Double-Blind Treatment of Apathy in Patients with Poststroke Depression Using Nefiracetam
We have been studying apathy in patients with stroke since 1993. 2 The identification of apathy thus far has been based primarily on severity of scores on apathy rating scales. 2 We developed an apathy rating scale 2 based on a modified version of the scale proposed by Marin. 6 The Marin scale was modified to provide a more brief assessment. This modified version has been shown to be both reliable 7 and valid. 5 Using a cutoff score of 12 on our Apathy Scale, we found that 18 of 80 consecutive patients (22.5%) admitted to the hospital with an acute cerebrovascular lesion met this criterion for apathy. Of the 18 patients with apathy, half had associated major or minor depression. Poststroke apathy was also significantly associated with older age, cognitive impairment, and impairment in activities of daily living as well as lesions of the internal capsule. 2
Although there is a strong association of apathy with depression, the distinction between depression and apathy is not difficult because of the symptoms in emotional, cognitive, psychomotor, and autonomic functions are very different between the two disorders (e.g., apathy is characterized by loss of emotion while depression is characterized by intense sadness of emotion.) 8 Furthermore, depression distresses patients while apathy distresses caregivers.
In spite of a growing interest in apathy, published treatment studies have been limited to anecdotal case reports generally utilizing dopamine agonists or stimulant medications. 9 – 12 Nefiracetam is a novel pyrrolidone-type nootropic agent which has been demonstrated in animal studies to enhance aminergic, glutaminergic, and cholinergic neurotransmission by stimulating α=4, β=2 type neuronal nicotinic acetylcholine receptors, activating protein kinase C, and reducing magnesium block of the NMDA receptor. 13 – 19 In addition, nefiracetam increased brain-derived neurotrophic factor (BDNF) expression as well as regional blood flow and glucose utilization after sustained cerebral ischemia in rats. 20 , 21 This compound was first administered to humans in Japan as a potential treatment for poststroke cognitive impairment. Preliminary results published in Japanese language journals, however, showed an effect of treatment on outlook (i.e., optimism about the future) and interest (i.e., desire to undertake new activities), but no significant change in cognitive impairment. 22
The current study was therefore undertaken as part of a phase II trial of nefiracetam for treatment of poststroke depression 23 and, secondarily, apathy utilizing multisite enrollment and double-blind placebo-controlled methodology. This study thus represents a secondary analysis which was powered for assessment of depression, not for apathy. The hypothesis was that apathy, as well as depression would improve more following nefiracetam treatment, 900 mg/day, compared with placebo.
METHODS
Participants
A multisite (28 sites) trial of nefiracetam utilizing double-blind methodology was conducted from 1999–2001. All sites obtained institutional review board approval and all participants provided informed consent. Patients who lacked the capacity to consent based on comprehension deficit or severe cognitive impairment were excluded. This was based on clinical assessment by the treating neurologist. The study included 159 patients within 3 months of stroke who met DSM-IV diagnostic criteria for “depression due to stroke with major depressive-like episode.” Exclusion criteria included prior nonstroke-related brain injury, other psychiatric or neurological disease such as Alzheimer’s or Parkinson’s disease, existence of other life-threatening illness, comprehension deficit that would preclude a verbal interview, allergic response to nefiracetam, and taking any other psychotropic medications with the exception of small doses of benzodiazepines or related insomnia medications. Patients were randomly assigned to one of three treatment arms including 600 mg nefiracetam (n=55), 900 mg nefiracetam (n=48), or identical placebo (n=56), given in three identical 150 mg capsules twice daily. Patients were evaluated prior to entry into the study and followed-up at 4 weeks, 9 weeks, and 12 weeks. Scores on the Hamilton Depression Rating Scale (HAM-D) were the primary outcome variable. After 12 weeks, the study was completed and nefiracetam was discontinued. The patient disposition is shown in the flow chart in Figure 1 . This secondary analysis of intention-to-treat data included all of the 137 patients who had initial assessment and at least 4 weeks of follow-up.
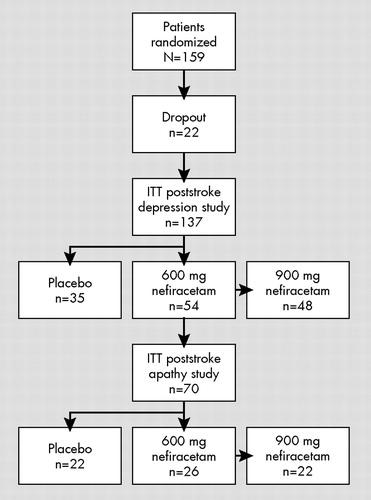
Chart includes treatment assignment and the number of patients who maintained treatment protocol for the first 4 weeks or more of the poststroke major depression study. Of the 159 enrolled, this group of 137 in the depression study and 70 in the apathy study constituted our intention-to-treat (ITT) sample.
Diagnosis
All patients included in the study were diagnosed with apathy using the diagnostic criteria suggested by Starkstein et al. 5 Based on the interviewer rated findings from the Apathy Scale (clinician version), all patients with a diagnosis of apathy had loss of motivation (a score of 2 or 3 on item 7 [Are you inspired to accomplish things?]) and at least one symptom indicating decreased function from each of the three symptom clusters: emotion (a score of 2 or 3 on items 10 [Are you indifferent to things?] or 13 [Are your emotions gone?]); behavior (a score of 2 or 3 on items 4 [Do you have energy to do things?] or 9 [Do you need prodding to get going?]); or cognition (a score of 2 or 3 on items 1 [Are you interested in learning?] or 2 [Do activities interest you?]).
The modified Apathy Scale is an interviewer-rated, 14-item scale that has been shown to be reliable and valid in the stroke population. 2 Scores range from 0 to 42 with higher scores indicating greater severity. The interviewers’ ratings represented a clinical judgment based on information provided by the patient and a family member.
Psychopathological Evaluation
In addition to the Apathy Scale, all patients were administered the modified Present State Examination, 24 a semistructured mental status exam designed to allow DSM-IV-TR 25 diagnoses of depression due to stroke with major depressive-like episode, minor depression (DSM-IV-TR, research criteria), or anxiety disorder due to stroke with generalized anxiety. Patients were also administered the HAM-D (17-item) 26 and the Beck Depression Inventory (BDI). 27 Each of these instruments has been shown to be reliable and valid in assessing patients with stroke. 28 , 29
Prior to beginning the study and halfway through the study (to prevent rater drift), all study raters were trained in the use of all of these instruments. All raters were shown 5 videos of patient interviews and asked to rate their responses. An interview rater was not permitted to participate in the study until their interrater reliability exceeded 80% agreement based on intraclass correlation with the ratings made by an experienced rater (i.e., RGR).
Neurological and Cognitive Examinations
Patients were administered the Modified Mini-Mental State test (3MS) for assessment of cognitive impairment. 30 Scores range from 0 to 100 with lower scores indicating greater impairment. The Functional Independence Measure 31 assessed activities of daily living in the domains of self-care, mobility, communications, sphincter control, locomotion, and social cognition. Scores range from 0 to 100 with lower scores indicating greater impairment. The NIH Stroke Scale 32 measured severity of neurological impairment in level of consciousness, visual fields, facial palsy, motor function, ataxia, sensory impairment, language, dysarthria, extinction, and distal motor function. Higher scores indicate greater severity of stroke-related impairment. Each of these scales has been demonstrated to be reliable and valid in a stroke population. 31 , 32
Statistical Analysis
The data were compared across groups using means, standard deviations, and analysis of variance. The intention-to-treat population of 137 had at least 4 weeks of data. Longitudinal data were analyzed using a repeated measures analysis of variance. Missing data points were estimated using last observation carried forward. Frequency distributions were evaluated using chi-squared or Fisher’s exact test. Statistical significance was based on a two-tailed p value less than 0.05.
RESULTS
Background Characteristics
Figure 1 shows patient disposition. A total of 159 patients were randomized and 158 given placebo or nefiracetam (600 mg or 900 mg). A total of 44 patients dropped out and 115 completed the 12-week protocol while 137 represented our intention-to-treat population who had 4 or more weeks of treatment. Of the 22 patients who dropped out prior to completing 4 weeks, three (13.6%) met criteria for apathy compared with 70 of 137 completers (51.1%) who met criteria for apathy (Fisher Test, two-tailed, p=0.001). The background characteristics and impairment scores of the apathetic and nonapathetic patients are summarized in Table 1 . There were no statistically significant differences in the background characteristics or mean scores on the HAM-D, or on the neurological and cognitive impairment measures. The background characteristics of the 22 dropouts compared to the 137 intention-to-treat patients showed no significant differences in age, gender, ethnicity, handedness, NIH Stroke Scale scores, cortical lesions, subcortical lesions, HAM-D scores, or Apathy Scale scores.
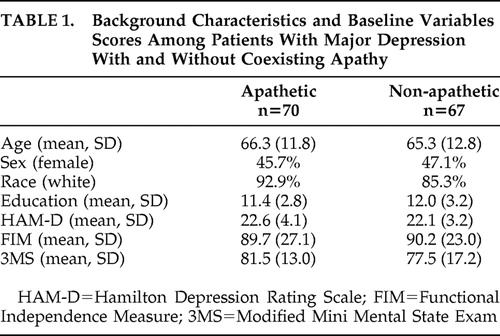 |
The background characteristics and impairment scores of the patients diagnosed with apathy, divided into the three medication treatment arms, are shown in Table 2 . There were no statistically significant differences in any of the demographic variables. Similarly there were no statistically significant differences in the HAM-D, Functional Independence Measure, 3MS, or Apathy Scales among the three groups. The patients all had moderately severe depression and apathy, but only mild-to-moderate severity of impairment in cognitive function and activities of daily living.
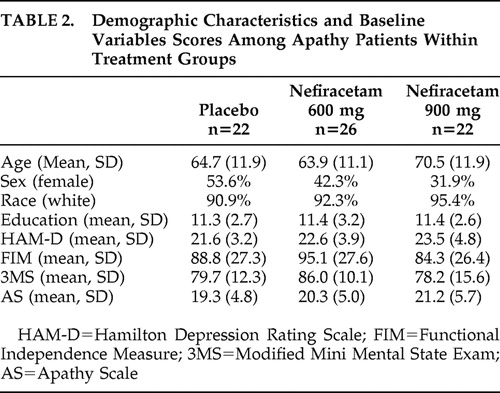 |
There were no significant differences among the three treatment groups in severity of stroke based on the NIH Stroke Scale, or the frequency of lesions affecting the frontal cortex, basal ganglia, thalamus, or internal capsule.
Drug-Related Side Effects
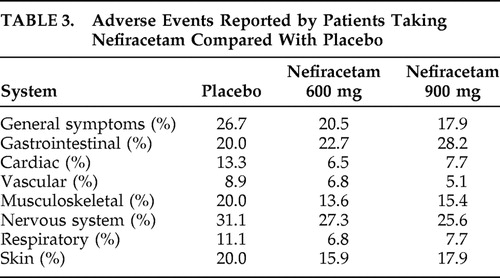
The frequency of adverse events comparing 900 or 600 mg of nefiracetam or placebo is shown on Table 3 . There were no significant differences between the groups in the frequency of adverse events.
 |
Intention-to-Treat Analysis
Apathy scores for the three treatment groups over the course of the treatment trial are shown in Figure 2 , panel A. Repeated measures analysis of variance (ANOVA) of Apathy Scale scores showed both a significant effect for time (F=9.4, df=3, 65, p=0.0001) and a significant time × treatment group interaction (F=2.3, df=6, 128, p=0.050). Patients receiving 900 mg/day of nefiracetam showed a significantly greater decrease in Apathy Scale scores during the 12-week trial compared to patients receiving placebo (time × treatment group interaction: F=4.0, df=3, 65, p=0.01). The time by treatment group interaction for 600 mg/day versus placebo was nonsignificant (F=1.3, df=3, 65, p=0.29). The time by treatment interaction for 900 mg versus 600 mg was nonsignificant (F=1.45, df=3, 65, p=0.23). The absolute risk reduction for 900 mg nefiracetam versus placebo was 0.18 (95% CI 0.02–0.34) while 600 mg nefiracetam versus placebo was 0.04 (95% CI=0.04–0.11).
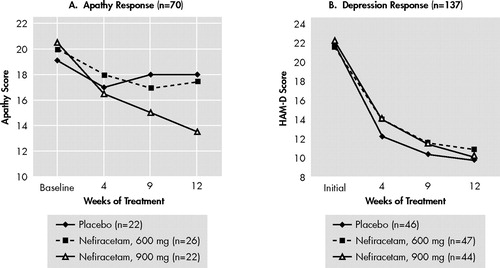
Patients completing 4 or more weeks of treatment as measured by the Apathy Scale (A) and the 137 patients included in the poststroke major depression trial (B). Patients who received 900 mg/day of nefiracetam had significantly greater reduction in Apathy Scale scores over 12 weeks than patients treated with placebo or 600 mg nefiracetam (time × treatment interaction; F=2.3, df=6, 128, p=0.050). There was not a significant time × treatment interaction using the Hamilton Depression Rating Scale. Note that all depression groups improved without specific response to Nefiracetam compared with placebo.
Furthermore, considering remission as a 75% decrease in apathy scale scores, four of 22 patients in the 900 mg nefiracetam group, one of 26 patients in the 600 mg nefiracetam group and none of the 22 patients in the placebo group had remission of symptoms (χ 2 =6.7, df=2, p=0.031). Thus, apathy remission was significantly more frequent in the 900 mg nefiracetam group compared with the placebo and 600 mg nefiracetam groups.
In the assessment of depression, a repeated measure analysis of HAM-D scores did not show a significant time by treatment group interaction, suggesting that the differential treatment effect on apathy scores was not simply due to an improvement in depression scores ( Figure 2 , panel B). In addition, we compared change on HAM-D and Apathy Scale scores (i.e., initial minus 12-week scores). There was a significant difference between the 900 mg, 600 mg, or placebo groups in change of Apathy Scale scores (i.e., apathy 900 mg group =7.5±8.5; 600 mg group =3.5±6.6; placebo group =2.0±7.0, p=0.038). This was not the case for change in HAM-D scores (i.e., 900 mg group =14.0±8.2, 600 mg group = 12.8±7.1, placebo group =12.7±7.9, ANOVA, p=0.82).
Since apathy has manifestations in cognition as well as emotion, we examined correlations between the change in Apathy Scale scores from beginning to end of treatment and HAM-D or 3MS scores (HAM-D score, Spearman ρ=0.28, p=0.0018 and 3MS (cognition) score (Spearman ρ=−0.12, p=0.15). Although this finding does not support the hypothesis that apathy effects cognition, this is a global score and some aspects of cognition may have improved with Apathy Scale scores.
Imaging Analysis
We examined treatment response in patients with subcortical compared to cortical involvement, 33 (i.e., cortical: 900 mg, n=10; 600 mg, n=14; placebo, n=13; and subcortical: 900 mg n=4; 600 mg, n=3; placebo, n=7) and there was no significant treatment × lesion location × time interaction.
DISCUSSION
This randomized, double-blind study demonstrated that, among patients who met diagnostic criteria for both apathy and major depression, 900 mg of nefiracetam administered over 12 weeks of treatment significantly improved apathy scores compared with patients who received placebo or a lower dose (600 mg) of nefiracetam. On the other hand, 900 mg of nefiracetam was not different from placebo as a treatment for depression, suggesting that the differential effect of active versus placebo effect on apathy was different than the active versus placebo effect on depression. Finally, nefiracetam and placebo had few similar side effects.
This is the first trial, of which we are aware, that has demonstrated a significant treatment effect among patients with a diagnosis of apathy using double-blind, placebo controlled methodology. The first issue which must be addressed, however, is whether this response is simply due to an improvement in depressive symptoms. First, clinicians can readily distinguish between apathy and depression because depression involves feelings of sadness, sometimes with agitation, decreased sleep and appetite, hopelessness, self-blame, and suicidal thoughts. Apathy is characterized by lack of motivation and blunted emotional responses without the former symptoms. Second, the strongest argument for this being a specific effect on apathy is that active versus placebo treatment showed no difference on depressive symptoms, but a very significant differential effect on apathy symptoms. Thus, the treatment effect on apathy cannot be explained based on the treatment effect on depression.
There is a growing literature consisting of case reports and small series of patients who were treated for apathy with a variety of psychoactive agents. 4 Psychostimulants and dopaminergic agonists may modestly improve arousal and speed of information processing, reduce distractibility, and improve some aspects of motivation and executive function. 34 , 35 However, the magnitude and temporal course of their therapeutic effect is still controversial. 36 Amantadine, a drug with pharmacologic effects on dopaminergic, cholinergic and NMDA receptors, could also have some efficacy in the treatment of motivational deficits. 37 – 39 Finally, there is some empirical evidence that cholinesterase inhibitors such as donepezil may improve motivation and general well being of patients with traumatic brain injury 40 – 42 and may improve apathetic symptoms among patients with dementia. 43 Thus, other drugs besides nefiracetam may be effective treatments for poststroke apathy.
Although the mechanism of apathy is unknown, Kalivas et al. 44 has postulated that the rostral cingulate, nucleus accumbens, ventral pallidum, and ventral tegmental areas constitute a core circuit in which motivational state is dependent upon the pattern of information in the core circuit. Limbic structures such as the amygdala, hippocampus, and frontal cortex modulate the core circuit based on the motivational and emotional significance of the internal and external input to these limbic structures. This hypothesis is consistent with the findings of Okada et al., 45 using xenon inhalation methods, who found that 20 patients with apathy following stroke had significantly reduced regional cerebral blood flow in the right dorsal lateral frontal and left frontotemporal regions compared with 20 patients without apathy. In a more recent study of 29 patients with apathy and subcortical stroke, the same group of investigators reported a significantly prolonged latency and decreased amplitude of the P3-Novelty component of the auditory event-related potential in the frontal cortex. 46 It is plausible that hypoactivity in frontal and temporal lobe regions, and therefore reduced input to the core circuit, may be reversed by the enhanced aminergic, glutaminergic, and cholinergic neurotransmission produced by nefiracetam. Other mechanisms could, of course, be proposed.
Finally, the limitations of the study should be acknowledged. First, this was a secondary analysis and the study was primarily designed to assess response of poststroke depression to nefiracetam. Second, of the 159 patients randomized to the three treatment arms, 22 patients (13.8%) dropped out during the first month of the trial. Although there was a significantly lower frequency of apathy among dropouts than continued participants, there were no significant differences in demographic or baseline impairment variables between patients who remained in the study and those who dropped out. Although it is unlikely that this influenced our findings, attrition-related bias cannot be ruled out. Third, all patients enrolled in the study had major depression as well as apathy. Based on prior literature, about half of all stroke patients with clinically significant apathy would be expected to have depression. 2 We do not know, however, whether the response to nefiracetam was applicable only to patients with apathy plus depression or whether these findings apply to patients with apathy without associated depressive disorder. Fourth, we lacked sufficient power to examine whether apathy was associated with specific impairments such as cognitive function or specific lesion location. Finally, because this was a 12-week treatment trial without prolonged follow-up, we do not know whether the improvement in apathy symptoms continued after discontinuation of the drug.
In conclusion, apathy has received increasing attention because of its effect on emotion, behavior, and cognitive function. The current study is the first randomized double-blind treatment trial to be conducted among a large group of stroke patients with coexistent apathy and depression, and our results suggest that nefiracetam may be an effective treatment for this clinically important condition. Further studies in patients with apathy without associated depression are needed to determine the specificity of nefiracetam as treatment of apathy and whether treatment of apathy significantly improves long-term outcome and recovery.
1. Marin RS: Apathy: a neuropsychiatric syndrome. J Neuropsychiatry Clin Neurosci 1991; 3:243–254Google Scholar
2. Starkstein SE, Fedoroff JP, Price TR, et al: Apathy following cerebrovascular lesions. Stroke 1993; 24:1625–1630Google Scholar
3. Levy R, Dubois B: Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cereb Cortex 2006; 16:916–928Google Scholar
4. Marin RA, Chakravorty S: Disorders of diminished motivation, in Textbook of Traumatic Brain Injury. Edited by Silver JM, McAllister TW, Yudofsky SC. Arlington, Va, American Psychiatric Publishing, 2005, pp 337–352Google Scholar
5. Starkstein SE, Petracca G, Chemerinski E, et al: Syndromic validity of apathy in Alzheimer’s disease. Am J Psychiatry 2001; 158:872–877Google Scholar
6. Marin RS: Reliability and validity of the apathy evaluation scale. Psychiatry Res 1991; 38:143–162Google Scholar
7. Starkstein SE, Mayberg HS, Preziosi TJ, et al: Reliability, validity and clinical correlates of apathy in Parkinson’s disease. J Neuropsychiatr Clin Neurosci 1992; 4:134–139Google Scholar
8. Marin RS, Firinciogullari S, Biedrzicky RC: The sources of convergence between measures of apathy and depression. J Affect Disord 1993; 28:117–124Google Scholar
9. Watanabe A, Matsuo K, Kato N, et al: Cerebrovascular response to cognitive tasks and hyperventilation measured by multi-channel near-infrared spectroscopy. J Neuropsychiatry Clin Neurosci 2003; 15:442–449Google Scholar
10. Van Reekum R, Bayley M, Garner S, et al: N of 1 study: amantadine for the amotivational syndrome in a patient with traumatic brain injury. Brain Inj 1995; 9:49–53Google Scholar
11. Newburn G, Newburn D: Selegiline in the management of apathy following traumatic brain injury. Brain Inj 2005; 19:149–154Google Scholar
12. Kraus MF: Neuropsychiatric sequelae of stroke and traumatic brain injury: the role of psychostimulants. Int J Psychiatry Med 1995; 25:39–51Google Scholar
13. Tsuchiya Y, Takahashi Y, Jindo T, et al: Comprehensive evaluation of canine renal papillary necrosis induced by nefiracetam, a neurotransmission enhancer. Eur J Pharmacol 2003; 475:119–128Google Scholar
14. Nishizaki T, Matsuoka T, Nomura T, et al: Nefiracetam modulates acetylcholine receptor currents via two different signal transduction pathways. Mol Pharmacol 1998; 53:1–5Google Scholar
15. Kitano Y, Komiyama C, Makino M, et al: Effects of nefiracetam, a novel pyrrolidone-type nootropic agent, on the amygdala-kindled seizures in rats. Epilepsia 2005; 46:1561–1568Google Scholar
16. Moriguchi S, Marszalec W, Zhao X, et al: Potentiation of N-methyl-D-aspartate-induced currents by the nootropic drug nefiracetam in rat cortical neurons. J Pharmacol Exp Ther 2003; 307:160–167Google Scholar
17. Narahashi T, Moriguchi S, Zhao X, et al: Mechanisms of action of cognitive enhancers on neuroreceptors. Biol Pharm Bull 2004; 27:1701–1706Google Scholar
18. Zhao X, Yeh JZ, Narahashi T: Post-stroke dementia: nootropic drug modulation of neuronal nicotinic acetylcholine receptors. Ann NY Acad Sci 2001; 939:179–186Google Scholar
19. Moriguchi S, Shioda N, Maejima H, et al: Nefiracetam potentiates N-methyl-D-aspartate (NMDA) receptor function via protein kinase C activation and reduces magnesium block of NMDA receptor. Mol Pharmacol 2007; 71:580–587Google Scholar
20. Ando T, Takagi N, Takagi K, et al: Effects of nefiracetam on the levels of brain-derived neurotrophic factor and synapsin I MRNA and protein in the hippocampus of microsphere-embolized rats. Eur J Pharmacol 2005; 507(1–3):49–56Google Scholar
21. Jin J, Watabe S, Yamamoto T: Nefiracetam improves the impairment of local cerebral blood flow and glucose utilization after chronic focal cerebral ischemia in rats. Pharmacology 2002; 64:119–125Google Scholar
22. Otomo E, Kogure K, Hirai S, et al: [Clinical utility of DM-9384 (Nefiracetam) in patients with aftereffect following cerebrovascular disorders: a comparative double-blind study with idebenone]. Rinsho Iyaku (J Clin Ther Med) 1994; 10:1871–1918 (Japanese)Google Scholar
23. Robinson RG, Jorge RE, Moser DJ, et al: Escitalopram and problem solving therapy for prevention of poststroke depression: a randomized trial. JAMA 2008; 299:2391–2400Google Scholar
24. Wing JK, Cooper JE, Sartorius N. The Measurement and Classification of Psychiatric Symptoms: An Instructional Manual for the PSE and CATEGO Programs. New York, Cambridge University Press, 1974Google Scholar
25. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorder-DSM-IV-TR. Washington, DC, American Psychiatric Association, 2000Google Scholar
26. Hamilton MA: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Google Scholar
27. Beck AT, Steer RA: Beck Depression Inventory manual. San Antonio, The Psychological Corporation, 1987Google Scholar
28. Robinson RG, Starr LB, Kubos KL, et al: A two-year longitudinal study of post-stroke mood disorders: findings during the initial evaluation. Stroke 1983; 14:736–744Google Scholar
29. House A, Dennis M, Warlow C, et al: Mood disorders after stroke and their relation to lesion location. A CT scan study Brain 1990; 113:1113–1130Google Scholar
30. Teng EL, Chui HC: The modified mini-mental state (3MS) examination. J Clin Psychiatry 1987; 48:314–318Google Scholar
31. Forer S, Granger CV: Functional Independence Measure. Buffalo, NY, The Buffalo General Hospital State University of New York at Buffalo, 1987Google Scholar
32. Kunitz SC, Gross CR, Heyman A, et al: The pilot stroke data bank: definition, design, and data. Stroke 1984; 15:740–746Google Scholar
33. Levy R, Dubois B: Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cereb Cortex 2006; 16:916–928Google Scholar
34. Plenger PM, Dixon CE, Castillo RM, et al: Subacute methylphenidate treatment for moderate to moderately severe traumatic brain injury: a preliminary double-blind placebo-controlled study. Arch Phys Med Rehabil 1996; 77:536–540Google Scholar
35. Zafonte RD, Lexell J, Cullen N: Possible applications for dopaminergic agents following traumatic brain injury, part 2. J Head Trauma Rehabil 2001; 16:112–116Google Scholar
36. Whyte J, Vaccaro M, Grieb-Neff P, et al: Psychostimulant use in the rehabilitation of individuals with traumatic brain injury. J Head Trauma Rehabil 2002; 17:284–299Google Scholar
37. Kraus MF, Maki P: The combined use of amantadine and L-dopa/carbidopa in the treatment of chronic brain injury. Brain Inj 1997; 11:455–460Google Scholar
38. Kraus MF, Maki PM: Effect of amantadine hydrochloride on symptoms of frontal lobe dysfunction in brain injury: case studies and review. J Neuropsychiatry Clin Neurosci 1997; 9:222–230Google Scholar
39. Meythaler JM, Brunner RC, Johnson A, et al: Amantadine to improve neurorecovery in traumatic brain injury-associated diffuse axonal injury: a pilot double-blind randomized trial. J Head Trauma Rehabil 2002; 17:300–313Google Scholar
40. Arciniegas D, Adler L, Topkoff J, et al: Attention and memory dysfunction after traumatic brain injury: cholinergic mechanisms, sensory gating, and a hypothesis for further investigation. Brain Inj 1999; 13:1–13Google Scholar
41. Freo U, Pizzolato G, Dam M, et al: A short review of cognitive and functional neuroimaging studies of cholinergic drugs: implications for therapeutic potentials. J Neural Transm 2002; 109:857–870Google Scholar
42. Arciniegas DB: The cholinergic hypothesis of cognitive impairment caused by traumatic brain injury. Curr Psychiatry Rep. Oct 2003; 5:391–399Google Scholar
43. Cummings JL, Koumaras B, Chen M, et al: Effects of rivastigmine treatment on the neuropsychiatric and behavioral disturbances of nursing home residents with moderate to severe probable Alzheimer’s disease: a 26-week, multicenter, open-label study. Am J Geriatr Pharmacother 2005; 3:137–148Google Scholar
44. Kalivas PW, Volkow N, Seamans J: Unmanageable motivation in addiction: a pathology in prefrontal-accumbens glutamate transmission. Neuron 2005; 45:647–650Google Scholar
45. Okada K, Kobayashi S, Yamagata S, et al: Poststroke apathy and regional cerebral blood flow. Stroke 1997; 28:2437–2441Google Scholar
46. Yamagata S, Yamaguchi S, Kobayashi S: Impaired novelty processing in apathy after subcortical stroke. Stroke 2004; 35:1935–1940Google Scholar



