Functional Neurological (Conversion) Disorder: A Core Neuropsychiatric Disorder
Foundational to any definition of neuropsychiatry is the indelible inseparability of brain and thought, of mind and body, and of mental and physical.
—Stuart C. Yudofsky and Robert E. Hales (1)
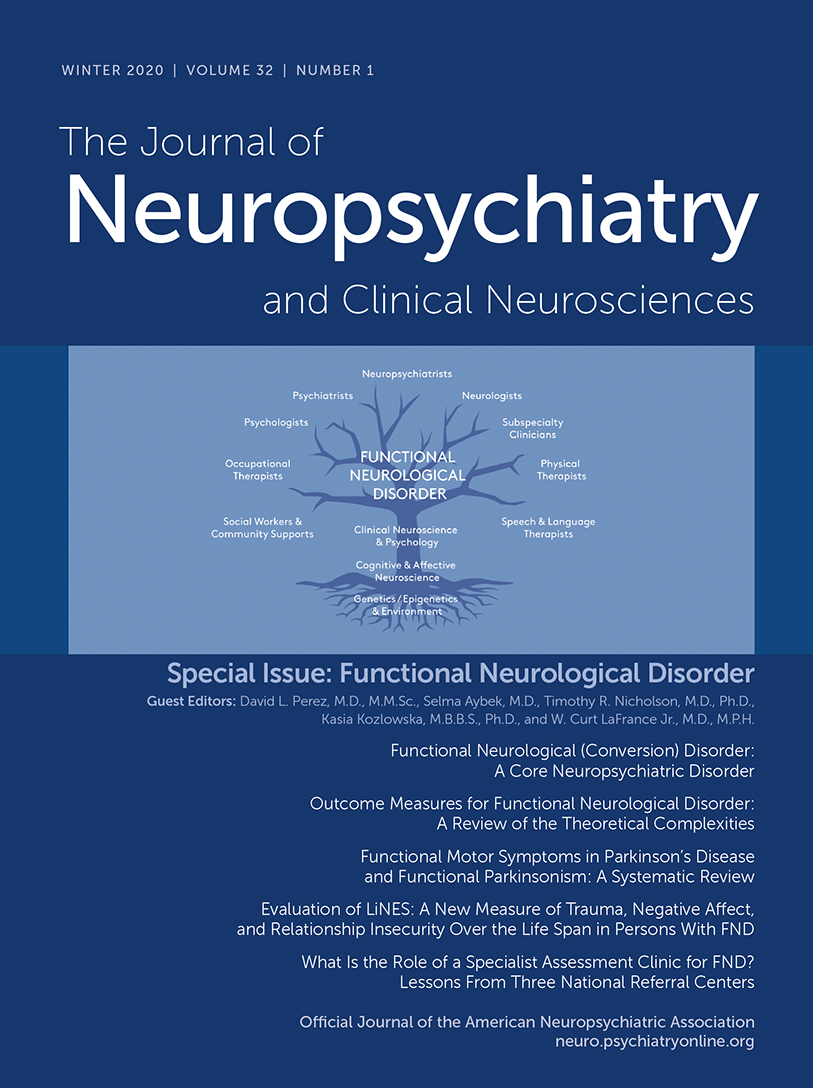
Functional neurological disorder (FND), also known as conversion disorder, constitutes individuals with neurological symptoms precipitated and/or perpetuated by maladaptive cognitive, affective, behavioral, psychological, and perceptual processes. As such, FND is a core neuropsychiatric disorder that exists at the intersection of the mind and brain. Furthermore, FND challenges the artificial divide between physical and mental health and can benefit greatly from an interdisciplinary approach across the clinical neurosciences (2, 3). A figurative conceptualization of this interdisciplinary approach to FND, as discussed in this special issue of the Journal, is featured on the cover of this issue.
FND is among the most common conditions encountered by neurologists and neuropsychiatrists today (4) and is often misidentified as “medical mysteries” in human interest stories (5). Importantly, the neuropsychiatric perspective that incorporates biopsychosocial aspects at the individual level, including consideration of community and spiritual aspects when relevant (3), is key for treatment and research for this complex condition.
For this special issue of the Journal, an international group of guest coeditors and authors organized to detail the depth and breadth of advancement in the field of FND, while also identifying areas of need. Several articles advance our understanding of the phenomenology of FND, including the development of a conceptual model for acute functional paralysis (6) (a common stroke mimic) and the intersection of Parkinson’s disease and functional movement disorders (7). Other articles identify predisposing vulnerabilities and perpetuating factors for FND (8) and characterize roles for locus of control (frame of reference) (9), impaired action inhibition (10), and altered emotional reactivity (11) among persons with FND. A new questionnaire for the concurrent assessment of adverse life events, negative emotions, and attachment styles among individuals with FND across the lifespan is also introduced (12). Additionally, another article integrates psychological and neurobiological models in the service of bridging the gap between the historical conversion model and modern systems-level neuroscience insights into FND (13).
Reflecting increasing clinical and research interest in FND as well as the need for a larger repertoire of evidenced-based therapeutics, several articles present new findings on the treatment of FND. A necessary prerequisite to evidence-based treatments and effective clinical services is the development of a core battery of accepted and widely used outcome measures. Toward that end, the international FND Core Outcome Measures group—the first large-scale international collaboration in the field, comprising 40 members from 14 countries and including patient group representation—discusses the complexities of standardizing outcomes for FND and outlines a research agenda to optimize outcome measurement (14). Given the high prevalence of FND and the need to promote integrated care models for this patient population, one article describes insights gained from established subspecialty FND clinics in the United Kingdom, Switzerland, and Canada (15). Although conventional cognitive-behavioral therapy (CBT) and CBT-informed psychotherapies are emerging evidence-based treatments for FND, this issue also includes an article demonstrating the feasibility and effectiveness of providing care to persons with FND in an outpatient behavioral medicine clinic (16). Treatment engagement in psychotherapy is another challenge, and evidence suggesting a role for motivational interviewing in the management of persons with FND is also included in this collection of articles (17). Similarly, while motor retraining using physical therapy is a mainstay of treatment for functional motor symptoms on the basis of available clinical trial evidence, the feasibility of implementing physical therapy for motor FND in the outpatient setting in the United States is reported in one of the studies presented (18). Regarding the development of novel treatment approaches, research opportunities to investigate potential roles for placebo (19) and virtual reality-delivered mirror visual feedback (20) in the treatment of FND are also addressed.
Although there remain areas of importance in the conceptualization, assessment, and management of FND not addressed in this issue, the limited presentation and discussion of pathophysiologic models and evidence-based treatments for pediatric FND is a noteworthy shortcoming of this collection. It is the sincere hope of our editorial group that the science presented in this issue will catalyze additional international collaborations on FND across the lifespan. The guest editors and authors, along with many in the wider research community, are dedicated to bettering the lives of those living with FND and to ensuring that this condition can be detected early, diagnosed accurately, and treated effectively.
While the condition presently referred to as FND has been described in the medical literature for centuries, its neuroscientific study and evidence-informed treatment remain at the early stages of development, particularly when compared with other equally common neuropsychiatric conditions. In partnership with persons with FND, their families, and other stakeholders, the clinical neuroscience community has great opportunities to advance the care and study of FND. We call upon clinicians and scientists eager to work impactfully at the brain-mind interface to join us in the renaissance in FND using a neuropsychiatric perspective.
1 : Neuropsychiatry and the future of psychiatry and neurology. Am J Psychiatry 2002; 159:1261–1264Crossref, Medline, Google Scholar
2 : Bridging the great divide: what can neurology learn from psychiatry? J Neuropsychiatry Clin Neurosci 2018; 30:271–278Link, Google Scholar
3 : Treatment of nonepileptic seizures. Epilepsy Behav 2002; 3(Suppl):19–23Crossref, Medline, Google Scholar
4 : Symptoms “unexplained by organic disease” in 1144 new neurology out-patients: how often does the diagnosis change at follow-up? Brain 2009; 132:2878–2888Crossref, Medline, Google Scholar
5 : Hiding in plain sight: functional neurological disorders in the news. J Neuropsychiatry Clin Neurosci 2019; 31:361–367Link, Google Scholar
6 : Functional stroke symptoms: a narrative review and conceptual model. J Neuropsychiatry Clin Neurosci 2020; 32:14–23Abstract, Google Scholar
7 : Functional motor symptoms in Parkinson’s disease and functional Parkinsonism: a systematic review. J Neuropsychiatry Clin Neurosci 2020; 32:4–13Abstract, Google Scholar
8 : Predisposing risk factors for functional limb weakness: a case-control study. J Neuropsychiatry Clin Neurosci 2020; 32:50–57Link, Google Scholar
9 : Internal versus external frame of reference in functional movement disorders. J Neuropsychiatry Clin Neurosci 2020; 32:67–72Link, Google Scholar
10 : Impaired action control in patients with functional movement disorders. J Neuropsychiatry Clin Neurosci 2020; 32:73–78Abstract, Google Scholar
11 : Emotional reactivity as a vulnerability for psychogenic nonepileptic seizures? Responses while reliving specific emotions. J Neuropsychiatry Clin Neurosci 2020; 32:95–100Link, Google Scholar
12 : Evaluation of LiNES: a new measure of trauma, negative affect, and relationship insecurity over the life span in persons with FND. J Neuropsychiatry Clin Neurosci 2020; 32:43–49Abstract, Google Scholar
13 : What does neuroscience tell us about the conversion model of functional neurological disorders? J Neuropsychiatry Clin Neurosci 2020; 32:24–32Link, Google Scholar
14 : Outcome measures for functional neurological disorder: a review of the theoretical complexities. J Neuropsychiatry Clin Neurosci 2020; 32:33–42Abstract, Google Scholar
15 : What is the role of a specialist assessment clinic for FND? lessons from three national referral centers. J Neuropsychiatry Clin Neurosci 2020; 32:79–84Abstract, Google Scholar
16 : Outpatient CBT for motor functional neurological disorder and other neuropsychiatric conditions: a retrospective case comparison. J Neuropsychiatry Clin Neurosci 2020; 32:58–66Abstract, Google Scholar
17 : Motivational interviewing techniques to improve psychotherapy adherence and outcomes for patients with psychogenic nonepileptic seizures. J Neuropsychiatry Clin Neurosci (Epub ahead of print August 30, 2019)Google Scholar
18 : Outpatient physical therapy for functional neurological disorder: a preliminary feasibility and naturalistic outcome study in a U.S. cohort. J Neuropsychiatry Clin Neurosci 2020; 32:85–89Abstract, Google Scholar
19 : Leveraging the shared neurobiology of placebo effects and functional neurological disorder: a call for research. J Neuropsychiatry Clin Neurosci 2020; 32:101–104Link, Google Scholar
20 : Virtual reality-delivered mirror visual feedback and exposure therapy for FND: a midpoint report of a randomized controlled feasibility study. J Neuropsychiatry Clin Neurosci 2020; 32:90–94Abstract, Google Scholar