Effects of Depression on Working Memory in Presymptomatic Huntington's Disease
Abstract
Cognitive decline may precede motor symptoms in Huntington's disease (HD). Depression is common in HD and has also been linked with cognitive impairment. The contribution of depression to cognition in individuals presymptomatic for HD (N=15) was investigated. Tests from the Cambridge Automated Neuropsychological Assessment Battery measured visual and working memory. Depression was assessed with the Beck Depression Inventory and the Unified Huntington's Disease Rating Scale. Depressed mood and estimated time to disease onset, calculated by using DNA mutation length, both were significant predictors of working memory performance. Findings are consistent with and contribute to existing research with individuals presymptomatic for HD, identifying a potentially remediable contribution to cognitive decline (i.e., depressed mood).
Huntington's disease (HD) is an autosomally dominant terminal illness characterized by a gradual deterioration in motor, cognitive, and emotional functioning. The disease is caused by an abnormal number of repeats of the trinucleotide sequence CAG in the gene IT15 on chromosome four. Individuals with more than 39 CAG repeats will develop HD. The symptoms of this illness typically present in middle adulthood.1
HD is not clinically diagnosed until the presence of abnormal motor symptoms is noted on neurological exam. Despite some mixed findings,2–4 there is a growing body of research suggesting that cognitive decline may precede the onset of motor symptoms.5–9 Recent studies have found links between cognitive decline and genetic data. For example, presymptomatic gene carriers showed deficits in delayed and immediate recall in verbal memory tasks of the Wechsler Memory Scale (WMS).10 Individuals showing impaired performance on subtests of the WMS had significantly longer CAG repeats than those who did not show impairments. On the basis of these findings, it was inferred that individuals who are closer to onset (i.e., have a greater number of repeats) were more cognitively impaired than individuals further from onset.
Individuals who are presymptomatic but known to have the gene mutation also showed deficits in general intelligence tests, memory, and language tasks.11 Again, CAG repeat length was correlated with cognitive test performance, and individuals with more repeats scored lower than individuals with fewer repeats. Deficits in attentional set-shifting and semantic fluency in individuals who were presymptomatic for HD also have been reported, although no significant correlation was established between CAG repeat length and cognitive performance.12 This latter finding may have been due to the small sample size and restricted range of repeat lengths.
Depression is estimated to occur in 9% to 63% of individuals with HD and may precede the onset of motor symptoms by 2 to 20 years.13,14 Depression is associated with changes in cognitive abilities. For example, research participants diagnosed with major depressive disorder scored significantly lower than a nonpatient control group on a visual memory task.15 Individuals with major depressive disorder also scored significantly lower than an age- and IQ-matched group of control subjects in the areas of verbal fluency, visual memory tasks, spatial span tasks, working memory tasks, and tasks involving executive function.16 Findings regarding deficits in executive functions were replicated.17
In light of the literature concerning cognitive decline in HD, the high prevalence of depression in HD, and the association of cognitive decline with depression, questions arise concerning the impact of the depression on cognition in individuals who are presymptomatic for HD. This is a critical issue to address because depression is a potentially treatable condition that may exacerbate cognitive decline in HD. The present study examined the effect of depression on the cognitive performances of individuals presymptomatic for HD.
METHODS
Subjects
Individuals who carried the expanded CAG gene but who were presymptomatic for HD (e.g., were not showing motor signs) were recruited from the University of Iowa Huntington's Disease Center of Excellence and the University of California–San Diego. Participants (N=15) were predominantly female (66.7%) and Caucasian (86.7%). Participants were an average of 40.51 years old (SD=10.67) and averaged 14.8 years of education (SD=2.08). Estimated age of onset was determined with an equation using CAG repeat length and age of HD onset in affected parent: age of onset=[– 0.81×repeat length]+[0.51×parental onset age]+54.87.18 The estimate of years to onset was calculated by subtracting current age from this estimated age of onset.
Procedure
After having the procedure explained to them and giving informed consent, participants were administered three tests from the Cambridge Automated Neuropsychological Assessment Battery (CANTAB),19 conducted on a computer equipped with a touch-sensitive monitor. Participants were seated a comfortable distance in front of the computer. To acquaint the participants with the CANTAB program, they participated in a motor speed task in which they were asked to touch the cross point of ten flashing crosses. Responses for all tests were made using the index finger of the dominant hand. Participants were also interviewed with the Unified Huntington's Disease Rating Scale (UHDRS)20 and completed the Beck Depression Inventory (BDI).21
Measures
Two tasks from the CANTAB measured visual memory. The pattern recognition test begins with the presentation of 12 unique patterns that participants are asked to remember. Following presentation of the patterns, participants are shown two patterns and asked to touch the pattern that they were previously shown. The spatial recognition test begins with the presentation of five white squares, which appear at different locations on the screen. Participants are asked to remember the locations in which the squares appear. After the presentation of all five squares, the participants are shown a pair of squares, one in a previously viewed location and the other in a new location. Individuals are asked to touch the box that appears in the location that was previously seen. This process is repeated three times, with presentations in new locations with each round.
The spatial span test of the CANTAB assesses the participant's working memory. Throughout this task, nine white blocks are presented on the computer screen. The boxes change color one by one and participants are asked to remember the order in which they change color. Initially two boxes change color, and if the participant successfully touches the boxes in the correct order, one more box changes color in the next round. The task continues until the participant successfully completes the highest level (all nine boxes change color) or makes three consecutive errors on the same level.
The UHDRS is a standardized clinical rating scale assessing four components of HD: motor function, cognition, behavior, and functional abilities. Participants were interviewed by an experimenter, who made the final ratings. For this study, information regarding the severity and frequency of depressed mood over the preceding month was used. Frequency ratings range from 0 (never or almost never) to 4 (very frequently, most all the time). Severity ratings range from 0 (no mood disturbance) to 4 (severe mood disturbance, significant suffering and loss of functioning). The UHDRS depression score is calculated by multiplying the frequency and severity ratings for depressed mood.
The BDI is a 21-item self-report questionnaire that measures symptoms of depression over the past week. The statements are rated on a scale from 0 to 3, and these ratings are summed to form a BDI total score.
RESULTS
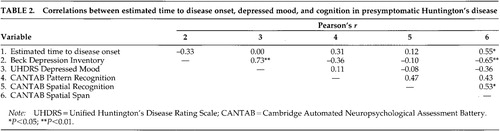
Descriptive information concerning the participants appears in Table 1. There was a negative value for time to estimated disease onset because the equation used to calculate this variable is merely an approximation. CANTAB scores reported in this study are standard scores based on age-corrected norms. Distributions of the two depression measures were skewed; consequently, scores from the BDI and UHDRS were standardized.
Pearson's correlations between the depression, cognitive, and time to estimated disease onset measures are shown in Table 2. Spatial span standard score was significantly correlated negatively with BDI total score (P<0.05) and positively with time to estimated disease onset (P<0.05). There was a significant correlation between the standard scores for spatial recognition and spatial span (P<0.05). A significant correlation also was found between the two depression measures (P<0.01).
A multiple regression analysis was conducted to determine how well depression and time to estimated disease onset predicted spatial span standard scores. An aggregated measure of the two depression scores was used in this analysis because of their high degree of overlap and because aggregate measures are more reliable.22 The overall regression equation was significant (F=11.607, df=2,11, P<0.01). Both depression and time to estimated disease onset were significant (P<0.05) predictors of the spatial span standard score.
DISCUSSION
Cognitive decline was associated with less time to estimated disease onset and with increased levels of depression. These findings are consistent with previous research indicating that cognitive decline in HD that precedes motor symptoms is associated with time to disease onset.10,11 Our findings are also consistent with studies that reported links between depression and cognitive impairment.15,16
Impairments in working memory were associated with less estimated time to disease onset and with increased depressed mood. Impaired performance on tasks of working memory has been attributed to impairment in the frontal lobe or a disruption of the frontal-striatal circuitry connecting the frontal lobe to the basal ganglia. These impairments are consistent with the known neuropathological changes that occur in HD.23 Specifically, neuronal loss and gliosis occur predominantly in the caudate and putamen, disrupting frontal-striatal circuitry. The findings suggesting frontal-striatal dysfunction (i.e., impaired working memory) also are consistent with evidence suggesting that depression in HD is associated with hypometabolism in the thalamus and inferior frontal cortex.24
Impairments in visual memory were not significantly associated with disease or depression measures in the present study. This finding was unexpected, since previous investigators had reported memory impairments in individuals presymptomatic for HD.10,11 The memory tasks used in the current study may not have been sensitive enough to detect the subtle changes that are probably characteristic of presymptomatic cognitive decline in HD. However, few previous investigations have compared types of memory tests to determine which aspects of memory are sensitive to early HD. Findings from this study suggest that measures of working memory, but not measures of consolidation and storage, may be the most sensitive to early changes in the basal ganglia.
Limitations of the current project arise from the cross-sectional study design, which precludes determination of the developmental relationship of depressed mood, time to disease onset, and cognitive decline. Additionally, calculation of the time to disease onset relied on an imperfect estimate, as reflected in the negative value obtained for time to onset in one presymptomatic individual. Finally, the samples sizes in the current study are low. These findings require replication with larger samples of presymptomatic individuals.
Despite these limitations, the findings are important, as they indicate that both depression and estimated time to disease onset of HD affect cognitive performance. This is a critical finding because while there is no effective treatment for HD, there are effective treatments for depression. The early cognitive changes in Huntington's disease may be exacerbated by or partially attributable to depression in some individuals. Therefore it may be very important to treat depression in presymptomatic HD, because alleviation of depressed mood might result in improved cognitive performance.
Improved understanding of the cause (or causes) of depressed mood in HD is critical to developing effective treatments. Many questions remain concerning the etiology of depression in individuals with HD. Depression could be a psychological reaction to knowledge about an impending terminal illness; this is unlikely, however, since there was no significant association of depression with estimated time to onset in the present sample. Alternatively, depression could be a response to other factors in participants' lives, such as the declining health or the death of a parent affected with HD. Still another possibility is that depression could result from pathological changes in the brain associated with Huntington's disease.
ACKNOWLEDGMENTS
This study was supported by National Institute of Mental Health (NIMH) Grants 5R29 MH55331-05 and 1K02 MH01579-01, National Institute of Neurological Disorders and Stroke Grant PO410951-G, a Howard Hughes Medical Institute Pilot Grant, and a Carver Medical Research Initiative Grant Award to J.S.P.; a National Institutes of Health/ National Institute on Aging predoctoral fellowship (T32 AG00214) to R.E.R.; and NIMH Grant R03 MH59430-01 to J.M.H.
 |
 |
1 Paulsen JS, Robinson RG: Huntington's disease, in Early-Onset Dementia, edited by Hodges J. Cambridge, UK, Cambridge University Press (in press)Google Scholar
2 de Boo GM, Tibben A, Lanser JBK, et al: Early cognitive and motor symptoms in identified carriers of the gene for Huntington disease. Arch Neurol 1997; 54:1353-1357Google Scholar
3 Giodani B, Berent S, Boivin MJ, et al: Longitudinal neuropsychological and genetic linkage analysis of persons at risk for Huntington's disease. Arch Neurol 1995; 52:59-64Crossref, Medline, Google Scholar
4 Strauss ME, Brandt J: Are there neuropsychologic manifestations of the gene for Huntington's disease in asymptomatic, at-risk individuals? Arch Neurol 1990; 47:905-908Crossref, Medline, Google Scholar
5 Campodonico JR, Codori AM, Brandt J: Neuropsychological stability over two years in asymptomatic carriers of the Huntington's disease mutation. J Neurol Neurosurg Psychiatry 1996; 61:621-624Crossref, Medline, Google Scholar
6 Lyle OE, Gottesman II: Premorbid psychometric indicators of the gene of Huntington's disease. J Consult Clin Psychol 1977; 45:1011-1022Google Scholar
7 Diamond R, White RF, Myers RH, et al: Evidence of presymptomatic cognitive decline in Huntington's disease. J Clin Exp Neuropsychol 1992; 14:961-975Crossref, Medline, Google Scholar
8 Foroud T, Siemers E, Kleindorfer D, et al: Cognitive scores in carriers of Huntington's disease gene compared to noncarriers. Ann Neurol 1995; 37:657-664Crossref, Medline, Google Scholar
9 Kirkwood SC, Siemers E, Stout JC, et al: Longitudinal cognitive and motor changes among presymptomatic Huntington disease gene carriers. Arch Neurol 1999; 56:563-568Crossref, Medline, Google Scholar
10 Hahn-Barma V, Deweer B, Dürr A, et al: Are cognitive changes the first symptoms of Huntington's disease? A study of gene carriers. J Neurol Neurosurg Psychiatry 1998; 64:172-177Crossref, Medline, Google Scholar
11 Jason GW, Suchowersky O, Pajurkova EM, et al: Cognitive manifestations of Huntington disease in relation to genetic structure and clinical onset. Arch Neurol 1997; 54:1081-1088Google Scholar
12 Lawrence AD, Hodges JR, Rosser AE, et al: Evidence for specific cognitive deficits in preclinical Huntington's disease. Brain 1998; 121:1329-1341Google Scholar
13 Folstein SE, Franz ML, Jensen BA, et al: Conduct disorder and affective disorder among the offspring of patients with Huntington's disease. Psychol Med 1983; 13:45-52Crossref, Medline, Google Scholar
14 Morris M: Huntington's Disease. London, WB Saunders, Harper Press, 1991, pp 81-126Google Scholar
15 Shah PJ, O'Carroll RE, Rogers A: Abnormal response to negative feedback in depression. Psychol Med 1999; 29:63-72Crossref, Medline, Google Scholar
16 Elliot R, Sahakian BJ, McKay AP, et al: Neuropsychological impairments in unipolar depression: the influence of perceived failure on subsequent performance. Psychol Med 1996; 26:975-989Crossref, Medline, Google Scholar
17 Purcell R, Maruff P, Kyrios M, et al: Neuropsychological function in young patients with unipolar major depression. Psychol Med 1997; 27:1277-1285Google Scholar
18 Aylward EH, Codori A, Barta PE, et al: Basal ganglia volume and proximity to onset in presymptomatic Huntington disease. Arch Neurol 1996; 53:1293-1296Google Scholar
19 Fray PJ, Robbins TW, Sahakian BJ: Neuropsychiatric applications of CANTAB. Int J Geriatric Psychiatry 1996; 11:329-336Crossref, Google Scholar
20 Huntington Study Group: Unified Huntington's Disease Rating Scale: reliability and consistency. Mov Disord 1996; 11:136-142Crossref, Medline, Google Scholar
21 Beck AT, Ward CH, Mendelson M, et al: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561-571Crossref, Medline, Google Scholar
22 Rushton JP, Brainerd CJ, Pressley M: Behavioral development and construct validity: the principle of aggregation. Psychol Bull 1983; 94:8-38Crossref, Google Scholar
23 Vonsattel JP, Difiglia M: Huntington's disease. J Neuropathol Exp Neurol 1998; 57:369-384Crossref, Medline, Google Scholar
24 Mayberg HS, Starkstein SE, Peyser CE, et al: Paralimbic frontal lobe hypometabolism in depression associated with Huntington's disease. Neurology 1992; 42:1792-1797Google Scholar