Depression, Avolition, and Attention Disorders in Patients with Schizophrenia: Associations with Verbal Memory Efficiency
Previous research from our group has suggested that depression, rather than negative symptomatology, is involved in the memory impairment. 5 This dimension is rarely taken into account in cognitive studies conducted in this population. However, depressive symptoms are prevalent in patients with schizophrenia, and they register as an important component in recent factor analyses of symptomatology in the disorder. 6 The commonly found association between negative symptoms and cognitive impairment may partly result from some overlap between depressive and negative symptomatology. Depression has been shown to affect verbal memory efficiency in a number of populations including children, 7 the elderly, 8 patients with affective disorders, 9 and patients with Parkinson’s disease. 10 In our previous schizophrenia sample, depression specifically affected effortful memory processes, in agreement with what was observed in individuals with primary depression. 11 Depression score was associated with impaired ability to organize lists of words in semantic categories, which reflects deep encoding. By contrast, it was not associated with the serial learning of items by rote rehearsal, which constitutes the most superficial way of encoding verbal information. The influence of depression on verbal memory efficiency in patients with schizophrenia has been reported by other groups. 12 – 14 However, several studies failed to reveal such a relationship. 15 – 18 Discrepancies may arise from differences in the scales used to assess depression, as well as from confounding factors, such as general verbal ability, or use of anticholinergic medication. Drugs with anticholinergic properties appear to affect verbal memory efficiency, 19 notably by impeding semantic organization of the material. 20
With regards to negative symptoms, the numerous studies which have investigated their potential influence on memory impairment in schizophrenia patients have most often reported the correlations with a global negative symptom score. One reason for the weak associations observed may be that multiple symptoms are combined together, thereby obscuring possibly stronger relationships with specific symptoms. A more effective approach might be to investigate the role of individual symptoms. One symptom which is likely to be involved in poor cognitive performance is volitional deficiency. Our previous research indicated that, among all the negative symptoms assessed by both the Scale for the Assessment of Negative Symptoms (SANS) and the Positive And Negative Syndrome Scale for Schizophrenia (PANSS), only avolition from the SANS was significantly associated with verbal memory performance. 21 This might be a spurious result, stemming from a number of computed correlations. Alternatively, avolition might be a genuine factor in the impaired memory performance in this population. The correlation between verbal memory and SANS scores observed in several studies might have been mostly accounted for by this symptom, pointing to impairment in motivational processes. Successful performance relies not only on specific cognitive abilities, but also on the degree of invested effort to complete the task. Motivation could be seen as a cognitive energetic reserve to be drawn from for performing any task irrespective of its intrinsic difficulty. Recent studies have revealed the role of mental effort on cognition in schizophrenia. 22 , 23 Schmand et al. 24 suggested that a motivational deficit underlies the association between negative symptoms and cognitive impairment in these patients. Although motivation might be crucial in cognitive and social functioning, its role has been understudied in schizophrenia, and warrants more systematic investigation. A better understanding of the impact of motivational processes would enable us to delineate more accurately the extent of the cognitive deficit. Besides, this would have practical implications for cognitive therapies if it were established that a significant amount of the observed impairment in memory and other cognitive domains is attributable to lack of motivation, rather than to impaired ability to perform the task.
Another clinical symptom that might be relevant for memory performance is attentional impairment. A disturbance in attention is commonly observed in patients with schizophrenia, and may contribute to their poor memory efficiency. Attention disorders might impede effective encoding by preventing the subjects from properly attending to the stimuli at the acquisition stage. Nevertheless, the few studies which have addressed the issue of the relationship between memory performance and various cognitive measures of attention in schizophrenia have not revealed a major role of attention deficit. 1 We observed in previous research that selective attention measured by the Stroop test was not associated with global verbal memory efficiency, or with any of the memory measures reflecting deep encoding. 25 However, deficits in selective attention were associated with impairment in the ability to encode and maintain series of either words or digits in memory by means of rote rehearsal. Likewise, distractibility, which stems from attentional dysfunction, has been suggested to interfere with the rehearsal processes of serial learning in schizophrenia patients 26 and children at risk for schizophrenia. 27 A specific relationship with serial encoding might similarly be observed when attentional impairments are assessed at the clinical level. Attention disorders are generally not considered a negative symptom, but they are nonetheless commonly evaluated as part of the SANS rating scale.
In this study, we wished to confirm in another schizophrenia sample our previous finding that depression has a significant effect on verbal memory efficiency, especially with regards to the deep encoding processes. A memory task yielding various levels of encoding was prepared. The most superficial encoding level was assessed by the forward digit span test, which merely requires learning sequences of digits. Three lists of words with increasing difficulty were administered. One list was not organizable; one was semantically organizable and contained typical instances of the semantic categories; the last list was semantically organizable with atypical examples, and presumably required even deeper processing than the typical one. We conducted regression analyses on the various memory scores to test the hypothesis that depression, rather than a global negative symptom score, was a significant predictor of verbal memory efficiency. More specifically, we expected the association with the recall of the organizable lists to be stronger than that with the recall of the nonorganizable list, and an even stronger correlation was expected for the atypical than for the typical organizable list. By contrast, no association between depression and the forward digit span was expected, since depression usually spares the superficial memory processes, and was unrelated to the efficiency of serial encoding in our previous study. Verbal IQ and use of antipsychotic medication with intrinsic anticholinergic activity were included in the regression analyses, in order to control for their potentially confounding effect.
Our second purpose was to test the hypothesis that certain clinical symptoms, commonly assessed in schizophrenia but not studied on their own, have a significant impact on memory performance. The SANS was used for clinical symptom assessment, and an extensive score for each symptom was tallied by summing the subscores which constitute the symptom. On the basis of our previous results, we hypothesized that avolition score would be significantly correlated with the total number of recalled words assessing global verbal memory efficiency. This would confirm an association which was not expected in our previous study, but rather emerged from a post-hoc analysis. Possible correlations between avolition score and other memory measures were explored, to determine the scope of the effect. Attention disorders were expected to be significantly associated with serial learning assessed by the forward digit span, in agreement with the findings from previous studies. By contrast, they were not expected to be associated with the other memory scores, which reflect deeper processes than serial learning. No significant association between the other SANS symptoms (affective flattening, alogia, and anhedonia) and any of the memory measures was expected.
METHODS
Participants
Forty-one patients with schizophrenia (8 inpatients) were recruited at the Maudsley Hospital, London (see Table 1 for sociodemographic and clinical information). They were all taking antipsychotic medication except three patients who were declining to take any medication. Fourteen of the patients were taking antipsychotic medication with intrinsic anticholinergic activity (olanzapine, clozapine, zuclopenthixol). Diagnosis was made on the basis of DSM-IV criteria by two senior psychiatrists who used patients’ history and chart review, and reached a consensus. Patients with substance abuse and comorbid medical or psychiatric conditions were excluded. Ethical approval for the study was obtained from the South London and Maudsley NHS Trust Ethics Committee. After a full explanation of the study, subjects provided written informed consent to participate.
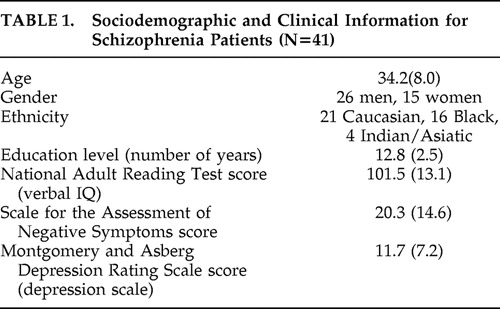 |
Clinical Ratings
The Montgomery and Asberg Depression Rating Scale (MADRS 28 ) was used to assess severity of depression. It includes 10 items (apparent sadness, reported sadness, inner tension, reduced sleep, reduced appetite, concentration difficulties, lassitude, inability to feel, pessimistic thoughts, suicidal thoughts), with a possible score ranging from 0 to 6 for each item. The total score range in the sample was 0–26. Negative symptoms and attention disorders were assessed with the SANS (score range=0–62). A score for each symptom was computed by summing the subscores which constitute this symptom (affective flattening: range=0–21, mean=6.2, SD=6.5; alogia: range=0–12, mean=2.3, SD=3.1; avolition/apathy: range=0–12, mean=3.9, SD=2.9; anhedonia: range=0–14, mean=6.8, SD=4.5; and attention disorders: range=0–7, mean=1.1, SD=1.7). The psychiatrists were blind to cognitive results during clinical assessment. Likewise, the experimenter (GB) was blind to patients’ symptoms during testing.
Forward Digit Span
The forward digit span test from the WAIS-Revised (WAIS-R 29 ) was administered. Increasingly long series of digits had to be repeated in the same order. The measure used was the total number of correct trials. This task was assumed to assess the superficial memory processes of serial encoding.
Lists of Words
Eight lists of 16 concrete words, equivalent in average number of syllables, were prepared. Four of the lists were made up of non semantically-related words, and only one of them chosen at random was presented for immediate recall. Four other lists were organizable into four semantic categories selected from Battig and Montague. 30 Two of them were made up of four typical instances within each category, whereas the other two were made up of four atypical instances. The words were distributed randomly within the lists, so that the semantic organization was not obvious. The subjects were presented with one typical and one atypical semantically organizable list. The choice of the target lists, as well as the order of presentation of the semantically organizable lists, was counterbalanced among subjects.
All the lists of words were printed. The nonorganizable list was administered first. The subjects were presented with the list and informed that they had 45 seconds to learn the words, and had to read them aloud at least once. Immediately after learning, they were provided with a blank sheet and required to write down all the words they could remember in any order. No time limit was imposed for free recall. Then one of the organizable lists was administered following the same procedure, and finally the other organizable list. The subjects were not informed that certain lists were semantically organizable. The numbers of words recalled in each list were tallied and used as dependent variables. In addition, a global verbal memory measure was computed by summing the number of words recalled in the three lists (total number of recalled words).
All the memory and clinical variables followed a normal distribution except the attention disorder score from the SANS, which was normalized by square-root transformation before data analysis. All statistical tests were two-tailed.
RESULTS
Memory Scores
The scores obtained by the patients on the memory measures were as follows: forward digit span: mean=7.0, SD=1.8; number of recalled words: nonorganizable list: mean=5.5, SD=2.1; typical organizable list: mean=6.4, SD=3.0; atypical organizable list: mean=5.0, SD=2.7; total number of recalled words: mean=16.9, SD=6.9. An analysis of variance (ANOVA) conducted on the number of words recalled in each of the three lists revealed a significant main effect of the type of list (F=7.54, df=2, 80, p<0.001). Notably, fewer words were recalled in the atypical than in the typical organizable list (F=15.1, df=1, 40, p<0.0001). The role of list structure on recall efficiency in mostly the same sample, as well as the impairment relative to a healthy control group, was fully discussed in a previous paper. 31 The patients were highly significantly impaired on the forward digit span and on the number of recalled words.
Associations of Memory Scores With Negative and Depressive Symptomatology
A matrix of the bivariate correlations among the memory measures and SANS, MADRS, and National Adult Reading Test (NART) scores is presented in Table 2 . The MADRS and SANS scores were significantly intercorrelated (r=0.52, p<0.001), which demonstrates the necessity to include these two variables together in regression analyses, so as to study the independent contribution of each to the memory impairment. Regression analyses were conducted on the memory measures. The SANS and MADRS scores were entered as predictors. The NART score, reflecting verbal intellectual level, and the use of antipsychotic medication with intrinsic anticholinergic activity (categorical variable) were entered as well, in order to control for their potentially confounding effect. All four predictors were entered together in the regression. Results are presented in Table 3 .
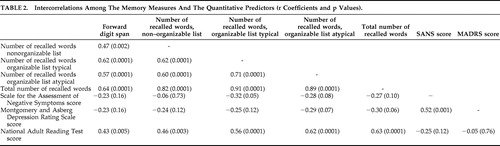 |
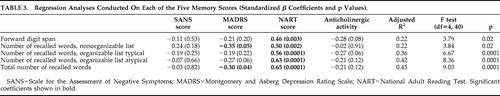 |
The NART score was a highly significant predictor of all the memory measures. The SANS score was not a significant negative predictor of any of the memory measures. If anything, it presented a positive, although nonsignificant, association with the number of words recalled in the nonorganizable list. By contrast, the MADRS score was a significant negative predictor of the total number of recalled words, as expected. Contrary to our hypothesis however, depression was not significantly associated with the recall of the typical organizable list, and was only marginally significantly associated with the recall of the atypical organizable list. The association between MADRS score and forward digit span was far from significant.
The type of antipsychotic medication made a marginally significant contribution to the recall of the typical organizable list. It should be noted that this contribution became significant when the scores from the typical and atypical organizable lists were summed (β=−0.26, p<0.05). This finding indicates that the patients who took antipsychotic treatment with intrinsic anticholinergic activity were impaired in the recall of these lists, relative to the other patients. In view of the significant role of antipsychotic medication, we recomputed a regression analysis in the subsample of 27 patients who did not take any antipsychotic drug with anticholinergic activity, after checking the normality of the score distributions. The criterion variable was the total number of recalled words. The SANS, MADRS and NART scores were entered together as predictors. The model yielded an adjusted R 2 =0.47 (F=8.62, df=3, 26, p<0.001). Results show that the SANS score did not make any negative contribution to the total recall score (β=0.15, p>0.43), whereas the strength of the association with the MADRS score was enhanced relative to that observed in the whole sample (β=−0.42, p<0.04). The NART score remained a highly significant predictor (β=0.60, p<0.0001).
In order to quantify the proportion of memory variance that was explained by depression, NART score, and drugs with intrinsic anticholinergic activity, we examined the variation in adjusted R 2 induced by removing each of these factors from the model. A regression analysis on the total number of recalled words was conducted in the whole sample, using MADRS score, NART score, and type of antipsychotic medication as predictors entered all together. The SANS score was omitted, since it did not show any effect on the total recall score. Then each predictor was alternately removed from the regression analysis, and the resulting variation in adjusted R 2 was studied. The results are reported in Table 4 . It appears that the MADRS score explained 8.3% of the variance in total recall, while the NART score explained 41.7%, and the use of antipsychotic medication with intrinsic anticholinergic activity explained 2.3%. Analyses conducted in the subsample of 27 patients who did not take antipsychotic treatment with intrinsic anticholinergic activity revealed that 9% of the variance in total recall was accounted for by the depression score, and 31.5% by the NART score.
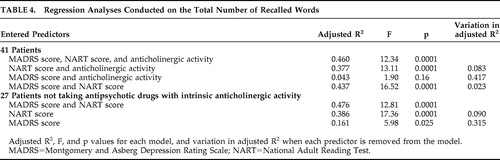 |
Complementary analyses with the same predictors were conducted on the scores obtained on the nonorganizable versus semantically organizable lists, to test the hypothesis that depression especially affects the learning of the organizable lists, requiring deep encoding processes. In the whole sample, the MADRS score accounted for 3.5% of the variance in the recall of the nonorganizable list, and for 8.2% of the variance in the summed recall of the two semantically organizable lists. In the subsample of 27 patients, the proportion of variance explained by depression was 0.1% for the nonorganizable list, and 10.9% for the summed two semantically organizable lists.
Correlations Between Memory Scores and Individual SANS Symptoms
We then tested the hypothesis that, in spite of the lack of association with the global negative symptom score, avolition and attention disorders were associated with certain memory measures. The correlations between the memory measures and each of the SANS symptom scores were computed, after controlling for NART score and use of antipsychotic medication with anticholinergic activity. Results are presented in Table 5 .
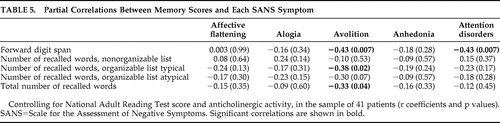 |
The avolition score was significantly correlated with the total number of recalled words, as expected. It was also significantly correlated with the forward digit span and with the recall of the typical organizable list, and tended to be correlated with the recall of the atypical list. In agreement with our hypothesis, attention disorders were significantly correlated with the forward digit span, but not significantly related to any word recall score. No significant or trend level correlation emerged between the other SANS symptoms (affective flattening, alogia, and anhedonia) and any of the memory scores.
The patients who did not present attention disorders might obscure any potential association with memory. We therefore recomputed the partial correlations between attention disorder score and memory measures in the subsample of 18 patients with attention disorders (score≥1), after checking that all studied variables followed a normal distribution. The negative correlation between attention disorder score and digit span remained significant (r=−0.54, p<0.03). The negative correlations with the other memory scores were far from significant (p>0.31 in all cases).
DISCUSSION
Memory efficiency has been shown to play a crucial role in daily living and social outcome in patients with schizophrenia. 3 It is therefore particularly important to determine the factors that are involved in the pronounced verbal memory impairment consistently observed in this population, in order to develop more targeted and effective treatment. Our previous finding concerning the role of depression was an important one, which called for replication. 5 In the current study, regression analyses involving both negative and depressive symptomatology indicated that the global negative symptom score did not present any significant association with any memory measure. By contrast, the depression score was significantly associated with the total number of recalled words, while it was unrelated to the forward digit span reflecting superficial encoding by serial learning. Our results therefore confirm that depression, rather than negative symptoms, contributes to the verbal memory impairment in patients with schizophrenia, at least insofar as deeper mechanisms than serial learning are involved. A similar pattern of associations between depressive symptoms and verbal memory measures requiring deep, but not superficial, encoding was reported by other groups. 12 , 14
It should be noted that the association with depression, although significant, was moderate. Correlational and regression analyses in the whole sample suggested that this association did not concern the semantically organizable lists of words any more than the nonorganizable list, contrary to our hypothesis. However, the relationship between memory efficiency and depression appears to be influenced by the use of antipsychotic drugs with intrinsic anticholinergic activity. The association between MADRS score and total recall was enhanced in the subsample of patients who did not take this type of medication (β=−0.42 in the subsample versus β=−0.30 in the whole sample). Furthermore, in this subsample, depression explained a substantial proportion of the variance in the recall of the semantically organizable lists (10.9%), but not in the recall of the nonorganisable list (0.1%). This suggests that depression affects the deep processes of semantic encoding.
Overall, the effect of depression appears less striking than that observed in our previous sample. 5 The reduced magnitude of this effect is not likely to be due to the task, which was at least as demanding as that designed in the previous study. The 21-item Hamilton Depression Rating Scale used in the previous study probably captures more of the relevant features of depression than the 10-items MADRS. Depression includes a variety of components, some of them being also part of negative symptomatology (e.g., blunted affect, social avoidance, disturbance of volition, psychomotor retardation). Our pattern of data suggests that depression affects memory through its volitional component. Other aspects more specific to the depressive state also play a role. More particularly, anxiety, which is included in the Hamilton Depression Rating Scale, was strongly associated with impaired ability to use the semantic organization in our previous data. It accounted for a great part of the association between depression score and memory efficiency. The fact that anxiety is not included in the MADRS probably explains the weak association with the recall of the organizable lists in the current data. Fatigue might also contribute to the association between memory efficiency and depression. Future studies of memory functioning in patients with schizophrenia should take into consideration the potentially deleterious role of depression. The association of memory performance with depressive severity, which has been robustly established in patients with primary depression, 9 , 11 and also observed in other clinical 10 and nonclinical 7 , 8 populations, is underestimated in schizophrenia research. Assessment of depression and anxiety should be routinely included in cognitive studies of schizophrenia, which have so far most often focused on positive and negative symptomatology. Clinicians should also consider the role of depressive symptoms when they attempt to remediate cognitive impairment by either behavioral or pharmacological therapies.
The lack of significant associations between SANS score and any of the memory measures in the regression analyses is consistent with a meta-analysis indicating that negative symptomatology only accounts for a small amount of the memory deficit. 4 The finding of significant associations in some studies might have been influenced by confounding factors, notably verbal IQ, which appears to have a strong impact on all the memory measures. Our results underscore the importance of controlling intelligence level when studying the relationships between cognition and clinical symptoms. Furthermore, the reported associations of verbal memory with negative symptoms in the literature might partly arise from overlap between negative and depressive symptomatology. The matrix of bivariate correlations in our study revealed significant or trend associations between SANS score and word recall. However, these associations disappeared when the data were submitted to regression analyses, which controlled for the effect of the other factors. This observation suggests that these bivariate correlations were either accounted for by an element common to negative and depressive symptomatology, or an artifact of the strong associations between memory and verbal IQ.
As expected, avolition was the only symptom from the SANS to be significantly correlated with the total number of recalled words. This finding illustrates the advantage of studying the influence of individual symptoms, rather than using a global negative symptom score. The size of the correlation with avolition was modest, yet similar to that observed in our previous study (r=−0.33 in this sample versus r=−0.36 in Brébion et al.). 21 In the current data, avolition was also associated with other memory scores, which suggests the pervasiveness of its negative effect on memory. The associations between memory efficiency and SANS score observed in several studies might have been triggered by the avolition item. Our findings corroborate recent reports demonstrating the role of mental effort on cognitive efficiency in schizophrenia, 22 , 23 and give support to Schmand et al’s 24 suggestion that the effect of negative symptoms on cognitive efficiency stems from motivational deficit. Regardless of task difficulty, one cause of patients’ poor memory performance might be failure to invest sufficient mental effort to perform the task. Patients’ cognitive deficit may be overestimated due to their lack of motivation to work at the maximum of their capacities. The issue of motivation, as critical as it might be, has been poorly investigated so far, prompting the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) committee to call for more research on this topic. 32 The motivational processes could be assessed with extensive rating scales, as well as with behavioral tests. If a significant impact of motivation on memory, and possibly other functions, were robustly established in this population, this would raise hope that patients would benefit from cognitive rehabilitation techniques that would aim at improving their motivation to perform the task.
With regards to clinically rated attention disorders as defined in the SANS, their influence on memory efficiency in this sample was very limited. Attention disorder scores were not associated with global verbal recall, or recall of either type of word list. This corroborates the few studies which assessed attention by means of cognitive tasks and did not reveal a major role on memory efficiency. 1 However, attention disorders were significantly associated with impairment in encoding series of digits. This specific association confirms that obtained in our previous study, in which attention disorders were assessed at a cognitive level by means of the Stroop test. 25 It also corroborates findings from other groups. 26 , 27 Attention deficit, assessed by either cognitive measure or clinical rating, seems to affect verbal memory only insofar as it disrupts the serial learning processes. Admittedly, the attention score had a narrow range, thereby reducing the chance of detecting significant associations. In addition, the SANS rating subscale captures only restricted aspects of attention disorders, which limits the scope of the conclusions. Considering that attention is a complex construct, various clinical and behavioral measures of attention should be used to confirm that impairment in this function does not broadly affect verbal memory efficiency in patients with schizophrenia, but merely interferes with serial encoding.
A limitation of this study is the relatively small size of the sample. The regression analyses may have been underpowered, and a stronger effect of depression might have emerged in a larger sample. Furthermore, the MADRS was not designed to assess depression in schizophrenia patients. Future studies should use other scales more specific to this population, such as the Calgary Depression Scale. Lastly, the finding of associations between clinical symptoms and memory measures does not necessarily mean that these symptoms influence memory efficiency. The dorsolateral prefrontal cortex has been shown to play a role in both symptoms of avolition and depression. 33 This brain area has also been involved in the long-term memory deficits in patients with schizophrenia. 34 It is possible that the underlying neurobiological abnormalities that give rise to impaired memory functioning in this disorder also concomitantly give rise to the clinical manifestations of depression and avolition. Nevertheless, our findings suggest that more consideration should be given to these two clinical symptoms in experimental investigations of verbal memory and other cognitive functions in schizophrenia, as well as in therapeutic interventions aiming at improving cognition.
1. Cirillo MA, Seidman LJ: Verbal declarative memory dysfunction in schizophrenia: from clinical assessment to genetics and brain mechanisms. Neuropsychol Rev 2003; 13:43–77Google Scholar
2. Fletcher PC, Shallice T, Dolan RJ: The functional roles of prefrontal cortex in episodic memory. I. Encoding Brain 1998; 121:1239–1248Google Scholar
3. Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 1996; 153:321–330Google Scholar
4. Aleman A, Hijman R, de Haan EHF, et al: Memory impairment in schizophrenia: a meta analysis. Am J Psychiatry 1999; 156:1358–1366Google Scholar
5. Brébion G, Smith M, Amador X, et al: Clinical correlates of memory in schizophrenia: differential links between depression, positive and negative symptoms, and two types of memory impairment. Am J Psychiatry 1997; 154:1538–1543Google Scholar
6. Emsley R, Rabinowitz J, Torreman M: The factor structure for the positive and negative syndrome scale (PANSS) in recent-onset psychosis. Schizophr Res 2003; 61:47–57Google Scholar
7. Gunther T, Holtkamp K, Jolles J, et al: Verbal memory and aspects of attentional control in children and adolescents with anxiety disorders or depressive disorders. J Affect Disord 2004; 82:265–269Google Scholar
8. Lichtenberg PA, Ross T, Millis SR, et al: The relationship between depression and cognition in older adults: a cross-validation study. J Gerontology, Series B, Psychol Sciences & Soc Sciences 1995; 50B:25–32Google Scholar
9. Fossati P, Harvey P-O, Le Bastard G, et al: Verbal memory performance of patients with a first depressive episode and patients with unipolar and bipolar recurrent depression. J Psychiatr Res 2004; 38:137–144Google Scholar
10. Norman S, Troster AI, Fields JA, et al: Effects of depression and Parkinson’s disease on cognitive functioning. J Neuropsychiatry Clin Neurosci 2002; 14:31–36Google Scholar
11. Hartlage S, Alloy LB, Vasquez C, et al: Automatic and effortful processing in depression. Psychol Bull 1993; 113:247–278Google Scholar
12. Lysaker PH, Bell MD, Greig TC, et al: Emotional discomfort and impairments in verbal memory in schizophrenia. Psychiatry Res 2000; 97:51–59Google Scholar
13. Sanfilipo M, Lafargue T, Rusinek H, et al: Cognitive performance in schizophrenia: relationship to regional brain volumes and psychiatric symptoms. Psychiatry Res Neuroim 2002; 116:1–23Google Scholar
14. Moser C, Krieg JC, Zihl J, et al: Attention and memory deficits in schizophrenia: the role of symptoms of depression. Cogn Behav Neurol 2006; 19:150–156Google Scholar
15. Paulsen JS, Heaton RK, Sadek JR, et al: The nature of learning and memory impairments in schizophrenia. J Int Neuropsychol Soc 1995; 1:88–99Google Scholar
16. Kohler C, Gur RC, Swanson CL, et al: Depression in schizophrenia: association with neuropsychological deficits. Biol Psychiatry 1998; 43:165–172Google Scholar
17. Holthausen EAE, Wiersma D, Knegtering RH, et al: Psychopathology and cognition in schizophrenia spectrum disorders: the role of depressive symptoms. Schizophr Res 1999; 39:65–71Google Scholar
18. Lucas S, Fitzgerald D, Redoblado-Hodge MA, et al: Neuropsychological correlates of symptom profiles in first episode schizophrenia. Schizophr Res 2004; 71:323–330Google Scholar
19. Minzenberg MJ, Poole JH, Benton C, et al: Association of anticholinergic load with impairment of complex attention and memory in schizophrenia. Am J Psychiatry 2004; 161:116–124Google Scholar
20. Brébion G, Bressan RA, Amador X, et al: Medications and verbal memory impairment in schizophrenia: the role of anticholinergic drugs. Psychol Med 2004; 34:369–374Google Scholar
21. Brébion G, Amador X, Smith M, et al: Depression, psychomotor retardation, negative symptoms, and memory in schizophrenia. Neuropsychiatry Neuropsychol Behav Neurol 2000; 13:177–183Google Scholar
22. Gorissen M, Sanz JC, Schmand B: Effort and cognition in schizophrenia patients. Schizophr Res 2005; 78:199–208Google Scholar
23. Van Beilen M, Van Zomeren EH, Van den Bosch RJ, et al: Measuring the executive functions in schizophrenia: the voluntary allocation of effort. J Psychiatr Res 2005; 39:585–593Google Scholar
24. Schmand B, Kuipers T, van der Gaag M, et al: Cognitive disorders and negative symptoms as correlates of motivational deficits in psychotic patients. Psychol Med 1994; 24:869–884Google Scholar
25. Brébion G, Smith M, Gorman J, et al: Memory and schizophrenia: differential link of processing speed and selective attention with two levels of encoding. J Psychiatr Res 2000; 34:121–127Google Scholar
26. Oltmanns TF: Selective attention in schizophrenic and manic psychosis: the effect of distraction on information processing. J Abnorm Psychol 1978; 87:212–225Google Scholar
27. Harvey P, Winters K, Weintraub S, et al: Distractibility in children vulnerable to psychopathology. J Abnorm Psychol 1981; 90:298–304Google Scholar
28. Montgomery SA, Asberg M: A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134:382–389Google Scholar
29. Wechsler D: Manual for the Wechsler Adult Intelligence Scale. New York, Psychological Corporation, 1981Google Scholar
30. Battig WF, Montague WE: Category norms for verbal items in 56 categories: a replication and extension of the Connecticut category norms. J Exp Psychol (Monograph) 1969; 80:1–46Google Scholar
31. Brébion G, David AS, Jones H, et al: Semantic organization and verbal memory efficiency in patients with schizophrenia. Neuropsychology 2004; 18:378–383Google Scholar
32. Barch DM: The relationships among cognition, motivation, and emotion in schizophrenia: how much and how little we know. Schizophr Bull 2005; 31:875–881Google Scholar
33. Nitschke JB, Mackiewicz KL: Prefrontal and anterior cingulate contributions to volition in depression. Int Rev of Neurobiol 2005; 67:73–94Google Scholar
34. Barch DM, Csernansky JG, Conturo T, et al: Working and long-term memory deficits in schizophrenia: is there a common prefrontal mechanism? J Abnorm Psychol 2002; 111:478–494Google Scholar



