Symptoms of Delirium Among Elderly Medical Inpatients With or Without Dementia
Abstract
This study examined the frequencies of the 10 symptoms of delirium identified in DSM-III-R among patients with delirium (DSM-III-R criteria) who did or did not have dementia. The prevalence of each symptom, the numbers of symptoms, and the combinations of symptoms were determined among 322 elderly medical inpatients classified into one of four groups: delirium and dementia (n=128), delirium only (n=40), dementia only (n=94), or neither (n=60). Symptoms were assessed at the time of diagnosis and independently (by use of a different scale) within 24 hours of diagnosis. Delirium appeared to be phenomenologically similar among patients with and those without dementia, although patients with dementia had more psychomotor agitation at the time of diagnosis and more disorganized thinking and disorientation at the second assessment.
Delirium is a cognitive disorder characterized by acute onset, a fluctuating course, an altered level of consciousness, and disturbances in orientation, memory, attention, thinking, perception, and behavior.1 It occurs in 11% to 26% of older hospitalized medical inpatients2–5 and appears to be associated with significant increases in length of hospital stay, rates of institutionalization, functional disability, and rates of death.6
In elderly persons, dementia is the most common risk factor for delirium.7 Consequently, there are problems in determining which symptoms are due to delirium and which to dementia. Using the Delirium Rating Scale (DRS, based on DSM-III criteria), Trzepacz et al.8 scored the severity of symptoms of delirium in hospital inpatients, 20 with delirium (ages 28–83; mean age 59), 9 with dementia (ages 70–84; mean age 78), and 9 with neither (ages 28–62; mean age 42). They reported no overlap in the distribution of DRS scores between groups. This scale has since been validated by two other research groups using DSM-III-R criteria to diagnose delirium and dementia.9,10
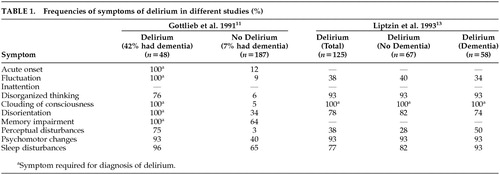
Gottlieb et al. (Table 1),11 using operationalized criteria for DSM-III symptoms of delirium, compared the frequency of symptoms of delirium in two groups of elderly medical inpatients, 48 with delirium (20 of whom had a previous diagnosis of dementia) and 187 without delirium (13 of whom had a previous diagnosis of dementia). By definition, clouding of consciousness, disorientation, memory impairment, fluctuation, and acute onset were present in 100% of patients with delirium; the same symptoms were present in 5%, 34%, 64%, 9%, and 12%, respectively, of patients without delirium. Similarly, perceptual disturbances, incoherent speech, sleep disorder, and psychomotor changes occurred in 75%, 76%, 96%, and 93%, respectively, of delirious patients and 3%, 6%, 65%, and 40%, respectively, of nondelirious patients.
Using the Delirium Symptom Interview (DSI),12 Levkoff et al.5 examined elderly hospitalized patients and identified 125 cases that met DSM-III criteria for delirium. Interrater agreement (kappa) for individual symptoms on the DSI ranged from 0.31 to 1.0.12 Liptzin et al.13 (Table 1) reexamined the data (collected independently of the diagnostic process) for these 125 cases to determine the frequency of symptoms of delirium among patients with (n=58) or without (n=67) dementia. Disturbances in orientation, consciousness, sleep, perception, speech, and psychomotor activities, and fluctuating behavior, occurred in 82%, 100%, 82%, 28%, 43%, 93%, and 40%, respectively, of delirious patients without dementia and 74%, 100%, 71%, 50%, 95%, 93%, and 34%, respectively, of delirious patients with dementia; the authors concluded that delirium may not be phenomenologically different in patients with and without dementia.
The most recent study14 compared mean item scores on the DRS between 18 elderly inpatients with delirium alone and 43 with delirium superimposed on dementia. The DRS was completed blind to diagnosis. Only one mean item score, cognitive impairment, was significantly different (greater in the group with dementia) between the groups. In the same study, an exploratory principal components analysis of DRS items identified 7 out of 10 delirium symptoms as comprising two core factors that were similar for the two groups. However, three symptoms (hallucinations, cognitive impairment, variability of symptoms) loaded onto opposite factors in the two groups.
To date, the evidence on the frequency of symptoms of delirium among patients with or without dementia is limited in six ways. First, most studies included relatively small numbers of cases with delirium and/or dementia.8,11,14 Second, most studies did not assess the reliability and validity of the measurement of individual delirium symptoms.8,11,14 Third, two of the studies did not assess the frequency of symptoms independent of the diagnostic process.8,11 Fourth, three of the studies did not report the frequency of delirium symptoms among delirious patients with or without dementia.8,11,14 Fifth, the frequencies of symptoms in the two studies that reported them differed substantially (Table 1).11,13 Sixth, none of the studies reported the frequencies of symptoms among delirious patients with or without dementia and in comparable but nondelirious patients with or without dementia. Thus, the purpose of this study was to examine the prevalence and patterns of symptoms of delirium among elderly delirious medical inpatients with or without dementia, using two different reliable and valid symptom measures: the Confusion Assessment Method completed by a screening nurse to diagnose delirium, and the Delirium Index completed by a research assistant to rate the severity of delirium, independent of the diagnostic process.
METHODS
Study Design
The study is a secondary analysis of data collected in two concurrent studies on delirium: a randomized controlled trial of management of delirium and a nonexperimental prospective study of the prognosis of delirium that included nondelirious subjects. The study was conducted at St. Mary's Hospital, a 400-bed primary acute care university-affiliated hospital in Montreal. A study nurse (SN) was responsible for patient screening and enrollment in the two studies. Only patients age 65 and over who were admitted from the emergency department to the medical services were included in the studies. We excluded patients with a primary diagnosis of stroke; those admitted to the oncology unit; those admitted to the intensive care unit (ICU) or cardiac monitoring unit (CMU) unless they were transferred to a medical ward within 48 hours of admission; and those who did not speak English or French.
The study nurse administered the Confusion Assessment Method (CAM)15 to those whose initial score on the Short Portable Mental Status Questionnaire (SPMSQ)16 was 3 or more (see Measures section), or whose nursing notes indicated symptoms of delirium. The SN used various data sources to complete the CAM (chart, family, nursing staff) and assessed the patient at several timepoints, if necessary. Delirium was diagnosed if the patient met DSM-III-R criteria for delirium.17 Those whose initial SPMSQ score was less than 3, or who scored 3 or more but were negative on the CAM, were rescreened with the SPMSQ daily for the following week. The CAM was readministered if the SPMSQ score increased or there was evidence from the nursing notes of symptoms of delirium.
Nondelirious subjects were selected from patients screened for delirium but free of this condition. In order to balance the distributions of age and prior cognitive impairment among patients with and without delirium, the sampling method for nondelirious patients took into account the patient's age and initial SPMSQ score. Thus, nondelirious subjects were selected from patients age 70 and over, and only a subsample of patients with SPMSQ scores of less than 3 were included.
Prior to enrollment, patients with delirium and/or dementia were asked for assent to participate in the study and a family member was asked for informed consent; cognitively intact patients were asked for informed consent.
The Delirium Index (DI)18 and the IQCODE19 were completed by a research assistant (RA) within 24 hours of the diagnosis. For completion of the DI, the RA had no knowledge of the patient's diagnosis and had been trained only to rate the presence and severity of the seven symptoms on the DI based on assessment of the patient at one point in time.
Other measures completed by the SN or RA included Clinical Severity of Illness,20 Mini-Mental State Examination (MMSE),21 Barthel Index (BI),22 and premorbid OARS Instrumental Activities of Daily Living.23
Measures
The SPMSQ16 is a widely used, observer-rated, 10-item questionnaire that evaluates orientation, memory, and concentration. Scale scores (based on the number of errors) range from 0 (no impairment) to 10 (severe impairment). The test-retest reliability is reported to be 0.8.16 At a cutoff point of three or more errors, the instrument is reported to have a sensitivity of 0.84 and a specificity of 0.89 in identifying medical inpatients with organic brain syndromes.24
The CAM15 is a structured instrument that operationalizes the 10 symptoms of delirium specified in the DSM-III-R: acute onset, fluctuating course, inattention, disorganized thinking, altered level of consciousness, disorientation, memory impairment, perceptual disturbances, psychomotor agitation or retardation, and sleep/wake disturbance. The CAM diagnosis of delirium (based on DSM-III-R criteria) was validated against the clinical judgment of a psychiatrist and found to have a sensitivity of 97% and a specificity of 92%.15 In the present study, the SN diagnosis of delirium had a sensitivity of 0.89 and a specificity of 1.0 compared with a consensus diagnosis involving psychiatrists.25 In an earlier study,26 interrater agreement (kappa) for the individual symptoms of delirium ranged from 0.64 to 1.0 (n=11), and in the present study, from 0.28 to 1.0 (n=14). The earlier study included only severe and typical cases of delirium, whereas the present study included a broader range of cases; hence the lower kappa values.
The DI18 is an instrument developed by our group for the measurement of the severity of symptoms of delirium. It is based solely on observation of the individual patients, without additional information from family members, nursing staff, or the patient's medical chart. The first five questions of the MMSE21 comprise the minimum basis of observation. Seven of the 10 symptoms assessed on the CAM (including disorders of attention, thought, consciousness, orientation, memory, perception, and psychomotor activity but excluding acute onset, fluctuation, and sleep-wake disturbance) are rated on the following impairment scale: 0=absent, 1=mild, 2=moderate, 3=severe. The total score ranges from 0 (no symptoms) to 21 (maximum severity). Patients who are unresponsive are scored at maximum severity on inattention, disorganized thinking, disorientation, and memory impairment. We established the interrater reliability, concurrent criterion validity, and sensitivity to change of the DI in 30 patients with delirium who were rated simultaneously and independently by one or two research assistants and a geriatric psychiatrist on up to four occasions. The concordance coefficient between DI ratings by a psychiatrist and a research assistant was 0.81, and between two research assistants, 0.71. Pearson correlation coefficients were 0.84 between the DI and the Delirium Rating Scale (DRS), and 0.71 between change in the DI and change in the DRS. The interrater agreement (kappa) for the individual symptoms of delirium in the present study ranged from 0.43 to 0.80 (n=43).
The IQCODE19 assesses the presence of dementia prior to admission based on the responses of an informant who has known the patient for at least 5 years; the score is an average of the 16-item scores, each rated from 1 (much improved) to 5 (much worse). In the original publication,19 using a cutoff of 3.32 or more to identify patients with dementia, the sensitivity was 0.79 and the specificity was 0.82. In a later validation study of a French version of the questionnaire conducted in Quebec,27 a cutoff of 3.6 or more had a sensitivity of 0.75 and a specificity of 0.96. On the basis of the distribution of scores in our population, we used a cutoff of 3.51 or more to identify patients with dementia.
Clinical Severity of Illness20 was assessed at baseline by the SN; scores range from 1 (minimal) to 9 (most severe). The Mini-Mental State Examination (MMSE)21 measures cognitive function on a scale of 0 (poor) to 30 (excellent). The Barthel Index22 measures independence in personal care activities; we used a modified scoring system28 that ranged from 0 (dependent) to 100 (independent). The OARS Instrumental Activities of Daily Living questionnaire23 was administered to an informant to assess premorbid function (prior to current illness but not more than one month before admission); the scale score ranges from 0 (dependent) to 16 (independent).
Statistical Analysis
Patients were classified into four different groups based on their delirium and dementia diagnosis: 1) both delirium and dementia, 2) delirium only, 3) dementia only, and 4) neither delirium nor dementia. Descriptive statistics of patients' demographic and clinical characteristics were obtained separately within the four groups.
To study the distribution of symptoms within each group, we used three different approaches. First, we estimated the prevalence of each symptom, separately for the CAM and DI scales, within the four patient groups. Among patients with delirium, those with and without dementia were compared based on the difference in the prevalence of each symptom (and the associated 95% confidence interval). Similarly, the difference in symptom prevalence attributable to delirium was examined among patients with and without dementia. Next, we compared the difference in the numbers of symptoms of delirium in the four groups based on the seven symptoms that were common between the CAM and DI scales, separately for each scale.
Finally, we used cluster analysis to study whether there were patient subgroups defined by different combinations of delirium symptoms (assessed by the DI) within the groups with delirium/dementia and delirium only. The cluster analysis was based on the “partitioning around medoids (PAM)” approach,29 which partitions the data into a predetermined number of clusters based on a dissimilarity criterion. The dissimilarity between each pair of patients on the DI scale was measured by using the Euclidean distance. To implement the cluster analysis we first randomly divided each patient group into two samples of equal size and then identified 2, 3, or 4 clusters in each sample by using PAM. By comparing the “medoids” or central values of different clusters between the two samples we were able to verify the validity of the clusters. Once the number of clusters was ascertained, PAM was used to determine the cluster membership for the entire patient group. Within clusters, we estimated a mean severity score for each symptom as the mean DI score for that symptom. We also estimated the mean (and 95% confidence interval) of demographic and clinical characteristics within each cluster. We did not use cluster analysis to study CAM symptoms because we believed that the resulting clusters would be determined by the symptoms required for the diagnosis of delirium. All statistical analyses were done by using the S-plus software package.30
RESULTS
During the study enrollment period, there were 4,085 medical admissions, of which 1,552 (38.0%) were screened for delirium. The reasons for exclusion were admission to oncology (452), admission to intensive care or coronary care units (377), transfer to long-term care (332), language barrier (301), stroke (289), not sampled or missed (181), refused screening (164), previously enrolled in study (127), transferred or discharged (113), communication problem (105), residence outside geographic area (69), died (20), and other (3). Of the 1,552 patients screened, 187 met DSM-III-R criteria for delirium; 174 nondelirious subjects were also enrolled in the study. We excluded 19 patients with delirium and 20 nondelirious subjects because data on dementia status were missing, leaving 168 delirium cases and 154 nondelirious subjects in the study sample.
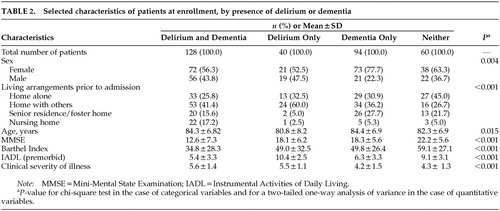
At enrollment, there were significant differences between the four patient groups with respect to age, gender, living arrangements, and the measures of function and severity (Table 2). Patients with delirium only were more likely than patients without delirium to be male and living at home with others. Patients with delirium, with or without dementia, had higher clinical severity and lower BI scores than the two groups without delirium. Patients with dementia only were more likely to be female.
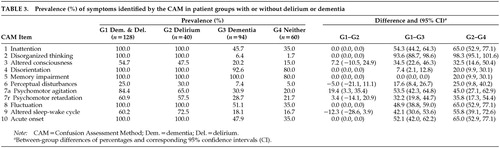
The prevalence of symptoms of delirium in the four groups, as determined by the CAM, is presented in Table 3. Most symptoms of delirium had a similar prevalence in the group with delirium/dementia (G1) as in the group with delirium alone (G2), except for psychomotor agitation, which was significantly more prevalent among patients with delirium/dementia. All symptoms of delirium were significantly more prevalent among patients diagnosed with delirium than patients without delirium, irrespective of the presence of dementia, except for memory impairment, which was present in 100% of dementia patients with or without delirium.
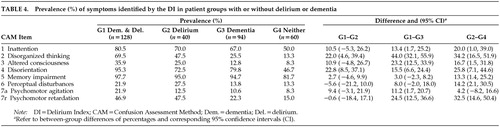
The prevalence of symptoms of delirium as determined by the DI tended to be lower than that determined by the CAM (Table 4). Most symptoms of delirium (except perceptual disturbances and psychomotor retardation) were more prevalent in the delirium/dementia group than in the delirium group, significantly so for disorganized thinking and disorientation. In contrast with the CAM, the symptom prevalence that was attributable to delirium tended to be smaller both among patients with and those without dementia, and it was not always statistically significant.
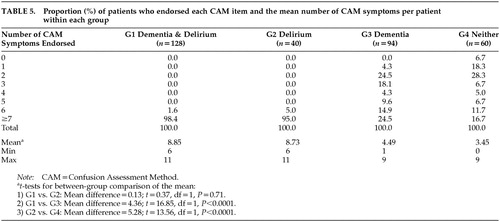
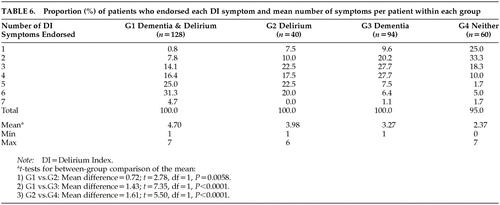
The frequency distributions and the mean number of symptoms as measured by the CAM and DI are presented in Table 5 and Table 6, respectively. For the DI but not the CAM, the mean number of symptoms was significantly higher in the delirium/dementia group than the delirium group (mean difference=0.72, P=0.0058). For both instruments, the mean number of symptoms differed significantly between groups with or without delirium irrespective of the presence of dementia; however, the mean difference in the number of symptoms attributable to delirium was greater for the CAM than the DI, regardless of the presence of dementia.
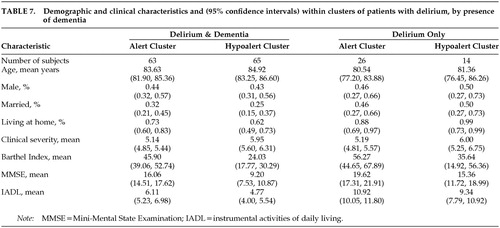
The cluster analysis identified two similar clusters of symptoms on the DI for the delirium/dementia and delirium groups. Figure 1 is a plot of the mean symptom severity score for each symptom within each cluster in the delirium/dementia and delirium-only groups. The clusters separate patients with delirium/dementia in terms of higher mean symptom severity scores for altered consciousness, memory impairment, disorientation, inattention, disorganized thinking, and psychomotor retardation. There are smaller differences between the clusters for patients with delirium only, except that one cluster has greater impairment of consciousness than the other cluster. These two clusters may be defined by level of consciousness as alert (mean DI score 0) or hypoalert (mean DI score 1). Notably, the hypoalert cluster defines a group of patients who have higher severity of illness scores and lower MMSE, Barthel and (premorbid) IADL scores scores in both delirium/dementia and delirium groups, significantly so in the delirium/dementia group (Table 7).
DISCUSSION
This study examined the prevalence and patterns of symptoms of delirium in elderly medical inpatients with or without dementia, using two independent measures. Thus, delirious patients with dementia tended to have more symptoms of delirium than delirious patients without dementia, significantly so for psychomotor agitation on the CAM, disorganized thinking and disorientation on the DI, and the mean number of symptoms on the DI. Symptom clusters distinguished groups of hypoalert patients, particularly among patients with dementia. Thus, delirium appears to be phenomenologically similar among patients with or without dementia, although patients with dementia tend to have more symptoms.
For most symptoms, the frequencies reported in the present study are similar to those reported by Liptzin et al.13 However, fluctuation was two to three times more frequent in the present study and clouding of consciousness was two to three times less frequent. These differences probably reflect how these symptoms were operationalized. In the present study, fluctuation was determined by interview with the patient and a family member, whereas it was determined by patient interview only in the study of Liptzin et al.13 Clouding of consciousness was determined by a positive rating on one item in the present study, whereas it was determined by a positive rating on one of eight items in the Liptzin et al. study.
The differences in results between the CAM and DI may be attributed to three factors. First, the diagnostic process, using the CAM, multiple data sources, and multiple points of observation, was more complete; however, the diagnostic process itself probably exaggerated the differences in the prevalence and mean numbers of symptoms between the patients with and without delirium. Second, when symptoms were determined independent of the diagnostic process (using the DI), there may have been regression toward the mean because more severe symptoms initially would tend to be less severe at the second assessment. Third, the DI was completed within 24 hours of the CAM, although there may have been clinical improvement and actual reduction in the frequencies and numbers of delirium symptoms between measurements.
This study has two strengths. First, the numbers of patients with and without delirium or dementia were relatively large. Second, the symptoms of delirium were rated independently by using two different, valid, and reliable instruments.
This study has six potential limitations. First, the study was a secondary analysis of data collected for a randomized trial and a prognosis study. Second, the sampling method for nondelirious subjects was weighted by SPMSQ score; thus, the symptom prevalences may have been inflated for patients without delirium and particularly for those with neither delirium nor dementia. Third, some symptoms of delirium can be difficult to rate, and consequently the kappa values for some symptoms on the CAM and DI were low; nonetheless, they were similar to values reported in a study using the Delirium Symptom Interview.12 Fourth, we used the IQCODE to determine dementia status. The sensitivity and specificity of this instrument are high, but it has not been validated among patients presenting with delirium; nevertheless, the reported demographic and clinical characteristics were consistent with the classification into the four groups. Fifth, the scoring of the DI for unresponsive patients may have been responsible for the two clusters we identified. And sixth, the results might have differed if DSM-IV criteria had been used to identify delirium.
On the basis of our findings, the 10 symptoms of delirium listed in DSM-III-R17 seem to distinguish well between patients with and those without delirium. Moreover, these symptoms seem to be equally useful whether or not the patient has dementia.
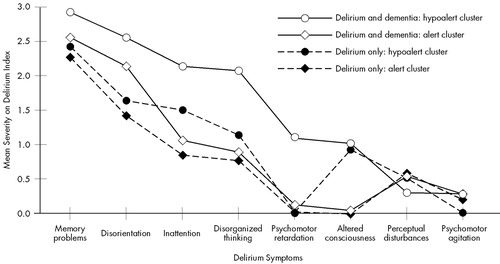
FIGURE 1. Mean symptom severity score within clusters
 |
 |
 |
 |
 |
 |
 |
1 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Washington, DC, American Psychiatric Association, 1994Google Scholar
2 Rockwood K: The occurrence and duration of symptoms in elderly patients with delirium. J Gerontol 1993; 48(4):M162-M166Google Scholar
3 Francis J, Martin D, Kapoor WN: A prospective study of delirium in hospitalized elderly. JAMA 1990; 263:1097-101Crossref, Medline, Google Scholar
4 Jitapunkul S, Pillay I, Ebrahim S: Delirium in newly admitted elderly patients: a prospective study. Q J Med 1992; 300:307-314Google Scholar
5 Levkoff S, Evans D, Liptzin B, et al: Delirium: the occurrence and persistence of symptoms among elderly hospitalized patients. Arch Intern Med 1992; 152:334-340Crossref, Medline, Google Scholar
6 Cole M, Primeau F: Prognosis of delirium in elderly hospital patients. Can Med Assoc J 1993; 149:41-46Google Scholar
7 Elie M, Cole M, Primeau F, et al: Delirium risk factors in elderly hospitalized patients. J Gen Intern Med 1998; 13:204-312Crossref, Medline, Google Scholar
8 Trzepacz, Baker R, Greenhouse J: A symptom rating scale for delirium. Psychiatr Res 1988; 23:89-97Crossref, Medline, Google Scholar
9 Rosen J, Sweet R, Mulsant B, et al: The Delirium Rating Scale in a psychogeriatric inpatient setting. J Neuropsychiatry Clin Neurosci 1994; 6:30-35Link, Google Scholar
10 Rockwood K, Goodman J, Flynn M, et al: Cross-validation of the Delirium Rating Scale in older patients. J Am Geriatr Soc 1996; 44:839-842Crossref, Medline, Google Scholar
11 Gottlieb G, Johnson J, Wanich C, et al: Delirium in the medically ill elderly: operationalizing the DSM-III criteria. Int Psychogeriatr 1991; 3:181-196Crossref, Medline, Google Scholar
12 Albert M, Levkoff S, Reilly C, et al: The Delirium Symptom Interview: an interview for the detection of delirium symptoms in hospitalized patients. J Geriatr Psychiatry Neurol 1992; 5:14-21Crossref, Medline, Google Scholar
13 Liptzin B, Levkoff SE, Gottlieb GL, et al: Delirium. J Neuropsychiatry Clin Neurosci 1993; 5:154-160Link, Google Scholar
14 Trzepacz PT, Mulsant BH, Dew MA, et al: Is delirium different when it occurs in dementia? A study using the Delirium Rating Scale. J Neuropsychiatry Clin Neurosci 1998; 10:199-204Link, Google Scholar
15 Pfeiffer E: A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975; 23:433-441Crossref, Medline, Google Scholar
16 Inouye S, van Dyck C, Alessi C, et al: Clarifying confusion: the Confusion Assessment Method, a new method for detection of delirium. Ann Intern Med 1990; 113:941-948Crossref, Medline, Google Scholar
17 American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, revised. Washington, DC, American Psychiatric Association, 1987Google Scholar
18 McCusker J, Cole M, Bellavance F, et al: Reliability and validity of a new measure of severity of delirium. Int Psychogeriatr 1998; 10:421-433Crossref, Medline, Google Scholar
19 Jorm A: A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): development and cross-validation. Psychol Med 1994; 24:145-153Crossref, Medline, Google Scholar
20 Charlson M, Sax F, Mackenzie R, et al: Assessing illness severity: does clinical judgment work? J Chron Dis 1986; 39:439-452Crossref, Medline, Google Scholar
21 Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189-198Crossref, Medline, Google Scholar
22 Mahoney FI, Barthel DW: Functional evaluation: the Barthel Index. Maryland State Medical Journal 1965; 14:61-65Medline, Google Scholar
23 Fillenbaum G: Multidimensional Functional Assessment: The OARS Methodology: A Manual, 2nd edition. Durham, NC, Center for the Study of Aging and Human Development, Duke University, 1978Google Scholar
24 Erkinjuntti T, Sulkava R, Wikstrom J, et al: Short Portable Mental Status Questionnaire as a screening test for dementia and delirium among the elderly. J Am Geriatr Soc 1987; 35:412-416Crossref, Medline, Google Scholar
25 Zou Y, Cole M, Primeau F, et al: Detection and diagnosis of delirium in the elderly: psychiatrist diagnosis, Confusion Assessment Method or consensus diagnosis? Int Psychogeriatr 1998; 10:303-308Crossref, Medline, Google Scholar
26 Cole M, Primeau F, Bailey R, et al: Systematic intervention for elderly inpatients with delirium: a randomized trial. Can Med Assoc J 1994; 151:965-970Google Scholar
27 Law S, Wolfson C: Validation of a French version of an informant-based questionnaire as a screening test for Alzheimer's disease. Br J Psychiatr 1995; 167:541-154Crossref, Medline, Google Scholar
28 Shah S, Vanclay F, Cooper B: Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 1989; 42:703-709Crossref, Medline, Google Scholar
29 Kaufman L, Rousseeuw PJ: Finding Groups in Data: An Introduction to Cluster Analysis. New York, Wiley, 1990Google Scholar
30 S-Plus 2000 (software package), MathSoft Inc., Seattle, 1999Google Scholar