Relationship Between MRI Findings and Prognosis for Patients With General Paresis
Abstract
MRI was performed in 7 patients with general paresis before or at a very early stage of treatment. A large dose of antibiotics, mainly penicillin, was given to all patients, and the effects of treatment, the patients' outcome, and MRI findings were investigated. Three of the 7 patients had MRI findings of atrophy of the medial temporal lobe including the hippocampus. In the medial temporal lobe atrophy group, a personality change or general dementia remained even after the treatment was completed, and outcome in social functioning was poor. Medial temporal lobe atrophy may be a poor prognostic sign in general paresis.
Although general paresis is quite rare nowadays, we still cannot clinically ignore this disease, as reports from the United States point out that the number of patients with neurosyphilis as well as acquired immunodeficiency syndrome (AIDS) is now increasing.1,2 As neurosyphilis advances, serious dementia or a personality change remains, but it is considered to be “treatable” dementia3,4 because it can be treated with antibiotics, mainly penicillin.2,5,6 Early diagnosis and treatment are therefore most important.
We scarcely find any descriptions of neuroimages of neurosyphilis, including general paresis, in recent textbooks.2,7 This may be because neuroimages of neurosyphilis generally are not very specific and are of little value in making a diagnosis. We performed magnetic resonance imaging (MRI) to understand the relationship between MRI findings and prognosis for patients with general paresis.
METHODS
Subjects
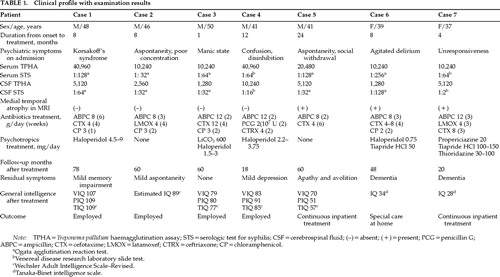
The subjects were 7 patients (5 men and 2 women) who were admitted to the psychiatric ward of Chiba University Hospital from 1990 to 1997. They were from 37 years to 50 years of age, and the average age was 43.1 years. Table 1 shows their clinical characteristics. Informed consent was obtained from them and/or their close relatives for the tests and treatment. Through clinical examinations, we found that most of their symptoms were mental disorders with few neurological symptoms. Their serum Treponema pallidum hemagglutination (TPHA) was highly positive, cerebrospinal fluid (CSF) serological test for syphilis (STS) was positive, cell counts of CSF were increasing, and their protein levels were going up. Considering these findings, all of these patients were diagnosed as having general paresis. The results of examinations for human immunodeficiency virus–type 1 (HIV) infection were negative. Other laboratory tests, including serum thyroid hormonal levels, serum vitamin B1 level, immunoglobulin G antibody titer for herpes simplex virus type 1 in the CSF, and others, were all negative.
MRI
We performed MRI in all of these cases before or at a very early stage of the treatment. CT imaging was also done at the same time in all cases. In the 4 cases out of the 7 that were followed up for more than 3 years, CT or MRI was repeated. We used a 1.5-tesla MRI unit (Signa or Signa Advantage System, General Electric). We obtained axial T2-weighted and proton density–weighted images and coronal T1-weighted images. No contrast MR imaging was performed in the MRI protocol.
A large dose of antibiotics, mainly penicillin, was given to all the patients, and we investigated the effects of treatment, the patients' outcome, and MRI findings.
RESULTS
MRI Findings
A summary of our MRI findings for the 7 cases is as follows (illustrated in Figures 1 and 2):
| 1. | Group A: Four patients (cases 1 to 4) had normal MRI or slight cerebral atrophy. | ||||
| 2. | Group B: Three patients (cases 5 to 7) had atrophy of the medial temporal lobe, including the hippocampus. Cerebral atrophy, mainly in the frontal lobes, and dilation of the third and lateral ventricles were also recognized, and in each case dilation of ventricles was more conspicuous than cerebral atrophy. | ||||
| 3. | One patient (Case 5) had high-intensity areas around the posterior horns of the lateral ventricles, but we did not find other abnormal signal areas. | ||||
Relationship Between MRI Findings Before Treatment and Patient's Outcome
Investigating the relationship between our MRI findings before treatment and the patient's outcome (Table 1), we found that in Group A, symptoms improved very well and outcome in social functioning was very good. On the other hand, Group B had benefited somewhat from the treatment, but a personality change or general dementia remained even after the treatment finished, and their outcome in social functioning was poor.
Furthermore, we reexamined 4 of the 7 patients (cases 1, 2, 3, and 6) at 3 to 6 years after the end of the treatment, and in 3 of them we did not recognize any worsening of atrophy on CT or MRI examinations. The remaining patient (Case 2) had only a very slight worsening of atrophy.
DISCUSSION
The most important MRI finding in this study is atrophy of the medial temporal lobe including the hippocampus in 3 of the 7 cases. MRI findings in patients with neurosyphilis have been reported. Zifko et al.8 performed MRI in 4 HIV-negative patients with general paresis. The outcome for social functioning of 3 of these patients was quite poor, and the personality changes and dementia remained. They had subcortical gliosis as well as cerebral atrophy mainly of the frontal lobes, and 1 of the 3 also had hippocampal atrophy. Furthermore, 1 year later they found in 1 of the 3 patients signs suggesting ferritin deposition in the basal ganglia. In this patient, psychiatric and neurological symptoms were worsening even after the treatment had been finished, and MRI examinations showed that atrophy was also advancing. On the other hand, the outcome for the remaining 1 patient was quite good, and he was able to get a job although he had manic symptoms. He had only slight frontal atrophy, and even at the time of reexamination 1 year later there were no changes on MRI. Cerebral atrophy and gliosis, dominantly in the frontal lobes, were equivalent to well-known neuropathological findings of general paresis;2,9 they were not very unusual findings and had little diagnostic value. There have been no studies of ferritin deposition in general paresis.
Russouw et al.10 performed MRI in 20 patients with neurosyphilis, and results in 13 of them proved to be abnormal. T2-weighted images showed high-intensity areas in 11 of the 20 patients and atrophy in the remaining 9. Furthermore, lesions in the frontal lobes proved to have a significant correlation with score on the Brief Psychiatric Rating Scale, and lesions in the temporoparietal lobes had a significant correlation with score on the Mini-Mental State Examination.
Longevity did not appear to be decreased in any of our patients, but only 4 were able to return to their jobs and regain almost the same social functioning level that they had before becoming ill. When we performed MRI before treatment, these 4 did not have any abnormal MRI findings except slight cerebral atrophy. On the other hand, in the remaining 3 cases, serious dementia or a personality change remained and a long stay in the hospital or special care at home was necessary. These 3 patients already had cerebral atrophy or dilation of the ventricles; moreover, medial temporal lobe atrophy had been recognized as a special feature before treatment. We looked for an etiology that might explain medial temporal lobe atrophy and residual impairment. There were no abnormal findings except syphilis-related abnormality in the patients' sera and CSF.
We consider that a neuroimaging finding of cerebral atrophy of various degrees mainly in the frontal lobes is equivalent to the pathological findings of general paresis reported so far,2,9 but we can scarcely find any pathological reports on atrophy of the medial temporal lobe including the hippocampus. Why atrophy occurs in the medial temporal lobe is unclear, but it may occur secondarily to dysfunction in the diffuse cerebral cortex, as the medial temporal regions have connections with the cerebral association areas, including the frontal, temporal, and parietal lobes. In our experience, when atrophy is observed in the medial temporal lobe including the hippocampus, the prognosis for the patient's social functioning may be poor in spite of proper treatment.
Early treatment for general paresis is considered to be effective in deciding the prognosis. But delay in starting treatment is not always the reason for a poor prognosis; some of our medial temporal atrophy patients (with a bad prognosis) had treatment started relatively soon after onset. We still do not know whether there is a type of general paresis in which cerebral atrophy would begin to worsen at a very early stage of the disease once its symptoms appeared. But even in these serious cases the patients benefited from treatment, their prognoses across the lifespan were good, and their activities in daily living were greatly improved.
On the other hand, in the case of a slight atrophy seen in neuroimaging, a high dose of antibiotics should be given from the beginning, irrespective of the patient's clinical condition. With this method we can expect the prognosis to be greatly improved. If the patient's clinical condition remained poor, it would be advisable to continue the large dose of antibiotics. Case 1 had shown cognitive disorders, mainly Korsakoff's syndrome, but after long-term treatment of 75 days with a high dose of antibiotics he returned to society with little memory disturbance. There are some reports11,12 from other groups concerning cases in which cerebral atrophy on CT worsened even after starting treatment. These patients had been given a small amount of penicillin (600,000 to 3 million units per day). When the patients showed prolongation and/or recurrence of psychiatric symptoms, the method of treatment was changed to a high dose of penicillin, but memory disturbance with personality change remained.
Among our cases, there has not been one in which cerebral atrophy worsened after starting treatment. In 4 cases we performed MRI again 3 to 6 years later; in 3 cases there was no change and in the remaining case only a slightly increased atrophy. Judging from the neuroimaging results, we believe that treatment with a high dose of antibiotics was very effective.
In summary, when patients with general paresis are treated, prognosis can be predicted on the basis of the existence of cerebral atrophy, especially medial temporal lobe atrophy that is detected by MRI. Patients with slight cerebral atrophy will have good social functioning after an effective high-dose antibiotics treatment. Even in patients with diffuse cerebral atrophy including the medial temporal lobe, a good prognosis across the lifespan can be predicted and more serious cerebral deterioration can be prevented when an effective high-dose antibiotics treatment starts during an early stage of the disease.
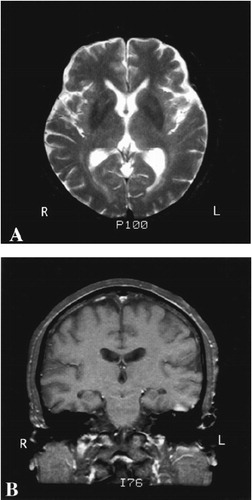
FIGURE 1. Case 1A: Axial T2-weighted image (TR=2,500, TE=90) showing mild frontal cortical atrophy. B: Coronal T1-weighted image (TR=100, TE=9); medial temporal lobe atrophy was not recognized.
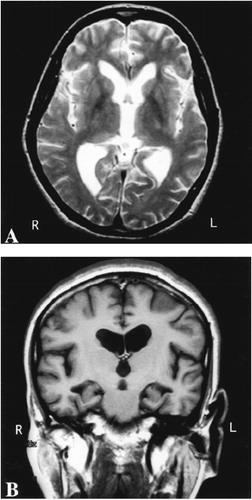
FIGURE 2. Case 7A: Axial T2-weighted image (TR=3,000, TE=98) showing cerebral atrophy mainly in the frontal lobes, dilation of the third and lateral ventricles. B: Coronal T1-weighted image (TR=440, TE=9) showing atrophy of the bilateral medial temporal lobe including the hippocampus.
 |
1 Hook EW III, Marra CM: Acquired syphilis in adults. N Engl J Med 1992; 326:1060–1069Google Scholar
2 Rowland LP: Spirochete infections: neurosyphilis, in Merritt's Textbook of Neurology, 9th edition, edited by Rowland LP. Baltimore, Williams and Wilkins, 1995, pp 200–208Google Scholar
3 Benson DF: The treatable dementias, in Psychiatric Aspects of Neurologic Disease, vol 2, edited by Benson DF, Blumer D. New York, Grune and Stratton, 1982, pp 123–148Google Scholar
4 Cummings JL: Treatable dementias, in Advances in Neurology, vol 38: The Dementias, edited by Mayeux R, Rosen WG. New York, Raven, 1983, pp 165–183Google Scholar
5 Centers for Disease Control: Sexually transmitted disease treatment guidelines. MMWR 1989; 38(S-8):1–43Google Scholar
6 Samuels MA (ed): Manual of Neurology, Diagnosis and Therapy, 4th edition. Boston, Little, Brown, 1991Google Scholar
7 Adams RD, Victor M, Ropper AH: Principles of Neurology. New York, McGraw-Hill, 1997Google Scholar
8 Zifko U, Wimberger D, Lindner K, et al: MRI in patients with general paresis. Neuroradiology 1996; 38:120–123Crossref, Medline, Google Scholar
9 Gray F, Nordmann P: Bacterial infections, in Greenfield's Neuropathology, 6th edition, vol 2, edited by Graham DI, Lantos PL. London, Edward Arnold, 1997, pp 113–152Google Scholar
10 Russouw HG, Roberts MC, Emsley RA, et al: Psychiatric manifestations and magnetic resonance imaging in HIV-negative neurosyphilis. Biol Psychiatry 1997; 41:467–473Crossref, Medline, Google Scholar
11 Nishiyama E, Takahashi T, Iwamoto N, et al: A case with general paresis recovered from long-term catatonia-like stupor by high-dose intravenous penicillin therapy [Japanese]. Jpn J Clin Psychiatry 1995; 24:93–98Google Scholar
12 Takahashi M, Hasegawa O, Fujita H, et al: A case of general paresis with marked improvement of cerebral blood flow after antiluetic therapy: case report [Japanese with English abstract]. No To Shinkei 1992; 44:645–648Medline, Google Scholar