Emergent Neuroleptic Hypersensitivity as a Herald of Presenile Dementia
Abstract
Neuroleptic hypersensitivity is characteristic of dementia with Lewy bodies (DLB) but not of other dementias. The authors report 5 patients with psychotic mood disorders and long-standing antipsychotic drug therapy. As they reached 50 to 60 years of age, they unexpectedly developed hypersensitivity to these medications, with rigidity, muteness, or the neuroleptic malignant syndrome. Nearly coincident with this reaction, they developed progressive cognitive deficits consistent with frontotemporal dementia. These patients illustrate emergent neuroleptic hypersensitivity as an early manifestation of other dementias. The predisposition to neuroleptic hypersensitivity could result from depleted nigral dopaminergic neurons suggested by “smudging” of the substantia nigra pars compacta on magnetic resonance imaging.
After Alzheimer's disease (AD), the most common neurodegenerative dementias are dementia with Lewy bodies (DLB) and frontotemporal dementia (FTD).1 The exact percentages are unclear, but AD accounts for 45 to 75 percent of all dementias, DLB for at least 20 percent, and FTD for up to 10 percent.1 One of the features that distinguishes DLB is neuroleptic hypersensitivity.2–4 Up to 81 percent of carefully diagnosed DLB patients may manifest neuroleptic sensitivity, ranging from a mild extrapyramidal syndrome to the neuroleptic malignant syndrome (NMS).2 Other features of DLB include dementia with fluctuations in cognition, visual hallucinations, and parkinsonism. FTD, on the other hand, is not characterized by neuroleptic sensitivity but by personality changes and executive dysfunction.5 FTD is the most common cause of a neurodegenerative dementia in the presenium (less than 65 years of age).5,6
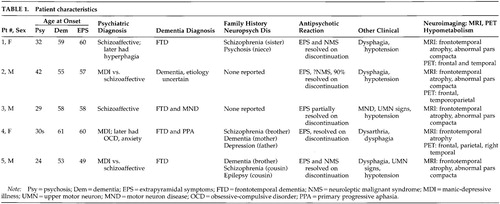
This report describes the emergence of neuroleptic hypersensitivity in five patients after decades of prior antipsychotic treatment, along with the development of a presenile dementia more characteristic of FTD than of DLB. Clinical and demographic characteristics of these patients are summarized in Table 1. In addition to extending the phenomenon of neuroleptic hypersensitivity to other dementing diseases, these cases suggest that neuroleptic hypersensitivity could be an early manifestation of a developing neurodegenerative dementia that includes loss of dopaminergic neurons. Furthermore, magnetic resonance imaging (MRI) studies may suggest this susceptibility by revealing attenuation of the pars compacta of the substantia nigra in the midbrain.7,8
CASE REPORTS
Patient 1. A 62-year-old woman with a prior diagnosis of FTD was hospitalized secondary to severe motor rigidity, delirium, dehydration, and aspiration pneumonia. The patient had a long psychiatric history of schizoaffective psychosis, with disorganized thinking and frequent spells characterized as manic. She had received antipsychotic medications for decades, chiefly haloperidol and trifluoperazine. A week prior to admission, she had had an increase in the dosage of her long-standing trifluoperazine to 20 mg and had started to develop confusion and greater extrapyramidal rigidity.
About one and a half years previously, she first manifested extrapyramidal rigidity and personality and behavioral changes. There had been no change in her antipsychotic or other medications at the time of emergence of extrapyramidal symptoms. In addition, the patient had been on high doses of antipsychotics in the past, including 6 months on trifluoperazine 10 mg bid, without extrapyramidal signs. An evaluation at that time disclosed progressive aspontaneity and decreased goal-directed behaviors consistent with FTD. Her past medical history was otherwise negative. Her family history revealed a sister and a niece with psychotic disorders.
On examination, the patient appeared acutely ill, with hypotension (blood pressure 85/53) and a temperature of 102.4 degrees. She had limited spontaneous speech and facial expression. She did not respond to commands, although voluntary movement was observed in all four limbs. Her neurological examination disclosed diffusely increased extrapyramidal tone with tremulousness of the upper extremities. Laboratory assessment revealed sodium 178, blood urea nitrogen 113, creatinine 4.3, leukocytes 17,600 (86% polymorphonuclear leukocytes), and initial creatine phosphokinase (CPK) of 1,644 IU. In addition to her pneumonia, the patient was considered to have NMS.
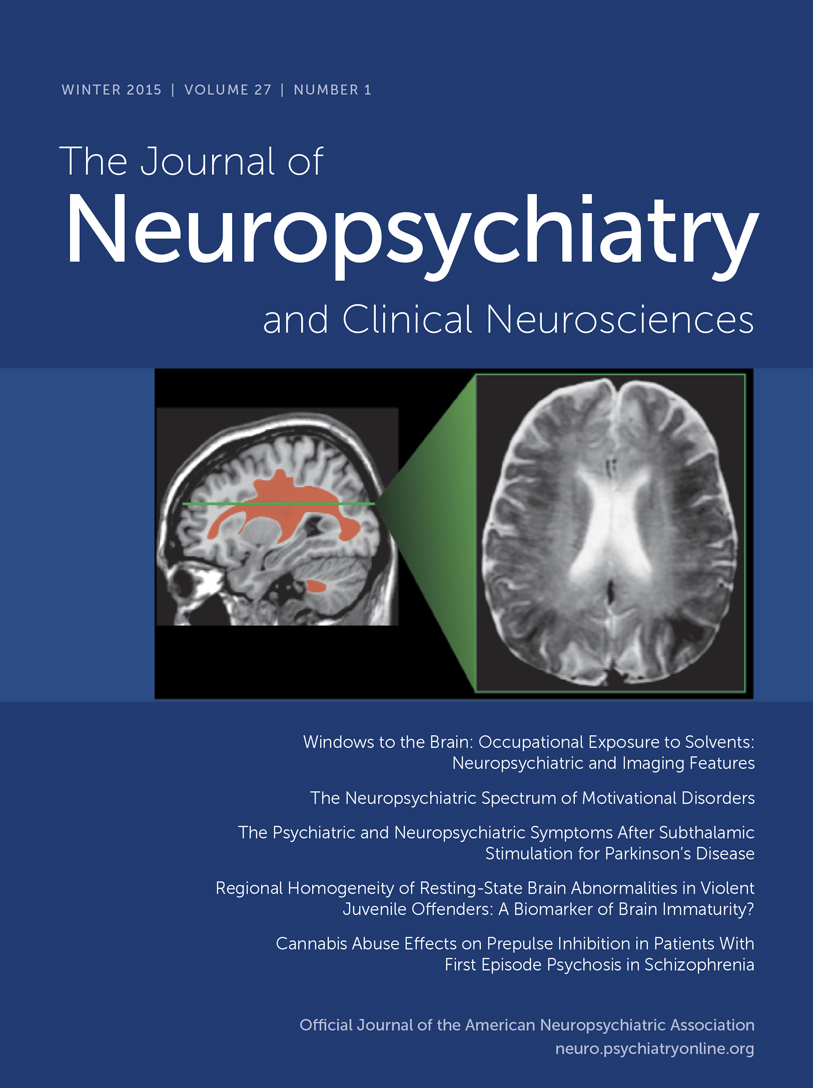
The patient gradually recovered during her hospitalization. Her extrapyramidal rigidity entirely resolved after discontinuation of the trifluoperazine. She did not receive antiparkinsonian medications. Despite resolution of her movement disorder, she continued to manifest decreased verbal and spontaneous behavior and a dysexecutive syndrome. During the course of her illness, she manifested hyperoral behavior and a tendency to explore with her hands, behaviors consistent with the Klüver-Bucy syndrome. Although her neuroimaging changes were not entirely typical, both MRI and positron emission tomography (PET) imaging suggested FTD (Figure 1A and Figure 2A). Moreover, she had changes in the pars compacta on MRI observed in some patients with Parkinson's disease (Figure 3B). The presence of motor neuron disease (MND) was considered, but was not seen on an electromyogram (EMG).
Patient 2. A 58-year-old man was hospitalized because of dementia and inability to care for himself. He had a long-standing history of either manic-depressive illness or schizoaffective psychosis and had recently developed neuroleptic hypersensitivity and a frontally predominant dementia. His psychiatric illness included multiple manic episodes and periods of depression with psychotic symptomatology treated with lithium, divalproex, and a range of antipsychotic medications. The patient had been on antipsychotic drugs for the majority of the prior 15 years, including chlorpromazine, thioridazine, haloperidol, and clozapine. The patient's past medical history also included poorly controlled diabetes, periods of heavy ethanol abuse, and prostate cancer of limited involvement treated conservatively. The family history did not disclose any specific or familial illnesses.
One year prior to hospitalization, while on haloperidol, he became very rigid and “parkinsonian,” mute, and unresponsive. There had been no change in his neuroleptic treatment, ongoing haloperidol dosage, or other medications. The assessment at that time showed a markedly elevated tone, slight temperature elevations, and orthostatic hypotension, but his CPK did not rise above 200 IU. These symptoms resolved after discontinuation of the haloperidol. After that episode, however, it became clear that the patient had a behavioral change with disinhibition and a progressive cognitive decline. His executive skills and memory were impaired, and his ability to perform activities of daily living had declined.
On the current hospitalization one year off of neuroleptics, he was alert and oriented to time and place but tended to sit and stare with little spontaneous verbal output. Mental status testing disclosed deficits in verbal memory and learning, decreased verbal fluency, poor visuospatial skills, and deficits on frontal-executive tasks. The neurological examination was unremarkable except for mild increased tone bilaterally and a decreased gait.
The patient underwent a dementia evaluation. He was initially suspected of having normal pressure hydrocephalus because of large ventricles and a suspicious cysternogram; however, ventriculoperitoneal shunt placement did not alter his clinical symptoms or progression. He was then suspected of having a form of FTD with MND because of disinhibited behavior, personality change, and swallowing difficulty; however, an EMG did not disclose MND. Review of his MRI suggested predominant frontal atrophy and possible changes in the substantia nigra region (Figure 1B and Figure 3C). A PET scan disclosed hypometabolism in the frontal and temporal regions with some involvement of parietal regions; however, the scan was suboptimal because of movement (see Figure 2). Subsequently, the patient continued to show hypersensitivity to reintroduction of antipsychotic drugs and was maintained on valproate alone.
Patient 3. A 61-year-old man with a long history of schizoaffective disorder was hospitalized because he had developed dysphagia, fasciculations, and an aspiration pneumonia. For at least 6 months the patient had experienced progressive swallowing difficulty, culminating in respiratory difficulty and a productive cough. Three years previously, the patient had received the diagnosis of dementia with progressive disengagement and apathy.
The patient had a 30-year history of a chronic affective psychosis and had been on a range of antipsychotic drugs for the majority of that time. He had received chlorpromazine, trifluoperazine, and risperidone as well as lithium. Three years previously he had developed severe parkinsonism while on at least a 3-month unchanged dosage of trifluoperazine and lithium. There had not been any changes in any other medications or dosages. His parkinsonism included cogwheel rigidity, hypomimia, and decreased verbal output. He was initially thought to have Parkinson's disease, but a brief trial of levodopa/carbidopa failed to improve his extrapyramidal symptoms. Most of these symptoms, however, resolved on discontinuation of the antipsychotic medication. Further evaluation disclosed a progressive language impairment with onset coincident with his extrapyramidal reaction. He had a decline in verbal output as well as a decrease in reading and writing ability, and mental status testing revealed declines in verbal memory and in executive functions.
Examination on this hospitalization revealed progression of his dementia, with limited verbal output and decreased spontaneous interaction. On neurological examination, he had difficulty protruding his tongue, fine and gross fasciculation in the upper extremities, slight increased tone, and brisk reflexes. His EMG confirmed the presence of MND. Review of his MRI suggested frontotemporal atrophy and smudging of the pars compacta towards the red nucleus on T2-weighted images (Figure 1C and Figure 3D).
This patient had a protracted course with partial recovery. He received the diagnosis of FTD with MND and was started on riluzole 50 mg q12h. His parkinsonism was mild when he was off of any antipsychotic medication. The patient was eventually transferred to a chronic care facility.
Patient 4. A 65-year-old woman with a 3- to 4-year history of dementia and a nearly 30-year history of manic-depressive illness presented for further diagnostic assessment of her dementia. Past medical history included manic episodes and periods of profound depression previously managed with lithium. Family history disclosed that her mother had died with an unspecified dementing illness and her brother had schizophrenia.
Five years previously, the patient had developed an extrapyramidal reaction to haloperidol. At that time, she had been on various antipsychotic medications as well as lithium or divalproex for most of the prior 20 to 30 years, particularly thiothixene (up to 30 mg/day) and haloperidol. The specific medication and dosage had not been changed at the time she developed neuroleptic hypersensitivity. She developed severe rigidity and muteness, but no clear fever, elevation of CPK levels, or other evidence of NMS. Discontinuation of the haloperidol resulted in resolution of her extrapyramidal rigidity without necessitating a trial of antiparkinsonian medications. Nearly coincident with this reaction, her family noted a decline in her speech and language and changes in her personality. She became unable to complete goal-oriented behaviors and developed new compulsive behaviors, including hoarding rolls of toilet paper.
She was reevaluated 5 years after her neuroleptic reaction and after the onset of her dementia. The patients had limited spontaneous interaction. Her speech was strained and dysarthric, and there were paraphasic errors on verbal output and paralexic errors on writing. On further testing of her writing she had prominent errors in grammatical and sentence structure. Memory and simple calculations appeared intact. The patient could do simple constructions but had difficulty with the planning and organization of complex figures. She had perseverations on Luria motor sequencing tasks and was very concrete in interpreting proverbs. The neurological examination was abnormal because of dysarthria, mild leadpipe rigidity bilaterally, and palmomental reflexes.
The clinical diagnosis was probable FTD with primary progressive aphasia. She had a frontally predominant dementia syndrome with a decline in verbal output, speech, and language. Neuropsychological testing confirmed the presence of marked impairment in verbal fluency and cognitive flexibility along with milder impairments in verbal memory and visuospatial skills. Her MRI scan performed elsewhere suggested greater frontotemporal atrophy; the imaging was not assessed for midbrain changes. PET imaging showed hypometabolism in the bilateral frontoparietal and right superior temporal regions (Figure 2B). Her symptoms were eventually managed with sertraline 100 mg bid and low-dose olanzapine (2.5 mg qd).
Patient 5. A 54-year-old man with schizoaffective disorder had a history of several episodes of severe extrapyramidal rigidity during the preceding 5 years. His physicians had not been able to distinguish between the development of Parkinson's disease and the possible contribution of his chronic antipsychotic drug therapy. Antipsychotic medications were taken for most of his adult life and included haloperidol (oral and decanoate), prolixin (oral and decanoate), chlorpromazine, thioridazine, thiothixene, clozapine, and risperidone. Prior to age 49, the patient had not experienced neuroleptic sensitivity even on high doses of these medications. Trials of levodopa/carbidopa and amantadine had not improved his extrapyramidal symptoms.
The patient's medical history was also significant for a cognitive decline. During the prior one or more years he had developed progressive deficits in memory, verbal fluency, and executive functions. These cognitive changes were superimposed on his chronic psychosis with affective and paranoid features, delusions of grandeur, hyperreligiosity, euphoria, and disorganized speech. Family history was positive for dementia in a brother and schizophrenia in a cousin.
The patient was hospitalized because of a severe rigidity, delirium, mutism, dehydration, and respiratory difficulties on olanzapine 10 mg qd. On examination, he was rigid and unresponsive. He was also febrile, dehydrated, hypotensive, dysphagic, and had an aspiration pneumonia. He had little spontaneous verbal output or behavior and was unable to communicate or follow instructions. He could make sounds that he clearly intended as meaningful, but they were indecipherable. Neurological examination disclosed masked faces, absent gag reflex, and extreme motor rigidity. On admission his CPK was elevated at 454. The patient was treated with tracheostomy, respiratory and intensive care support, rehydration, discontinuation of his antipsychotic medication, and a period of antibiotics and bromocriptine. He gradually resolved from his delirium, extreme rigidity, and other NMS symptoms but remained with dementia.
The diagnosis was FTD with extreme sensitivity to antipsychotic agents, including NMS to olanzapine. MRI scans were remarkable for frontotemporal atrophy and suggestive abnormalities in the pars compacta of the substantia nigra (Figure 1D and Figure 3E). A subsequent EMG did not reveal evidence of MND.
DISCUSSION
Five patients with bipolar disease or a schizoaffective disorder developed new and severe sensitivity to antipsychotic medications. Previously, these patients had had decades of chronic treatment with antipsychotic drugs without evidence of hypersensitivity. They were on a stable dose with no alterations in the remainder of their drug regimens at the time of development of their extrapyramidal syndromes. Their reactions involved the typical antipsychotics and, in one case, olanzapine, and ranged from extrapyramidal rigidity to NMS. Nearly coincident with these reactions, the patients developed progressive cognitive and behavioral declines. All five patients had frontal-executive dysfunction, one had “primary progressive aphasia” and new-onset compulsive behaviors, one had Klüver-Bucy symptoms, and another had MND, all of which are clinical correlates of FTD. The occurrence of emergent neuroleptic sensitivity appeared to correspond to the development of a neurodegenerative dementia with features consistent with the broad spectrum of FTD.
Neuroleptic hypersensitivity including NMS is a feature of dementia with Lewy bodies.3,9 DLB is a common cause of dementia characterized by histological presence of distinctive inclusions within neurons or Lewy bodies.9 Hypersensitivity to typical neuroleptics and the newer antipsychotics may range from extrapyramidal rigidity to partial or forme fruste NMS or the entire NMS with severe rigidity, delirium, fever, muteness or hypophonia, autonomic changes, elevated white count, and CPK levels greater than 300 IU.10 NMS usually occurs on initiation or increase of antipsychotic medications, but this was evident in only one of our patients (Patient 1).
Some investigations have recommended neuroleptic hypersensitivity as a diagnostic feature of DLB.2 The patients reported here, however, did not meet clinical criteria for DLB.11 They did not have significant parkinsonism off of their neuroleptic medications, nor did they manifest a fluctuating mental status with visual hallucinations. Moreover, they were younger than the typical DLB patient, and their examinations suggested frontally predominant dementias with ages of onset in the presenium. Their functional imaging showed predominant anterior hypometabolism consistent with FTD rather than the predominant posterior hypometabolism consistent with DLB.1,4,9 Ultimately, only pathological confirmation will confirm the absence of DLB; however, in the wide spectrum of FTD, some hereditary forms have been reported with cortical Lewy bodies as well as depleted neurons in the substantia nigra.12
The mechanism for neuroleptic hypersensitivity in dementia probably involves compromise of the nigrostriatial dopamine system. In DLB, there is loss of substantia nigra neurons, as well as decreased dopamine and dopamine uptake sites in caudal putamen.13 The extreme sensitivity to dopaminergic blockade may relate to a 60 to 70 percent reduction in dopaminergic neurons in the substantia nigra and a failure to upregulate the striatal dopamine D2 postsynaptic receptors in response to antipsychotic medications.14 The patients reported here may have a disorder in the FTD spectrum but also characterized by striatal D2 depletion and inability to upregulate these dopamine receptors similar to DLB. This mechanism is further suggested by their MRI scans. The band of high intensity normally separating the substantia nigra from the red nucleus appeared decreased in size, a finding that has suggested increased atrophy of the substantia nigra in patients with Parkinson's disease or other parkinsonian syndromes.7,8 Although the value of this radiologic finding is debated, it is not known to occur in most patients with neuroleptic sensitivity. It could suggest a potential marker for neuroleptic sensitivity in patients at risk because of depletion of dopaminergic neurons.
The dementing illnesses in these five patients fall within the FTD spectrum. FTD is a heterogeneous group of degenerative disorders that overlap in clinical and neuropathological findings.6,15 Patients with FTD have frontal personality alterations, compulsive or repetitive behaviors, a decline in frontal executive abilities, possible progressive aphasia, and elements of the Klüver-Bucy syndrome (the compulsion to attend to visual stimuli, hyperorality, hypersexuality, visual agnosia, and placidity).5,6,16,17 Approximately 20 percent of FTD patients have Pick bodies on pathology consistent with Pick's disease, another 10 percent have accompanying MND, and a small percentage have parkinsonism and an abnormal gene on chromosome 17.5,6,18,19 Several FTD syndromes with parkinsonism have an abnormality of chromosome 17,18 including pallidopontonigral degeneration,20 hereditary dysphasic disinhibition syndrome,21 and disinhibition-dementia-parkinsonism-amyotrophy complex.22,23 Other autosomal dominant variants exist in the literature with features including rapidly progressive frontal dementia, parkinsonism, hypotension, neuronal loss in the substantia nigra, possible MND, and even possible cortical Lewy bodies.12,24 These varied FTD spectrum disorders may have in common hyperphosphorolated tau deposits within glial cells and neurons, or “tauopathies.”19,25–28 The patients reported here probably had a disorder consistent with the FTD spectrum, with added neuroleptic hypersensitivity unmasking an underlying dopaminergic deficiency.
The potential association of affective psychosis with FTD is unclear. Other factors could contribute to emergence of dementia in the course of a long history of affective disorder; however, no other factors except dementia were documented in these cases. There is scant information about the number of affective psychotics who progress to FTD; however, depression or psychosis can be a prelude to FTD,15,18 and there could be a shared genetic susceptibility underlying both diseases. Both FTD and manic-depressive illness are strongly genetic disorders.15,29–30 The affective psychosis preceding the dementia in these patients could indicate that FTD can be a lifelong syndrome initially presenting with psychiatric symptomatology—somewhat analogous to Huntington's disease, which can manifest depression or bipolar symptoms years before the onset of choreoathetosis or cognitive difficulties.31,32
These patients with premorbid mood psychoses developed neuroleptic hypersensitivity and a dementing illness consistent with FTD spectrum disorders. Their cases suggest that neuroleptic hypersensitivity is not confined to DLB, but rather is more pervasive in dementing diseases. The antipsychotics may have unmasked a preexisting dopamine deficiency that would have become symptomatic. This is a retrospective clinical report, and these patients should be investigated further, particularly with fluorodopa PET imaging and with newer genetic testing for linkage to chromosome 17. Further research should evaluate the mechanisms of neuroleptic sensitivity in FTD and other dementias, as well as the value of MRI imaging of the substantia nigra in predicting this predisposition.
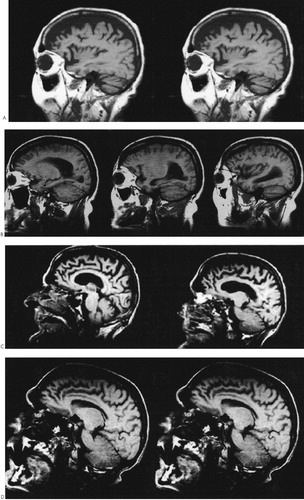
FIGURE 1. Magnetic resonance images: sagittal T1-weighted images demonstrating predominant frontal atrophy in Patient 1 (A), Patient 2 (B), Patient 3 (C), and Patient 5 (D)Patient 3 also had a significant amount of generalized cerebral atrophy. Magnetic resonance images: sagittal T1-weighted images demonstrating predominant frontal atrophy in Patient 1 (A), Patient 2 (B), Patient 3 (C), and Patient 5 (D). Patient 3 also had a significant amount of generalized cerebral atrophy.
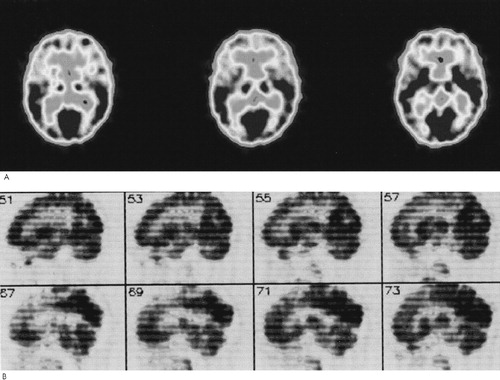
FIGURE 2. Positron emission tomography images: representative samples of 18-fluorodeoxyglucose resting PET scans for Patient 1 (A) and Patient 4 (B)The PET scans show disproportionate frontal hypometabolism.
FIGURE 3. Magnetic resonance images: T2-weighted images of the midbrain in the area of the substantia nigra and red nucleusFigure A is a normal image for comparison. It shows the relatively high intensity normally separating the substantia nigra and the red nucleus. The patients' images suggest a “smudging” of this distinction, particularly in the pars compacta bordering the tegmentum. The scans correspond to Patient 1 (B), Patient 2 (C), Patient 3 (D), and Patient 5 (E).
 |
1 Mendez MF, Cummings JL: Dementia and Alzheimer's disease, in Prognosis of Neurological Disorders, 2nd edition, edited by Evans RW, Baskin DS, Yatsu FM, et al. New York, Oxford University Press, 2000, pp 571-592Google Scholar
2 McKeith I, Fairbairn A, Perry R, et al: Neuroleptic sensitivity in patients with senile dementia of Lewy body type. British Medical Journal 1992; 305:673-678Crossref, Medline, Google Scholar
3 Rojas-Fernandez CH, MacKnight C: Dementia with Lewy bodies: review and pharmacotherapeutic implications. Pharmacotherapy 1999; 19:795-803Crossref, Medline, Google Scholar
4 Burke WJ, Pfeiffer RF, McComb RD: Neuroleptic sensitivity to clozapine in dementia with Lewy bodies. J Neuropsychiatry Clin Neurosci 1998; 10:227-229Link, Google Scholar
5 The Lund and Manchester Groups: Clinical and neuropathological criteria for frontotemporal dementia. J Neurol Neurosurg Psychiatry 1994; 57:416-418Crossref, Medline, Google Scholar
6 Gustafson L: Clinical picture of frontal lobe degeneration of non-Alzheimer type. Dementia 1993; 4:143-148Medline, Google Scholar
7 Duguid JR, De La Paz R, De Groot J: Magnetic resonance imaging of the midbrain in Parkinson's disease. Ann Neurol 1986; 20:744-747Crossref, Medline, Google Scholar
8 Braffman BH, Grossman RI, Goldberg HI, et al: MR imaging of Parkinson's disease with spin-echo and gradient-echo sequences. Am J Neuroradiol 1988; 9:1093-1099Google Scholar
9 Forstl H: The Lewy body variant of Alzheimer's disease: clinical, pathophysiological and conceptual issues. Eur Arch Psychiatry Clin Neurosci 1999; 249(suppl 3):64-67Google Scholar
10 Hasan S, Buckley P: Novel antipsychotics and the neuroleptic malignant syndrome: a review and critique. Am J Psychiatry 1998; 155:1113-1116Google Scholar
11 McKeith IG, Ballard CG, Perry RH, et al: Prospective validation of consensus criteria for the diagnosis of dementia with Lewy bodies. Neurology 2000; 54:1050-1058Google Scholar
12 Muenter MD, Forno LS, Hornykiewicz O, et al: Hereditary form of parkinsonism-dementia. Ann Neurol 1998; 43:768-781Crossref, Medline, Google Scholar
13 Piggott MA, Marshall EF, Thomas N, et al: Striatal dopaminergic markers in dementia with Lewy bodies, Alzheimer's and Parkinson's diseases: rostrocaudal distribution. Brain 1999; 122:1449-1468Google Scholar
14 Piggott MA, Perry EK, Marshall EF, et al: Nigrostriatal dopaminergic activities in dementia with Lewy bodies in relation to neuroleptic sensitivity: comparisons with Parkinson's disease. Biol Psychiatry 1998; 44:765-774Crossref, Medline, Google Scholar
15 Chow TW, Miller BL, Hayashi VN, et al: Inheritance of frontotemporal dementia. Arch Neurol 1999; 56:817-822Crossref, Medline, Google Scholar
16 Mendez MF, Selwood A, Mastri AR, et al: Pick's disease versus Alzheimer's disease: a comparison of clinical characteristics. Neurology 1993; 43:289-292Crossref, Medline, Google Scholar
17 Lilly R, Cummings JL, Benson DF, et al: The human Klüver-Bucy syndrome. Neurology 1983; 33:1141-1145Google Scholar
18 Foster NL, Wilhelmsen K, Sima AA, et al: Frontotemporal dementia and parkinsonism linked to chromosome 17: a consensus conference. Ann Neurol 1997; 41:706-715Crossref, Medline, Google Scholar
19 Spillantini MG, Bird TD, Ghetti B: Frontotemporal dementia and parkinsonism linked to chromosome 17: a new group of tauopathies. Brain Pathol 1998; 8:387-402Crossref, Medline, Google Scholar
20 Reed LA, Schmidt ML, Wszolek ZK, et al: The neuropathology of a chromosome 17-linked autosomal dominant parkinsonism and dementia (“pallido-ponto-nigral degeneration”). J Neuropathol Exp Neurol 1998; 57:588-601Crossref, Medline, Google Scholar
21 Lendon CL, Lynch T, Norton J, et al: Hereditary dysphasic disinhibition dementia: a frontotemporal dementia linked to 17q21-22. Neurology 1998; 50:1546-1555Google Scholar
22 Wilhelmsen KC: Disinhibition-dementia-parkinsonism-amyotrophy complex (DDPAC) is a non-Alzheimer's frontotemporal dementia. J Neural Transm Suppl 1997; 49:269-275Medline, Google Scholar
23 Basun H, Almkvist O, Axelman K, et al: Clinical characteristics of a chromosome 17-linked rapidly progressive familial frontotemporal dementia. Arch Neurol 1997; 54:539-544Crossref, Medline, Google Scholar
24 Gilbert JJ, Kish SJ, Chang LJ, et al: Dementia, parkinsonism, and motor neuron disease: neurochemical and neuropathological correlates. Ann Neurol 1988; 24:688-691Crossref, Medline, Google Scholar
25 Hulette CM, Pericak-Vance MA, Roses AD, et al: Neuropathological features of frontotemporal dementia and parkinsonism linked to chromosome 17q21-22 (FTDP-17): Duke Family 1684. J Neuropathol Exp Neurol 1999; 58:859-866Crossref, Medline, Google Scholar
26 Nasreddine ZS, Loginov M, Clark LN, et al: From genotype to phenotype: a clinical pathological, and biochemical investigation of frontotemporal dementia and parkinsonism (FTDP-17) caused by the P301L tau mutation. Ann Neurol 1999; 45:704-715Crossref, Medline, Google Scholar
27 Hong M, Zhukareva V, Vogelsberg-Ragaglia V, et al: Mutation-specific functional impairments in distinct tau isoforms of hereditary FTDP-17. Science 1998; 282:1914-1917Google Scholar
28 Mirra SS, Murrell JR, Gearing M, et al: Tau pathology in a family with dementia and a P301L mutation in tau. J Neuropathol Exp Neurol 1999; 58:335-345Crossref, Medline, Google Scholar
29 Stevens M, van Duijn CM, Kamphorst W, et al: Familial aggregation in frontotemporal dementia. Neurology 1998; 50:1541-1545Google Scholar
30 Kessing LV, Olsen EW, Mostensen PB, et al: Dementia in affective disorder: a case-register study. Acta Psychiatr Scand 1999; 100:176-185Crossref, Medline, Google Scholar
31 Fahim S, van Duijn CM, Baker FM, et al: A study of familial aggegration of depression, dementia and Parkinson's disease. Eur J Epidemiol 1998; 14:233-238Crossref, Medline, Google Scholar
32 Folstein SE: Huntington's Disease: A Disorder of Families. Baltimore, Johns Hopkins University Press, 1989Google Scholar