloid protein aggregation. Anal Chem 2005; 77:7012–7015Google Scholar
422. Brusco LI, Marquez M, Cardinali DP: Monozygotic twins with Alzheimer’s disease treated with melatonin: case report. J Pineal Res 1998; 25:260–263Google Scholar
423. Reiter RJ: Oxidative damage in the central nervous system: protection by melatonin. Prog Neurobiol 1998; 56:359–384Google Scholar
424. Jou MJ, Peng TI, Reiter RJ, et al: Visualization of the antioxidative effects of melatonin at the mitochondrial level during oxidative stress-induced apoptosis of rat brain astrocytes. J Pineal Res 2004; 37:55–70Google Scholar
425. Ciuffi M, Pisanello M, Pagliai G, et al: Antioxidant protection in cultured corneal cells and whole corneas submitted to UV-B exposure. J Photochem Photobiol B 2003; 71:59–68Google Scholar
426. Thomas B, Mohanakumar KP: Melatonin protects against oxidative stress caused by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine in the mouse nigrostriatum. J Pineal Res 2004; 36:25–32Google Scholar
427. Imam SZ, el-Yazal J, Newport GD, et al: Methamphetamine-induced dopaminergic neurotoxicity: role of peroxynitrite and neuroprotective role of antioxidants and peroxynitrite decomposition catalysts. Ann N Y Acad Sci 2001; 939:366–380Google Scholar
428. Lezoualc’h F, Sparapani M, Behl C: N-acetyl-serotonin (normelatonin) and melatonin protect neurons against oxidative challenges and suppress the activity of the transcription factor NF-kappaB. J Pineal Res 1998; 24:168–178Google Scholar
429. Herrera F, Sainz RM, Mayo JC, et al: Glutamate induces oxidative stress not mediated by glutamate receptors or cystine transporters: protective effect of melatonin and other antioxidants. J Pineal Res 2001; 31:356–362Google Scholar
430. Mayo JC, Sainz RM, Uria H, et al: Melatonin prevents apoptosis induced by 6-hydroxydopamine in neuronal cells: implications for Parkinson’s disease. J Pineal Res 1998; 24:179–192Google Scholar
431. Miller JW, Selhub J, Joseph JA: Oxidative damage caused by free radicals produced during catecholamine autoxidation: protective effects of O-methylation and melatonin. Free Radic Biol Med 1996; 21:241–249Google Scholar
432. Khaldy H, Escames G, León J, et al: Comparative effects of melatonin, L-deprenyl, Trolox and ascorbate in the suppression of hydroxyl radical formation during dopamine autoxidation in vitro. J Pineal Res 2000; 29:100–107Google Scholar
433. Rocchitta G, Migheli R, Esposito G, et al: Endogenous melatonin protects l -DOPA from autoxidation in the striatal extracellular compartment of the freely moving rat: potential implication for long-term l -DOPA therapy in Parkinson’s disease. J Pineal Res 2006; 40:204–213 Google Scholar
434. Maharaj H, Sukhdev Maharaj D, Scheepers M, et al: l -DOPA administration enhances 6-hydroxydopamine generation. Brain Res 2005; 1063:180–186 Google Scholar
435. Andrabi SA, Sayeed I, Siemen D, et al: Direct inhibition of the mitochondrial permeability transition pore: a possible mechanism responsible for anti-apoptotic effects of melatonin. FASEB J 2004; 18:869–871Google Scholar
436. Han YX, Zhang SH, Wang XM, et al: Inhibition of mitochondria responsible for the anti-apoptotic effects of melatonin during ischemia-reperfusion. J Zhejiang Univ Sci B 2006; 7:142–147Google Scholar
437. Leon J, Acuna-Castroviejo D, Escames G, et al: Melatonin mitigates mitochondrial malfunction. J Pineal Res 2005; 38:1–9Google Scholar
438. Saravanan KS, Sindhu KM, Mohanakumar KP: Melatonin protects against rotenone-induced oxidative stress in a hemiparkinsonian rat model. J Pineal Res 2007; 42:247–253Google Scholar
439. Absi E, Ayala A, Machado A, et al: Protective effect of melatonin against the 1-methyl-4-phenylpyridinium-induced inhibition of complex I of the mitochondrial respiratory chain. J Pineal Res 2000; 29:40–47Google Scholar
440. Martin M, Macias M, Escames G, et al: Melatonin-induced increased activity of the respiratory chain complexes I and IV can prevent mitochondrial damage induced by ruthenium red in vivo. J Pineal Res 2000; 28:242–248Google Scholar
441. Dabbeni-Sala F, Di Santo S, Franceschini D, et al: Melatonin protects against 6-OHDA-induced neurotoxicity in rats: a role for mitochondrial complex I activity. FASEB J 2001; 15:164–170Google Scholar
442. Fosslien E: Mitochondrial medicine–molecular pathology of defective oxidative phosphorylation. Ann Clin Lab Sci 2001; 31:25–67Google Scholar
443. Martin M, Macias M, Leon J, et al: Melatonin increases the activity of the oxidative phosphorylation enzymes and the production of ATP in rat brain and liver mitochondria. Int J Biochem Cell Biol 2002; 34:348–357Google Scholar
444. Okatani Y, Wakatsuki A, Reiter RJ: Melatonin protects hepatic mitochondrial respiratory chain activity in senescence-accelerated mice. J Pineal Res 2002; 32:143–148Google Scholar
445. Acuna-Castroviejo D, Escames G, Leon J, et al: Mitochondrial regulation by melatonin and its metabolites. Adv Exp Med Biol 2003; 527:549–557Google Scholar
446. Khaldy H, Escames G, León J, et al: Synergistic effects of melatonin and deprenyl against MPTP-induced mitochondrial damage and DA depletion. Neurobiol Aging 2003; 24:491–500Google Scholar
447. Scott AE, Cosma GN, Frank AA, et al: Disruption of mitochondrial respiration by melatonin in MCF-7 cells. Toxicol Appl Pharmacol 2001; 171:149–156Google Scholar
448. Kolker S, Ahlemeyer B, Krieglstein J, et al: Contribution of reactive oxygen species to 3-hydroxyglutarate neurotoxicity in primary neuronal cultures from chick embryo telencephalons. Pediatr Res 2001; 50:76–82Google Scholar
449. Park JW, Youn YC, Kwon OS, et al: Protective effect of serotonin on 6-hydroxydopamine- and dopamine-induced oxidative damage of brain mitochondria and synaptosomes and PC12 cells. Neurochem Int 2002; 40:223–233Google Scholar
450. Lee CS, Park SY, Ko HH, et al: Effect of change in cellular GSH levels on mitochondrial damage and cell viability loss due to mitomycin c in small cell lung cancer cells. Biochem Pharmacol 2004; 68:1857–1867Google Scholar
451. Vassilopoulos A, Papazafiri P: Attenuation of oxidative stress in HL-1 cardiomyocytes improves mitochondrial function and stabilizes Hif-1alpha. Free Radic Res 2005; 39:1273–1284Google Scholar
452. Weinreb O, Mandel S, Youdim MB: cDNA gene expression profile homology of antioxidants and their antiapoptotic and proapoptotic activities in human neuroblastoma cells. FASEB J 2003; 17:935–937Google Scholar
453. Weinreb O, Mandel S, Youdim MB: Gene and protein expression profiles of anti- and pro-apoptotic actions of dopamine, R-apomorphine, green tea polyphenol (-)-epigallocatechine-3-gallate, and melatonin. Ann N Y Acad Sci 2003; 993:351–361Google Scholar
454. Alvira D, Tajes M, Verdaguer E, et al: Inhibition of the cdk5/p25 fragment formation may explain the antiapoptotic effects of melatonin in an experimental model of Parkinson’s disease. J Pineal Res 2006; 40:251–258Google Scholar
455. Mayo JC, Sainz RM, Antolín I, et al: Ultrastructural confirmation of neuronal protection by melatonin against the neurotoxin 6-hydroxydopamine cell damage. Brain Res 1999; 818:221–227Google Scholar
456. Chetsawang J, Govitrapong P, Chetsawang B: Melatonin inhibits MPP + -induced caspase-mediated death pathway and DNA fragmentation factor-45 cleavage in SK-N-SH cultured cells. J Pineal Res 2007; 43:115–120 Google Scholar
457. Uz T, Giusti P, Franceschini D, et al: Protective effect of melatonin against hippocampal DNA damage induced by intraperitoneal administration of kainate to rats. Neuroscience 1996; 73:631–636Google Scholar
458. Chen ST, Chuang JI: The antioxidant melatonin reduces cortical neuronal death after intrastriatal injection of kainate in the rat. Exp Brain Res 1999; 124:241–247Google Scholar
459. Das A, Belagodu A, Reiter RJ, et al: Cytoprotective effects of melatonin on C6 astroglial cells exposed to glutamate excitotoxicity and oxidative stress. J Pineal Res 2008; 45:117–124Google Scholar
460. Feng Z, Zhang JT: Protective effect of melatonin on beta-amyloid-induced apoptosis in rat astroglioma C6 cells and its mechanism. Free Radic Biol Med 2004; 37:1790–1801Google Scholar
461. Chuang JI, Chen TH: Effect of melatonin on temporal changes of reactive oxygen species and glutathione after MPP + treatment in human astrocytoma U373MG cells. J Pineal Res 2004; 36:117–125 Google Scholar
462. Niles LP, Armstrong KJ, Rincón Castro LM, et al: Neural stem cells express melatonin receptors and neurotrophic factors: colocalization of the MT1 receptor with neuronal and glial markers. BMC Neurosci 2004; 28:5:41Google Scholar
463. Castro LM, Gallant M, Niles LP: Novel targets for valproic acid: up-regulation of melatonin receptors and neurotrophic factors in C6 glioma cells. J Neurochem 2005; 95:1227–1236Google Scholar
464. Kong X, Li X, Cai Z, et al: Melatonin regulates the viability and differentiation of rat midbrain neural stem cells. Cell Mol Neurobiol 2008; 28:569–579Google Scholar
465. Armstrong KJ, Niles LP: Induction of GDNF mRNA expression by melatonin in rat C6 glioma cells. Neuroreport 2002; 13:473–475Google Scholar
466. Imbesi M, Uz T, Dzitoyeva S, et al: Stimulatory effects of a melatonin receptor agonist, ramelteon, on BDNF in mouse cerebellar granule cells. Neurosci Lett 2008; 439:34–36Google Scholar
467. Atri A, Shaughnessy LW, Locascio JJ, et al: Long-term course and effectiveness of combination therapy in Alzheimer disease. Alzheimer Dis Assoc Disord 2008; 22:209–221Google Scholar
468. Tol J, Koopman M, Cats A, et al: Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med 2009; 360:563–572Google Scholar
469. Lauterbach EC, Victoroff J, Coburn KL, et al: Psychopharmacological neuroprotection in neurodegenerative disease: assessing the preclinical data. J Neuropsychiatry Clin Neurosci 2010; 22:8–18Google Scholar



