Comparison of Extrapyramidal Signs in Dementia With Lewy Bodies and Parkinson's Disease
Abstract
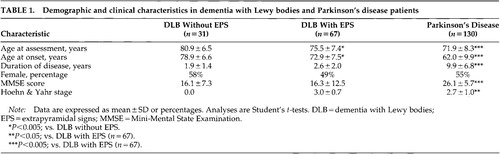
Extrapyramidal signs (EPS) were compared in 98 dementia with Lewy bodies (DLB) and 130 medication-responsive Parkinson's disease (PD) patients. DLB patients were older at assessment and at disease onset, were cognitively more impaired, and had a shorter duration of disease than PD patients. Sixty-seven DLB patients (68%) showed EPS. The 58 DLB patients with complete data had more severe action tremor, body bradykinesia, difficulty arising from a chair, and facial expression, gait, and rigidity symptoms than PD patients (all P<0.001). Abnormal posture and tremor at rest did not differ. Severity of EPS correlated with age, duration of disease, and cognitive impairment in PD patients but not in DLB patients. Studies of the clinical significance and management of EPS in DLB patients are needed.
Dementia with Lewy bodies (DLB) accounts for about 20% of dementia cases and is characterized by dementia, fluctuating cognition, extrapyramidal signs (EPS), and visual hallucinations.1 The literature on the clinical features in DLB has focused mainly on the psychiatric and cognitive symptoms, whereas less is known regarding the severity and characteristics of EPS. There is no consensus regarding the proportion of DLB patients with EPS; the reported rates of EPS range from 45%2 to 100%.3
There are several possible reasons for these reported variations in the prevalence of EPS. First, DLB is a neurodegenerative disease involving both cortical and subcortical brain regions,1 and variations in the regional distribution of pathology and the corresponding clinical presentations might be expected. Second, most studies have included samples too small to be fully representative of the general DLB population. Given the clinical variation, large samples are needed to establish the frequency of clinical features in DLB. Third, because motor, cognitive, and psychiatric symptoms occur, DLB patients are referred to neurological, geriatric, or psychiatric centers. Selection bias may therefore occur. Fourth, the methods of assessing EPS have varied. In some studies, retrospective studies of case notes have been used,4 and quantitative methods to assess EPS usually were not employed. Finally, there is considerable diagnostic overlap between DLB and PD, and some DLB patients are misdiagnosed as having PD.5 To compare the clinical features in DLB and PD patients, diagnostic criteria of PD with a high specificity should be used.
PD is the most common neurological basal ganglia disease, with a prevalence of 1% in those over 65 years.6 Both DLB and PD are part of the spectrum of Lewy body disease, and dementia and hallucinations are common in both. The nosological distinction between PD and DLB is complex and not yet fully resolved. It is suggested that patients presenting with EPS one year before dementia and hallucinations should receive a diagnosis of PD with dementia, although this time frame is somewhat arbitrary.1 Comparison of the clinical features of PD and DLB would potentially help in the clinical and nosological differentiation between the two diseases.
To overcome some of the limitations of previous investigations, we designed a study to compare the frequency and severity of EPS in two large and representative samples of patients with clinical probable DLB1 and clinical definite PD.6 Postmortem confirmation of diagnosis was obtained for 33% of DLB cases. Published diagnostic criteria with high specificity were employed,1,7 and EPS were evaluated prospectively by using a validated and reliable rating instrument, the Unified Parkinson's Disease Rating Scale (UPDRS).8 A modified version, shown to provide a reliable and generally applicable instrument for the assessment of parkinsonism in DLB patients,9 was used in this study.
METHODS
Case Ascertainment and Clinical Diagnosis
DLB Patients:
DLB patients were recruited via two routes. A specialist outpatient clinic invited potential DLB case referrals from psychiatrists, neurologists, and geriatricians covering a wide geographical area (northeast England). The second source was consecutive referrals to an old-age psychiatry service responsible for assessing dementia presentations from a catchment area population of 100,000 people over 65 years of age living in Tyneside. Patients were eligible for the study if they met relevant diagnostic criteria, were not severely demented at baseline (Mini-Mental State Examination10 [MMSE] score>8), had a reliable informant, and gave appropriately informed consent. To maximize the diagnostic differentiation between the DLB and the PD groups, DLB cases with parkinsonism before dementia were excluded.
Clinical diagnosis was made after comprehensive multidisciplinary assessment. The DLB Consensus criteria1 were published during the initial recruitment phase of the study and were substituted for the original Newcastle criteria. All DLB study diagnoses were therefore made by using Consensus criteria. Next of kin were approached at study entry and asked to indicate their intention to consent to brain autopsy at the time of the subject's death.
Clinical diagnoses were reviewed after death and before neuropathological diagnosis was available. All clinical data, including research assessments and clinical charts, were made available to three independent raters, who listed the clinical diagnoses made and checked that patients had indeed fulfilled criteria. The raters' decisions were compared and a primary research clinical diagnosis assigned to each case. Disagreements were resolved by majority verdict. Only probable or autopsy-confirmed DLB cases were included in this study.
Neuropathological examinations (performed in 33% of the DLB cases) followed previously described protocols, and the neuropathological diagnosis of DLB was made according to the International Consensus criteria.1
PD Patients:
The PD population was drawn from the 220,000 inhabitants in the southern part of Rogaland county, Western Norway.6 A diagnostic classification defining clinical definite, probable, and possible PD was used.7 To achieve high diagnostic specificity, we included only the definite PD cases in this study. A definite PD diagnosis requires that a patient has resting tremor and at least two more cardinal signs: 1) akinesia or bradykinesia, 2) rigidity, or 3) postural abnormalities. Unilateral onset and asymmetrical development of disease are required, as well as a good to excellent response to a dopaminergic agent. Early dementia or autonomic failure, or hallucinations within the first 2 years after disease onset, were not compatible with a diagnosis of definite PD. Other neurological diagnoses or current or previous use of neuroleptic drugs would exclude a diagnosis of PD, and no clinically significant changes on computed tomographic or magnetic resonance imaging scans should be present. During a follow-up evaluation 4 years later, a diagnostic reevaluation was performed. Only patients who fulfilled a diagnosis of clinical definite PD on both occasions were included. Further details of the case-finding and diagnostic procedures have been published elsewhere.6
Assessment
The assessment included a standardized physical examination with completion of the UPDRS motor scale to assess extrapyramidal signs. EPS were staged by using the Hoehn and Yahr scale.11 Several UPDRS items are closely related to the severity of cognitive impairment and are therefore difficult to assess reliably in patients with dementia.8 A 5-item subscale that has been shown to provide a reliable and generally applicable instrument for the assessment of parkinsonism in DLB patients8 was used in this study. The subscale consists of the UPDRS items facial expression, rigidity, body bradykinesia, tremor at rest, and action tremor (4 points per item). Each item was scored for the most severely affected limb. In addition, the items for difficulty arising from chair, gait, and posture characteristics were included, since it was felt that these items could also be reliably assessed. Stage 1 or higher on the Hoehn and Yahr scale was taken to indicate a significant level of parkinsonism, and a UPDRS score of 2 or more on each item was taken to identify individual UPDRS signs, since inclusion of mild signs would compromise interrater reliability.12 A cognitive screening instrument, the MMSE,10 was also administered.
Statistical Analyses
Because UPDRS scores were not normally distributed, nonparametric analyses (Spearman rank correlation and Mann-Whitney test) were used. Normally distributed data were analyzed by using Pearson correlations and Student's t-test. Proportions were compared by using the chi-square test or the gamma test for linear associations. A statistical significance level of 0.05 was chosen for most analyses. For the correlation analyses, a statistical significance level of 0.005 was chosen because multiple analyses would be performed. For all analyses, tests were two-tailed.
RESULTS
Prevalence of Extrapyramidal Signs in DLB
Ninety-eight DLB and 130 definite PD patients were included. Sixty-seven DLB subjects (68%) had a Hoehn and Yahr stage score of 1 or higher, whereas 31 (32%) did not have EPS. Three of those without EPS were being treated with levodopa, indicating previous EPS. The clinical and demographic characteristics of the patients are shown in Table 1. DLB patients with EPS were younger, had an earlier onset of disease, and showed a nonsignificant trend toward a higher proportion of men than those without EPS (Table 1). Nine DLB patients without EPS (29%) and 25 with EPS (37%) had autopsy-confirmed DLB, and nigral cell loss was assessed in 23 DLB patients. A significant association between severity of nigral loss and the Hoehn and Yahr stage in this subgroup was found (gamma=0.8, P<0.001).
Extrapyramidal Signs in DLB and PD
In the subsequent analyses, only the DLB patients with EPS were included. When contrasted with the PD patients, DLB patients with EPS were older, were cognitively more impaired, and had both a later disease onset and a shorter duration of disease (Table 1). Nine patients had had incomplete UPDRS ratings, and thus 58 DLB patients were included in the analyses of EPS.
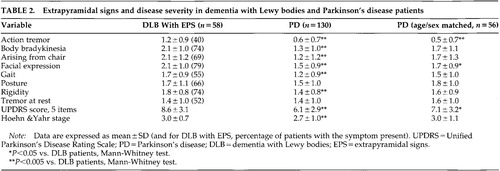
DLB patients with EPS had higher Hoehn and Yahr and UPDRS 5-item scale scores than the PD patients (Table 2). The severity of action tremor, body bradykinesia, difficulty arising from chair, facial expression, gait, and rigidity were higher in DLB than PD patients. Severity of abnormal posture and tremor at rest did not differ (Table 2).
In DLB patients, UPDRS and Hoehn and Yahr scores did not correlate with MMSE score, age, age at onset, or duration of disease. Nonsignificant correlations were found between body bradykinesia and current age (r=–0.28, P=0.04) and age at onset (r=–0.24, P=0.07), and between MMSE score and Hoehn and Yahr stage (r=–0.25, P=0.06) and difficulty arising from chair (r=–0.24, P=0.07). In the PD group, increasing age, longer duration of disease, and low MMSE score correlated significantly with increased severity of most EPS measures (all P<0.005).
To adjust for the demographic differences between DLB and PD patients, 56 of the DLB patients were matched on a one-to-one basis with a PD patient according to age (±2 years) and sex. A matching PD patient was not found for 2 of the oldest female DLB patients. The age- and sex-matched PD patients had an earlier age at onset, longer disease duration, and higher MMSE score than the 56 DLB patients (all P<0.001). The overall level of EPS as measured by Hoehn and Yahr stage was similar in DLB and the age- and sex-matched PD patients, but DLB patients had a higher UPDRS 5-item sumscore than PD patients. DLB patients had higher scores on action tremor and facial expression, whereas no significant between-group differences were found on the other UPDRS items (Table 2).
Use of Medications
All PD patients received at least one dopaminergic agent, compared with 40 (60%) of the DLB patients with EPS (χ2=60.1, df=1, P<0.001). When only patients taking antiparkinsonian agents were included, Hoehn and Yahr stage was higher in DLB patients (mean=3.2, SD=0.6) than in PD patients (mean=2.7, SD=1.0; U=1,625, P<0.001). Eleven (16%) of the DLB patients were treated with a traditional antipsychotic agent, as compared with 8 (6%) of the PD patients (χ2=5.3, df=1, P<0.05). Sixteen (20%) of the DLB patients had previously received an antipsychotic agent. Six DLB patients (9%) but no PD patients were treated with an atypical antipsychotic (risperidone or clozapine; χ2=12.0, df =1, P=0.001). Nine (13%) of the DLB patients had previously received such an agent.
Severity of EPS as measured with the Hoehn and Yahr scale did not differ between DLB patients ever exposed to traditional or atypical antipsychotics (mean score=3.0, SD=0.6) and those who had never received such agents (mean score=3.0, SD=0.6; P=0.6).
DISCUSSION
The findings in this study demonstrate that extrapyramidal signs are common in DLB patients. In DLB patients with EPS, most EPS assessed were more severe than those in PD patients. Thus, these findings do not support the previous assumptions that EPS are usually mild in DLB patients,1 but findings are consistent with previous studies using smaller samples3 and retrospective assessment.4 On the other hand, 32% of DLB patients, one-third of whom had the diagnosis confirmed at autopsy, did not have significant EPS. Accordingly, DLB can be diagnosed also in the absence of EPS.
Methodological factors may have influenced the assessment of EPS in DLB. The first and most important of these relates to sampling. The PD group were epidemiologically based and therefore represent the full spectrum of severity, from very mild and early cases to endstage disease. The DLB group, on the other hand, were referrals to a tertiary clinical service with a potential bias for more severely affected cases to be included and early presentations excluded. Second, DLB patients were older and included more men than PD, characteristics that might influence the severity of EPS;13 however, after matching for age and sex, the DLB patients still had more severe EPS than the PD cases. Third, only PD patients with a good response to levodopa were included, and thus the difference in EPS between DLB and PD patients may be entirely accounted for by a differential response to antiparkinsonian medications. Fourth, the proportion of patients who were currently taking or had previously received neuroleptics was higher in the DLB than in the PD patient group. Medication history thus may have contributed to the prevalence and severity of EPS in DLB patients, although our results suggested that this was not the case.
Data on reliability between centers were not available. Rater variability could therefore influence the principal observations in this study, although raters from different countries can obtain a high rate of agreement in UPDRS scoring despite differences in culture, economics, health systems, and medical standards.14 It is also possible that PD patients would show more impairment on some of the UPDRS items not assessed in this study. The truncated version of the UPDRS may thus have underestimated the extent of EPS in the PD group. Finally, the Hoehn and Yahr scale does not have the same meaning for PD and for DLB. PD patients usually have a unilateral onset of EPS, and would thus be rated at Hoehn and Yahr stage 1. DLB patients usually begin with bilateral EPS, leading to a Hoehn and Yahr stage of 2, although this does not necessarily mean that they have more severe EPS.
An additional factor relates to diagnostic accuracy for PD and DLB. Some DLB patients may be misdiagnosed as having PD and vice versa.5 The risk for diagnostic overlap may be increased because PD and DLB patients were diagnosed at two different centers. However, we took care to avoid this. First, only DLB patients with dementia at least one year prior to EPS were included, and one-third of the DLB patients had their diagnosis confirmed at autopsy. Second, only PD patients with EPS before occurrence of cognitive impairment were included. Third, surviving PD patients (75% of the population) were followed for 4 years without evidence of diagnoses other than PD. Finally, we used conservative criteria for PD that have demonstrated a diagnostic specificity for PD of more than 90%.15
The major methodological strength of this study is its large and representative patient samples. The PD group were community-based with a high case ascertainment,6 and the DLB cohort constitutes one of the largest DLB cohorts reported. Moreover, EPS were assessed with standardized and validated instruments, and care had been taken to include only items that could provide reliable and valid assessments of EPS in DLB.
The neuropathological and neurochemical correlates of extrapyramidal signs in DLB remain to be determined. In vivo studies have demonstrated nigrostriatal degeneration in DLB patients,16 and an association between nigral cell loss and EPS was found in the subgroup of DLB patients with autopsy in the current study. However, cell loss in the substantia nigra is less pronounced in DLB than in PD,17,18 and in a recent study no association between nigral cell loss and severity of parkinsonism was found.19 Thus, mechanisms other than nigral cell loss seem to contribute to EPS in DLB. Cell loss in the striatum may provide an explanation, but we have no morphological evidence for this to date. The residual substantia nigra neurons do not seem to have the same capacity for presynaptic increase in dopamine turnover in DLB patients as in PD patients.18 When combined with low postsynaptic dopamine D2 receptors, this could result in greater motor deficits in DLB for the equivalent dopamine loss in PD, which has both presynaptic and postsynaptic compensatory mechanisms.18 Alternatively, alpha-synuclein pathology in the striatum, or abnormalities in the input of the cholinergic pedunculopontine nucleus to the substantia nigra, may contribute to EPS in DLB. These hypotheses might also explain preliminary reports of the attenuated response to dopaminergic therapy in DLB compared with PD,20 although the majority of DLB patients do seem to have some response to such therapies.3,4
We found that 68% of a large sample of DLB patients had extrapyramidal signs. Among those DLB patients who exhibited EPS, most symptoms were more severe than in PD patients. To further explore this finding, future studies should compare EPS in medication-naïve PD and DLB patients. Although cognitive impairment and neuropsychiatric symptoms may be the most striking features of dementia with Lewy bodies, the functional impairment caused by severe EPS needs to be addressed and managed. Clinical trials of antiparkinsonian agents in DLB are therefore urgently needed.
 |
 |
1 McKeith IG, Galasko D, Kosaka K, et al: Consensus guidelines for the clinical diagnosis of dementia with Lewy bodies (DLB): report of the Consortium on DLB International Workshop. Neurology 1996; 47:1113-1124Google Scholar
2 McKeith I, Fairbairn A, Perry R, et al: Neuroleptic sensitivity in patients with senile dementia of the Lewy body type. BMJ 1992; 35:673-678Crossref, Google Scholar
3 Gnanalingham KK, Byrne EJ, Thornton A, et al: Motor and cognitive function in Lewy body dementia: comparison with Alzheimer's and Parkinson's diseases. J Neurol Neurosurg Psychiatry 1997; 62:243-252Crossref, Medline, Google Scholar
4 Louis ED, Klatka LA, Liu Y, et al: Comparison of extrapyramidal features in 31 pathologically confirmed cases of diffuse Lewy body disease and 34 pathologically confirmed cases of Parkinson's disease. Neurology 1997; 48:376-380Crossref, Medline, Google Scholar
5 Litvan I, MacIntyre A, Goetz CG, et al: Accuracy of the clinical diagnoses of Lewy body disease, Parkinson's disease, and dementia with Lewy bodies. Arch Neurol 1998; 55:969-978Crossref, Medline, Google Scholar
6 Tandberg E, Larsen JP, Nessler EG, et al: The epidemiology of Parkinson's disease in the county of Rogaland, Norway. Mov Disord 1995;10:541-549Google Scholar
7 Larsen JP, Dupont E, Tandberg E: The clinical diagnosis of Parkinson's disease: proposal of diagnostic subgroups classified at different levels of confidence. Acta Neurol Scand 1994; 84:242-251Google Scholar
8 Fahn S, Elton RL, and members of the UPDRS Development Committee: Unified Parkinson's Disease Rating Scale, in Recent Developments in Parkinson's Disease, edited by Fahn S, Marsden CD, Calne DB, et al. Florham Park, NJ, Macmillan Health Care Information, 1987, pp 153-163Google Scholar
9 Ballard C, McKeith I, Burn D, et al: The UPDRS scale as a means of identifying extrapyramidal signs in patients suffering from dementia with Lewy bodies. Acta Neurol Scand 1997; 96:366-371Crossref, Medline, Google Scholar
10 Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the mental state of patients for the clinician. J Psychiatr Res 1975; 12:189-198Crossref, Medline, Google Scholar
11 Hoehn MH, Yahr MD: Parkinsonism: onset, progression, and mortality. Neurology 1967; 17:427-442Crossref, Medline, Google Scholar
12 Richards M, Marder K, Bell K, et al: Interrater reliability of extrapyramidal signs in a group assessed for dementia. Arch Neurol 1991; 48:1147-1149Google Scholar
13 Bennett DA, Beckett LA, Murray AM, et al: Prevalence of parkinsonian signs and associated mortality in a community-based population of older people. N Engl J Med 1996; 334:71-76Crossref, Medline, Google Scholar
14 Althaus M, Jorg J, for The European DHEC Study Group: Interrater reliability of the UPDRS motor score in an international multicentre trial. J Neurol 1999; 246(suppl 1):1/153Google Scholar
15 Hughes AJ, Ben-Shlomo Y, Daniel S, et al: What features improve the accuracy of clinical diagnosis in Parkinson's disease: a clinico-pathologic study. Neurology 1992; 42:1142-1146Google Scholar
16 Walker Z, Costa DC, Ince P, et al: In-vivo demonstration of dopaminergic degeneration in dementia with Lewy bodies. Lancet 1999; 354:646-647Crossref, Medline, Google Scholar
17 Piggot MA, Marshall EF, Thomas N, et al: Striatal dopaminergic markers in dementia with Lewy bodies, Alzheimer's and Parkinson's disease: rostrocaudal distribution. Brain 1999; 122:1449-1468Google Scholar
18 Perry RH, Irving D, Blessed G, et al: Senile dementia of Lewy body type: a clinically and neuropathologically distinct type of Lewy body dementia in the elderly. J Neurol Sci 1990; 95:119-139Crossref, Medline, Google Scholar
19 Ala TA, Yang KH, Sung JH, et al: Clinical parkinsonism in dementia with substantia nigra Lewy bodies. J Neural Transm 1999; 106:47-57Crossref, Medline, Google Scholar
20 Mark MH, Sage JI, Dickson DW, et al: Levodopa-nonresponsive Lewy-body parkinsonism: clinicopathologic study of two cases. Neurology 1992; 42:1323-1327Google Scholar