The Relationship Between Stressful Life Events and Cognitive Function in HIV-Infected Men
Abstract
Previous studies have demonstrated an impact of stress on immune function, and recent studies have suggested an adverse effect of stress on the brain. However, no previous study has examined the impact of stress on cognitive function. This article examines the relationship between stress and cognitive function in 82 HIV-negative subjects and 251 HIV-positive subjects. Subjects completed a comprehensive neuropsychological examination, measures of anxiety and depression, and a measure of stressful life events. After controlling for the impact of anxiety, depression, age, and education, stressful life events were related to cognitive impairment only among the HIV-positive subjects. The data were interpreted in the context of previous studies that have demonstrated an adverse effect of stress on the brain and suggest that this adverse impact may be expressed in the setting of a compromised immune system. Furthermore, this analysis suggests several implications for patient management.
Over the past decade, there have been numerous investigations of the nature and prevalence of cognitive dysfunction in human immunodeficiency virus (HIV)-infected people. There is clear agreement that cognitive impairment is more common in patients with more advanced infection. Although there has been considerable controversy, there is an emerging consensus that a small proportion of patients with early-stage infection may also have subtle cognitive impairment that may be sufficient to interfere with normal daily functions.1 Numerous additional investigations have begun to isolate the factors associated with the identification or prevalence of these impairments.
Previous investigations have demonstrated that increasing age, an increasing level of immune suppression, a history of acquired immune deficiency syndrome (AIDS) defining opportunistic infections, and a lower premorbid level of ability are associated with greater risk of cognitive impairment.2,3,4,5 In contrast, depression does not appear to be consistently associated with greater impairment in HIV-infected people. Preliminary data have indicated that a higher level of anxiety is associated with cognitive impairment in HIV-infected patients. Recent studies have begun to examine the association of psychosocial factors, such as social support and cognitive function in HIV-infected people.6
Life stress has frequently been examined in the context of psychosocial factors in HIV-infected people because of the known effects of stress on immune function.7,8 In the context of cognitive function in HIV-infected people, the potential importance of stress has gained increased support from emerging literature that has demonstrated its adverse effects on brain structure and function. Several animal studies have reported atrophy in the CA3 region of the hippocampus in response to stress.9,10 The structural remodeling caused by chronic stress is mediated by glucocorticoid hormones interacting with excitatory amino acids and N-methyl-d-aspartate receptors and transmitters such as serotonin and the GABA-benzodiazepine system.9 In addition, the rodent hippocampus contains many receptors for corticosterone, a glucocorticoid secreted in response to stress. Corticosterone appears to regulate levels of internal calcium (Ca2+) and thus may influence synaptic plasticity, aging, and cell death.10 Furthermore, human studies have demonstrated evidence of brain atrophy and abnormalities in function as a result of heightened levels of glucocorticoids and severe, traumatic stress.9
In view of the evidence of the adverse impact of stress on immune function as well as on brain structure and function, it is important to explore the potential role of stress as a mediator of cognitive dysfunction in HIV-infected people. Toward this end, we examined the relationship between cognitive function and stressful life events in a large sample of HIV-infected patients and HIV-seronegative controls. Because of the potential impact of age, education, depression, and anxiety, these variables were included as covariates in the analyses.
METHODS
Subjects
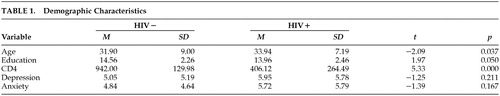
The sample consisted of 251 HIV-positive (HIV+) and 82 HIV-negative (HIV−) gay or bisexual, predominantly white (92.2%), male volunteers who were recruited specifically for participation in this research project. In this study, asymptomatic, symptomatic, and AIDS patients were included in the HIV+ group. 49.1% of the HIV+ sample had a CD4 count greater than 400/mm3, 27.5% had a CD4 count ≥ 200/mm3 and ≤400/mm3, and 23.4% had a CD4 count less than 200/mm3. The two groups were similar for levels of depression and anxiety, but the control group was significantly younger and had significantly more years of education than the HIV+ group. Demographic data are summarized in Table 1. There was no attempt to select subjects with subjective complaints of cognitive impairment. Individuals with histories of intravenous drug use, head injury resulting in unconsciousness for more than 60 minutes, neurologic disorder, or learning disorder were excluded.
Both control and HIV+ subjects were informed of the study through registration with an AIDS Clinical Trials Unit (ACTU), through local HIV-related community support groups, by newspaper advertisements, or by word of mouth. Subjects were provided with an informational brochure describing the study. All participants received detailed descriptions of the nature and purposes of the study, and all gave written informed consent. Blood samples were drawn during the subjects' regularly scheduled ACTU visits, which corresponded to the time of enrollment in this study. Prior to their enrollment, subjects were followed as part of a cohort in the ACTU. Serostatus was determined by enzyme-linked immunosorbent assay, and positive assays were confirmed by Western blot.
Procedures
Neuropsychological Measures: Subjects completed an extensive neuropsychological battery that included standardized neuropsychological measures and a series of simple and choice reaction-time measures. Because the nature of cognitive changes in HIV infection has been characterized as a subcortical dementia,11 tests were selected on the basis of demonstrated sensitivity to the effects of subcortical dementia in general and HIV infection in particular. The following standardized neuropsychological measures were used: Wechsler Adult Intelligence Scale-Revised, Selective Reminding Test, Visual Memory Span Forward and Backward from the Wechsler Memory Scale-Revised, Verbal Concept Attainment Test, Wisconsin Card Sorting Test, Verbal Fluency, Figural Fluency, Trail Making A and B, Grooved Pegboard, and the Paced Auditory Serial Addition Test.
Simple and choice reaction-time measures were also included because these tasks have consistently been found to be sensitive to the effects of HIV infection.12 In addition to performance on the individual neuropsychological measures, a summary performance score was determined for each subject that represented the number of measures on which subjects' performance was one standard deviation below the mean of controls.
Self-Report Measures: All subjects completed a questionnaire derived from the Psychiatric Epidemiology Research Interview (PERI) Life Events Scale,13 which was designed to measure stressful life events. The questionnaire consists of a list of 47 events in seven different categories: relationships and love, family, residence, crime and legal matters, finances, health, and other. Some categories (i.e., relationships and love) include both positive (i.e., monogamous commitment in a relationship/engaged) and negative (i.e., partners separated) events, whereas other categories were exclusively either positive or negative events. For the categories that included both positive and negative events, separate scores were computed. The subjects were asked to report the events that had occurred during the past year and whether or not they felt in control of these events. The PERI Life Events Scale is a well-recognized measure, which is commonly used in studies of the effects of life stress.14,15 These life events represent chronic stress, as they generally result in a change in lifestyle. The consequences of these life events do not simply dissipate after a short period but must be dealt with over time. The subjects identified events that had occurred within the past year; however, the effects of the stress resulting from the events are probably still present in the subjects' lives. Furthermore, the questionnaire derived from the PERI was modified so that it specifically applied to gay males. In addition to the total life events score, separate scores that reflected the frequency of life events in each of the above categories were computed. Subjects also completed the Hamilton Rating Scale for Depression and the Hamilton Rating Scale for Anxiety.
RESULTS
Prior to examining the relationship between stressful life events and cognitive performance, it was important to examine the impact of potential confounding variables such as age, education, depression, and anxiety that may influence cognitive function as well as perceptions of stress. As expected and as seen in Table 2, depression and anxiety were highly correlated (r = .86, p < .001). Depression and anxiety were also related to overall impairment. Table 3 presents the Pearson correlations between age, education, depression, and anxiety and the component scores from the PERI. There were several significant relationships. It was essential to control for these effects in order to determine whether life stressors had an impact on cognitive function that was independent of these confounding variables. Therefore, we decided to include these variables in a partial correlation analysis and control for the effects of age, education, anxiety, and depression.
It was also important to determine whether marijuana use was correlated with stressful life events, as previous studies have found evidence of such a relationship. However, no significant Pearson correlations existed between marijuana use and the subcategories of stressful life events in either the HIV-sample or the HIV+ sample. Therefore, it was not necessary to control for marijuana use in our analyses.
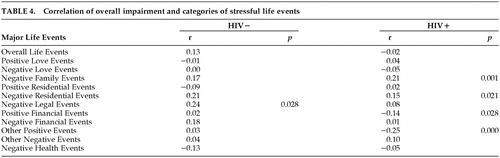
The results of the partial correlation analyses are presented in Table 4 and Table 5. Table 4 presents the Pearson correlation coefficients between overall impairment and life stressors for the HIV-negative and HIV-positive subgroups. It can be seen that several of the life stress areas were significantly correlated with cognitive function. These relationships suggest that more positive life events or fewer negative stressors were related to better cognitive performance. However, when the confounding variables were included in the partial correlation analysis, most of the significant relationships in the HIV-negative subjects were attenuated. The only relationship that remained significant in the HIV-negative subgroup was the relationship between overall impairment and negative home events (r = .26, p < .05). Similarly, the number of individual cognitive tests that were significantly related to life stress categories was not greater than would be expected by chance alone. A total of 264 partial correlations were computed, and only nine of these were significant, which is less than the number of correlations expected to be significant by chance alone.
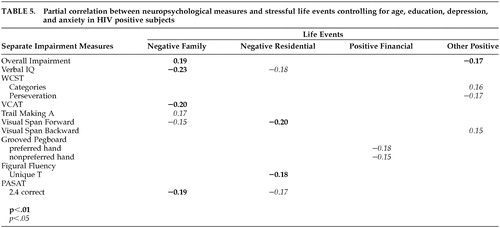
In contrast, there were numerous individual cognitive tests as well as the overall impairment measure that were significantly related to life stress categories, even after the effects of age, education, anxiety, and depression were controlled. Here, 25 out of 264 partial correlations were significant, which is above chance level. Furthermore, the great majority of these correlations (22) were in the hypothesized direction, suggesting that the results were not due to chance. As seen in Table 5, negative family events were strongly related to the overall impairment score as well as a broad range of cognitive and motor tasks. Negative residential events and positive life occurrences, such as positive financial events, were also related to a broad range of neuropsychological measures. The remaining correlations were scattered relationships and revealed no apparent pattern, and therefore are not included in the table. Further review of Table 5 indicates that most of the significant relationships with life stresses were observed on measures of executive function and attention and processing speed.
DISCUSSION
The data indicate that stressful life events are related to specific aspects of neuropsychological performance. Furthermore, the data suggest that the effect is only found in HIV+ individuals. For HIV+ subjects, negative stressors are related to worse performance on measures of executive function and attention and processing speed, while positive life events are related to better performance on these measures. The relationship between stress and neuropsychological performance could not be attributed to extraneous variables such as age, education, depression, anxiety, or marijuana use. To our knowledge, this is the first demonstration of a relationship between stressful life events and cognitive function. This extends previous studies that analyzed the adverse effects of stress on the brain.
Most of the previous studies conducted on humans have utilized individuals who were subject to chronic, severe stress (i.e., holocaust survivors).16 Past studies have not examined cognitive function in relation to stress as reflected by current stressful life events, and they have focused on memory in view of the relationship between stress and hippocampal atrophy.9,10 In this study, no relationship was observed between stressful life events and memory, although relationships were found with executive function, attention, and information processing speed. This is consistent with recent studies of patients with posttraumatic stress disorder that demonstrated abnormalities on working memory17 and attention.18
The finding that stressful life events was significantly related to cognitive performance only in the HIV-infected subjects is of interest and could suggest that immunocompetence provides a buffer against the adverse effects of stress. This would be consistent with recent studies from our laboratory, which suggest that HIV may interact with conditions that affect the immune or central nervous system. In these studies, alcohol use19 and anxiety (Melhem et al., under review) were found to impact cognitive function only in the HIV-infected subjects. These data were interpreted to suggest that the relatively subtle effects of such conditions may not normally be expressed but may manifest in the setting of immunosuppression. The current data may be interpreted in a similar context and suggest that although stress is not associated with cognitive dysfunction in immunocompetent individuals, the potential adverse effects of stress on the brain9 become expressed in the setting of a compromised immune system.
These data also have implications for patient care and management. If life stress is associated with cognitive dysfunction, there may be potential for alleviating this dysfunction through therapeutic interventions such as stress management. Health care providers could be encouraged to become aware of stress levels in immunocompromised subjects and facilitate referrals to programs designed to resolve stressors or to assist in stress management skills.
ACKNOWLEDGMENTS
This study was supported by grants from the National Institute of Mental Health (MH45649), the National Institute on Drug Abuse (DA10248), and the National Institute on Alcohol Abuse and Alcoholism (AA11720).
 |
 |
 |
 |
 |
1 White DA, Heaton RK, Monsch AU, et al: Neuropsychological studies of asymptomatic human immunodeficiency virus-type-1 infected individuals. JINS 1995; 1:304–315Crossref, Medline, Google Scholar
2 Arendt G, Hefter H, Nelles HW, et al: Age-dependent decline in cognitive information processing of HIV-positive individuals detected by event-related potential recordings. J Neurol Sci 1993; 115:223–229Crossref, Medline, Google Scholar
3 Bornstein RB, Nasrallah HA, Para MF, et al: Rate of CD4 decline and neuropsychological performance in HIV infection. Arch of Neurol 1991; 48:704–707 Crossref, Medline, Google Scholar
4 Basso MR, Bornstein RA: Effects of immunosuppression and disease severity upon neuropsychological function in HIV infection. J Clin Exp Neuropsycol 2000; 22:104–114Crossref, Medline, Google Scholar
5 Stern RA, Silva SG, Chaisson N, et al: Influence of cognitive reserve on neuropsychological functioning in asymptomatic human immunodeficiency virus-1 infection. Arch Neurol 1996; 53:148–153Crossref, Medline, Google Scholar
6 Honn VJ, Bornstein RA: Social support, neuropsychological performance and depression in HIV infection. J Int Neuropsychol Soc 2002; 8:436–447Crossref, Medline, Google Scholar
7 Patterson TL, Semple SJ, Temoshok LR, et al: Stress and depressive symptoms prospectively predict immune change among HIV-seropositive men. Psychiatry 1995; 58:299–312Crossref, Medline, Google Scholar
8 Evans DL, Leserman J, Perkins DO, et al: Severe Life Stress as a Predictor of early disease progression in HIV infection. Am J Psychiatry 1997; 154:630–634Crossref, Medline, Google Scholar
9 McEwen BS: Effects of adverse experiences for brain structure and function. Biol Psychiatry 2000; 48:721–731Crossref, Medline, Google Scholar
10 Kim JJ, Yoon KS: Stress: metaplastic effects in the hippocampus. Trends Neurosci 1998; 21:505–509Crossref, Medline, Google Scholar
11 Price RW, Brew B, Sidtis J, et al: The brain in AIDS: central nervous system HIV-1 infection and AIDS dementia complex. Science 1988; 239:586–592Crossref, Medline, Google Scholar
12 Bornstein RA, Nasrallah HA, Para MF, et al: Neuropsychological performance in asymptomatic HIV infection. J Neuropsychiatry Clin Neurosci 1992; 4:386–394Link, Google Scholar
13 Dohrenwend BS, Krasnoff L, Askenasy AR, et al: Exemplification of a method for scaling life events: the PERI Life Events Scale. J Health Soc Behav 1978; 19:205–229Crossref, Medline, Google Scholar
14 Brown SA, Vik PW, McQuaid JR, et al: Severity of psychosocial stress and outcome of alcoholism treatment. J Abnorm Psychol 1990; 99:344–348Crossref, Medline, Google Scholar
15 Skodol AD, Shrout PE: Use of DSM-III axis IV in clinical practice: rating etiologically significant stressors. Am J Psychiatry 1989; 146:61–66Crossref, Medline, Google Scholar
16 Sapolsky R: Stress, the Aging Brain and the Mechanisms of Neuron Death, in Behavioral Endocrinology, Edited by Becker JB, Breedlove SM, Crews D. Cambridge, MIT Press, 1992, pp 287–324Google Scholar
17 Galletly C, Clark CR, McFarland AC, et al: Working memory in posttraumatic stress disorder: an event-related potential study. J Trauma Stress 2001; 14:295–309Crossref, Medline, Google Scholar
18 Sachinvala N, von Scotti H, McGuire M, et al: Memory, attention, function, and mood among patients with chronic posttraumatic stress disorder. J Nerv Ment Dis 2000; 188:818–823Crossref, Medline, Google Scholar
19 Green JE, Saveanu R, Bornstein RA: The effect of previous alcohol abuse on cognitive function in HIV infection. Am J Psychiatry 2003 (in press)Google Scholar



